A Review of Bipolar Disorder Among Adults
Abstract
OBJECTIVE: This paper reviews the epidemiology, etiology, assessment, and management of bipolar disorder. Special attention is paid to factors that complicate treatment, including noncompliance, comorbid disorders, mixed mania, and rapid cycling. Advances in biopsychosocial treatments are briefly reviewed, including new health service models for providing care. METHODS: A MEDLINE search was done for the period from January 1988 through October 1997 using the key terms of bipolar disorder, diagnosis, and treatment. Papers selected for further review included those published in English in peer-reviewed journals. Preference was given to articles reporting randomized, controlled trials. RESULTS: Bipolar disorder is a major public health problem. The etiology of the disorder appears multifactorial. Diagnosis often occurs years after onset of the disorder. Comorbid conditions are common. Management includes a lifetime course of medication and attention to psychosocial issues for patients and their families. Standardized treatment guidelines for the management of acute mania have been developed. New potential treatments are being investigated. CONCLUSIONS: Assessment of bipolar disorder must include careful attention to comorbid disorders and predictors of compliance. Randomized trials are needed to further evaluate the efficacy of medication, psychosocial interventions, and other health service interventions, particularly as they relate to the management of acute bipolar depression, bipolar disorder co-occurring with other disorders, and maintenance prophylactic treatment.
Bipolar disorder is a major public health problem, with estimates of lifetime prevalence in the general population of the United States ranging from 1 to 1.6 percent (1,2) and from .3 to 1.5 percent worldwide (3). Bipolar disorder is also associated with significant mortality risk; approximately 25 percent of patients attempt suicide at some time during their lives, and 11 percent of patients die by suicide (4).
Fortunately, many advances in the understanding of bipolar disorder have occurred over the past ten years. First, pharmacologic options now include lithium, valproate, and carbamazepine as standard treatments, and electroconvulsive therapy, clozapine, and antipsychotic medication as alternative or adjunctive therapies. Second, the importance of psychosocial issues for understanding patients' illnesses and factors affecting treatment compliance is more fully realized. Although the study of psychoeducation, self-help, and psychotherapeutic interventions for individuals, couples, and families is only beginning, these modalities are frequently utilized. Indeed, the American Psychiatric Association (APA) practice guideline for bipolar disorder states that "specific psychotherapeutic treatments may be critical components of the treatment plan" (5).
The National Depressive and Manic-Depressive Association (NDMDA) has taken a leading role in educating patients, their families, medical and mental health professionals, and the public at large about manic-depressive illness. The National Alliance for the Mentally Ill (NAMI) has also sought information by surveying family members about utilization of mental health services and the value of these services (6).
This paper reviews the epidemiology, etiology, diagnosis and assessment, and management of bipolar disorder.
Methods
For this review, a MEDLINE search was done for the period from January 1988 through October 1997; the key terms used were bipolar disorder, diagnosis, and treatment. Papers published in English in peer-reviewed journals were among those selected for further review. Articles reporting randomized, controlled trials were given preference.
Epidemiology
Over the course of a lifetime, bipolar I disorder affects approximately .8 percent of the adult population, and bipolar II disorder affects approximately .5 percent (7). Males and females are equally affected by bipolar I disorder, whereas bipolar II disorder is more common among women. The Epidemiologic Catchment Area (ECA) study reported a mean age of onset of 21 years for both types of bipolar disorder (8). When age of onset is stratified in five-year intervals, the peak age of onset is the 15-to-19-year age group, followed by the 20-to-24-year age group. In a survey of members of the NDMDA, more than half of the patients did not seek care for five years after first experiencing symptoms, and 36 percent did not seek care for more than ten years (9). According to the survey, the correct diagnosis was not made until an average of eight years after respondents first sought treatment.
In 1990 the economic burden of bipolar disorder in the U.S. was estimated to be $15.5 billion in diminished or lost productivity in work performance alone (10). In 1990 patients in treatment lost an estimated 152 million cumulative days from work, and untreated patients lost another 137 million days. Undertreatment of bipolar and depressive disorders is a significant factor in weighing the disorders' potential costs, because it is assumed that one-third of the untreated population with bipolar disorder can eventually be treated successfully (11).
