Acceptability of Telepsychiatry to a Rural Population
Abstract
Sixty-seven residents of a rural Midwestern state were surveyed by telephone to determine which factors influence their willingness to receive mental health services through live, two-way audio and video transmission. Two-thirds of the survey respondents were willing to participate in telepsychiatry. Many expressed reluctance, however. They were concerned about maintaining confidentiality, and they perceived telepsychiatry as impersonal. Medicare enrollees and older survey respondents were less willing than younger respondents to endorse the use of telemedicine.
Telemedicine has the potential to improve health care delivery to rural residents (1,2), and clinical applications of telepsychiatry to rural populations have been described (3,4,5). However, the willingness to receive mental health services through telemedicine remains uncertain. Simpson and Simpson (6) showed that the perceptions, health status, and behavior of rural residents differ from those of their urban counterparts. We conducted a telephone survey to determine which factors may influence the willingness of rural residents to receive mental health services through live, two-way audio and video transmission.
Methods
Subjects
Subjects came from a rural region in eastern Iowa. To be eligible, a resident had to be 18 years or older and live in a rural county with a total population of less than 50,000. A stratified sampling scheme based on a percentage of the total county population was used: From 1 to 16 households were sampled in each county until a study sample of 200 subjects was achieved. Households were randomly selected from among each eligible hardwired—that is, noncellular—exchange. Cellular telephones were excluded because they potentially duplicated households sampled from the hardwired exchanges. Calls were made between 9 a.m. and 9 p.m. between February 7 and March 4, 1999.
Survey instrument
The survey instrument, which was developed by one of the authors (PR), consisted of seven general topics that included demographic information, access to health care services, satisfaction with the health system, health status, mental health status, adaptive coping, and willingness to participate in telepsychiatry or to recommend it to a friend. Most of the questions had been tested in other surveys of rural populations conducted by one of the authors (JER). Questions about satisfaction were drawn from a scale developed by Rand (7). Adaptive coping was measured using a short-form scale from a revised version of the COPE scale developed by Carver and associates (8).
The dependent variables in the survey were the willingness of respondents to receive mental health treatment via telepsychiatry themselves or to recommend it to friends. Subjects who were unwilling to use the service themselves were asked follow-up questions to elicit the reason.
Frequency distributions, means, and standard deviations were prepared for the variables included in the analysis. Chi square analyses were used for categorical variables. T tests were used for continuous responses, including the three scales. Analyses were conducted using SAS computer software.
Results
Sample description
Of the 202 persons contacted, 67, or 33 percent, agreed to participate in the survey. Their mean±SD age was 53.3±17.4 years. Survey responses related to demographics and access are summarized in Table 1.
The respondents had a mean±SD of 2±6.3 encounters with a family physician in the past six months, with a lower mean of 1.2±4 encounters with a medical specialist during the same period. More than four-fifths of the respondents (N=56) indicated that they had a personal provider they could go to if they needed medical care, and two, or 3 percent, had been hospitalized during the preceding six months.
Thirty of the survey respondents (45 percent) reported a shortage of family physicians in their counties, and 15 (22 percent) perceived a shortage of mental health professionals. Most respondents had private insurance, and only seven (10 percent) reported that they had put off seeing a physician in the past 12 months because they could not afford to pay for care. However, 58 of the 67 respondents, or 87 percent, were not satisfied with the local health care system. The mean±SD score for satisfaction with visits to the physician's office was 17.9±4.0 for the group as a whole, 18.2±3.7 for those willing to participate in telepsychiatry, and 17.3±4.4 for those unwilling to participate. Scores on the satisfaction scale ranged from 0 to 25, with 25 indicating extreme satisfaction.
Willingness to participate in telepsychiatry
Forty-five of the survey respondents, or two-thirds of the sample, expressed a willingness to use telemedicine for mental health services, and 49 of the 67, nearly three-quarters, said that they would recommend the service to a friend. About half of the Medicare enrollees in the sample of respondents were willing to participate in telepsychiatry, compared with 74 percent of those who were not covered by Medicare; however, the difference was not significant. Not surprisingly, the mean±SD age of those interested in telepsychiatry was significantly lower than those who were not, 50.1±17.6 years versus 59.9±15.4 years (t=2.21, df=65, p<.05).
The respondents who perceived their health as being good, very good, or excellent—38 respondents, or 57 percent of the total—were more willing to participate in telepsychiatry than respondents who felt their health was fair or poor. Of those who said their health was good, very good, or excellent, 79 percent were willing to participate in telepsychiatry, compared with 21 percent of those who said their health was fair or poor (χ2=5.53, df=1, p<.05).
The mean±SD number of days of abnormal activity due to physical illness in the past 30 days was 2.1±6.8 for the group as a whole, 2±6.81 for those willing to participate, and 2.18±7 days for those who were not. Chronic illness was reported by 21 of the respondents, or 46 percent, of whom 58 percent were willing to participate in telepsychiatry. The mean± SD mental health status score for all respondents was 9.8±3.2 on a scale ranging from 0 to 25, with 25 indicating optimal mental health. For those willing to participate, the mean score was 9.6±3.1, and for those unwilling to use telemedicine, it was 10.3±3.4.