Theoretically, efficient treatment of bipolar disorder would cost $25.6 billion annually and save $10.5 billion, a net loss of $15.1 billion, in the first year. However, by the end of the second year of treatment, the savings of $12.6 billion would exceed costs of $7 billion, for a net gain of $5.6 billion (11). Because bipolar disorder is a long-term or lifetime disorder, economic analyses need to examine a longer period of time when calculating costs or benefits.
Etiology and pathophysiology
Researchers have not developed a single hypothesis that unifies genetic, biochemical, pharmacological, anatomical, and sleep data on bipolar disorder (12). Epidemiological evidence, particularly studies of concordance in identical and fraternal twins, has implied that affective disorders are heritable. For family members of probands with bipolar disorder, the risk of morbidity is between 2.9 and 14.5 percent for bipolar disorder and between 4.2 and 24.3 percent for unipolar depression, depending on the diagnostic criteria used and the heterogeneity of the probands (12).
Whether bipolar I disorder, bipolar II disorder, hypomania, cyclothymia, and unipolar depression are genetically related or distinct entities is unknown (13). It remains unclear if the phenotype of mood disturbance is the best indicator of a genetic etiology. Therefore, it has been difficult to construct models for linkage analysis, which are necessary when simple Mendelian models do not explain inheritance—that is, when several independent genetic mutations contribute independently. However, no linkage is unequivocally established in bipolar illness at this time.
It is crucial to screen the entire genome for linkage to bipolar illness in populations, derive data from affected rather than unaffected individuals in screening studies, develop hypotheses from preliminary findings, and conduct further investigations (13). For the clinician, the concerns of patients and their relatives can be dealt with through counseling that draws on empirical risk figures in the majority of cases and on linkage results for large pedigrees that have been investigated thoroughly.
Biochemical and pharmacologic studies led to hypotheses involving the neurotransmitters catecholamine and serotonin to explain bipolar disorder. The catecholamine hypothesis presumes that mania is due to an excess of catecholamines, and depression to their depletion. Norepinephrine has been implicated mainly because of the link between depression and aberrant noradrenergic transmission. Dopamine has been implicated because the dopamine precursor L-dopa almost uniformly produces hypomania among patients with bipolar disorder. Amphetamines can also produce hypomania among patients with bipolar disorder, as well as those without it. Antipsychotic medications that selectively block dopamine receptors, such as pimozide, are effective for severe mania. Chronic use of tricyclic antidepressants presumably leads to activation of central dopaminergic neurotransmission.
The "permissive hypothesis" of serotonin function holds that low serotonergic function accounts for both manic and depressive states through defective dampening of other neurotransmitters, mainly norepinephrine and dopamine. Many other etiological theories involving neurochemicals such as neurotransmitters, enzymes, and neuropeptides are under investigation, as are theories involving the endocrine and immunological systems.
A wide range of neuroanatomical and neuroimaging studies are being conducted to learn more about bipolar disorder (12). The study of neuroanatomy is important because organic lesions are associated with signs and symptoms of bipolar disorder and because mood stabilizers are able to stabilize symptoms without altering the underlying neuropathological deficit. Lesions in the frontal and temporal lobes are most frequently associated with bipolar disorder. Left-sided lesions tend to be associated with depression and right-sided lesions with mania, though differences may occur in the posterior regions of the brain. For example, depression may be associated with lesions in the right parietooccipital region.
No abnormalities have been consistently found through computer tomography studies, although ventricular enlargement has been noted in some studies. Magnetic resonance imaging studies have revealed an increase in white matter intensities associated with bipolar disorder and correlated with age (14), although the clinical significance of these findings is unknown. Overall, most functional imaging studies, including single photon emission computer tomography and positron emission tomography, have noted prefrontal and anterior paralimbic hypoactivity in bipolar depression; preliminary studies of manic patients have yielded inconsistent findings.