The group that was willing to use telepsychiatry had a mean±SD adaptive coping score of 10.9±1.8 on a 15-point scale, with 15 indicating optimal adaptive coping skills; the group that showed no interest scored 9.9±2.3. The mean adaptive coping score for the entire group was 11±2.5. No significant difference between groups was found in the coping scores.
One-third, or 22, of the respondents were not willing to participate in telepsychiatry. The two most frequently cited reasons were a concern about confidentiality, cited by 12 respondents (55 percent), and the impersonal approach to care that the service entails, cited by 17 respondents (77 percent). Lack of knowledge about the technology was cited by six respondents (27 percent). Three respondents (14 percent) said they were unwilling to participate because of problems with hearing or vision.
Discussion and conclusions
The majority of rural residents who responded to a telephone survey expressed a willingness to use or refer others to telemedicine mental health services. However, a third of the survey respondents expressed reluctance to use such services because of concerns about confidentiality, the perceived impersonal nature of the contact, lack of knowledge about the technology, or problems with hearing or vision. Persons receiving Medicare and, in general, those who were older, were less likely to express a willingness to use telepsychiatry. This finding suggests that younger persons may be more amenable to using this technology to receive health care—possibly because they are more accustomed to technology in other aspects of their lives. It is also possible that the reluctance of older persons to use telepsychiatry reflects their greater reluctance to use mental health care services in general.
Our results also indicate that respondents with better physical health and higher adaptive coping scores tended to be more willing to participate in telepsychiatry. Self-report of poor mental health was not associated with an increased willingness to use the service. One interpretation of this finding is that persons who are less likely to require mental health services express less reluctance to use it because they do not expect to need it or use it. Hence, this study may overestimate the true acceptability of telemedicine in the rural population surveyed.
The generalizability of the study findings is uncertain because the response rate was low and the study was confined to one geographic region of a single Midwestern state. A bias may have been introduced because households that had no telephone or only a cell phone were excluded by the study's design. Despite these limitations, the findings have important implications for policy makers and providers. Telemedicine will not increase access to needed services if the intended recipients are unwilling to receive care via this mechanism. In addition to studies of technological and economic feasibility, future research must address the acceptability of this technology to the targeted population to determine its true potential for increasing access to health care in rural areas.
Acknowledgments
This project was supported by contract N01-LM-6-3548 from the National Library of Medicine. The authors acknowledge the assistance of Jayne McQuillen, Diane Mesiti, and Robyn Squire.
Dr. Rohland is affiliated with the department of health services research and management at the School of Medicine at Texas Tech University Health Sciences Center, 1C165B Health Sciences Building, 3601 Fourth Street, Lubbock, Texas 79430 (e-mail: [email protected]). Mr. Saleh is a doctoral student in the department of health management and policy in the College of Public Health at the University of Iowa. Dr. Rohrer is the head of the department of health services research and management at the School of Medicine at Texas Tech University. Dr. Romitti is in the department of epidemiology in the College of Public Health at the University of Iowa.
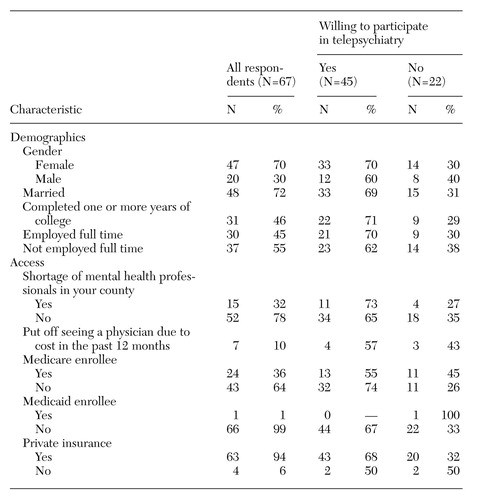 |
Table 1. Characteristics of rural respondents to telepsychiatry survey
1. Preston J, Brown FW, Hartley B: Using telemedicine to improve health care in distant areas. Hospital and Community Psychiatry 43:25-32, 1992Abstract, Google Scholar
2. Brown FW: Rural telepsychiatry. Psychiatric Services 49:963-964, 1998Link, Google Scholar
3. Ermer DJ: Experience with a rural telepsychiatry clinic for children and adolescents. Psychiatric Services 50:260-261, 1999Link, Google Scholar
4. Blackmon LA, Kaak HO, Ranseen J: Consumer satisfaction with telemedicine child psychiatry consultation in rural Kentucky. Psychiatric Services 48:1464-1466, 1997Link, Google Scholar
5. Smith HA: Telepsychiatry. Psychiatric Services 49:1494-1495, 1998Link, Google Scholar
6. Simpson C, Simpson MA. Complexity of the healthcare crisis in rural America. Journal of the American Osteopathic Association 94:502-508, 1994Crossref, Medline, Google Scholar
7. Rubin H, Gandek MS, Rogers WH, et al: Patients' ratings of outpatient visits in different practice settings: results from the Medical Outcomes Study. JAMA 270:835-840, 1993Crossref, Medline, Google Scholar
8. Carver CS: You want to measure coping but your protocol's too long: consider the brief COPE. International Journal of Behavioral Medicine 4:92-100, 1997Crossref, Medline, Google Scholar