Two other important biochemical models for bipolar disorder have been suggested. Post and collaborators (15) have proposed that electrophysiological kindling and behavioral sensitization underlie bipolar disorder, particularly the increasing frequency of episodes over time. Parallels between this model and bipolar disorder include the predisposing effects of both genetic factors and early environmental stress; the presence of threshold effects, in which mild alterations eventually produce full-blown episodes; the pattern that early episodes require precipitants while later ones do not; and the sequence of repeated episodes of one phase—mania or depression—leading to the emergence of the other (12).
Desynchronization of circadian rhythm has also been implicated in bipolar disorder. Data from animal studies indicate that periodic physiological disturbances can occur if two rhythms become desynchronized—that is, if one becomes free-running in and out of phase with the other (12). It is unclear if, and how, genetics contribute to the role of circadian and seasonal rhythms, the capacity for kindling and sensitization, and variation in the course of bipolar disorder, such as rapid cycling.
Diagnosis
The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) includes bipolar I disorder, bipolar II disorder, cyclothymic disorder, and bipolar disorder not otherwise specified (16). The episodes are characterized by mania, hypomania, depressive symptoms, and mixed symptoms.
The diagnostic criteria for the four types of episodes are shown in Table 1. By definition, patients with bipolar I disorder have had at least one episode of mania, whereas those with bipolar II disorder have had major depressive and hypomanic episodes. Mania occurring in patients who are taking medications such as corticosteroids or antidepressants or who have a medical illness is known as secondary mania and is classified separately in DSM-IV as substance-induced mania or mania due to a general medical condition.
The differential diagnosis of bipolar disorder is quite extensive and complex. First, the presentation of patients with bipolar disorder can be similar to that of patients with other mood and psychotic disorders, including major depression, schizoaffective disorder, and schizophrenia. A positive family history of mood disorder is suggestive of a mood disorder, even when the patient presents with prominent psychotic symptoms. Second, bipolar disorder can be associated with substance-induced disorders and with recklessness, impulsivity, truancy, and other antisocial behavior. Therefore, the disorder must be differentiated from substance-related disorders, antisocial personality disorder, and other personality disorders. Among children and adolescents, attention-deficit hyperactivity disorder and conduct disorder must be considered. Third, the relationship between affective illness and personality must be considered in making the diagnosis of bipolar disorder (17).
Bipolar disorder should always be considered in the differential diagnosis of patients with unipolar depression. Of 559 patients in the National Institute of Mental Health Collaborative Depression Study, 3.9 percent were eventually given a diagnosis of bipolar I disorder and 8.6 percent a diagnosis of bipolar II disorder on follow-up over two to 11 years (18). Prospective predictors of bipolar I disorder were acute onset of depression, severity of the depressive episode, and psychosis, while predictors of bipolar II disorder included earlier age of onset, higher rates of substance abuse, disruption of psychosocial functioning, and a protracted course. These findings are consistent with the findings of a study in which patients with bipolar disorder had an earlier and more acute onset, more total episodes, more familial mania, and equal sex distribution, compared with patients with unipolar depression (19).
Assessment
The evaluation of a patient with bipolar disorder is a complex clinical task. Neuropsychiatric assessment includes a complete history, physical examination, and laboratory evaluation. The laboratory evaluation includes a complete blood count, serum chemistries, thyroid function tests, and an erythrocyte sedimentation rate. Electroencephalograms and imaging studies may be reasonable as part of the initial assessment.
It is particularly important to detect episodes of secondary mania, which has been recognized as a subtype of mania since the 1970s (12,20). In DSM-IV, two types of secondary mania—substance-induced mania or mania due to a general medical condition—are described. Secondary mania is often difficult to treat. Although correction of the underlying organic factor, which could be infectious, toxic, or metabolic, may effectively reverse the manic presentation, many organic factors, such as stroke, trauma, and aging, are not reversible. Patients with mania originating in late life are more likely to have an underlying organic disturbance, negative family history of affective disorder, irritable behavioral characteristics, a tendency toward treatment resistance, and a higher rate of mortality (12,20). A list of frequent etiologies of secondary mania is shown in Table2.
After determining if the patient meets criteria for a specific episode type, the clinician assesses the patient for the presence of psychotic features, cognitive impairment, risk of suicide, risk of violence to persons or property, risk-taking behavior, sexually inappropriate behavior, and substance abuse. In addition, it is important to assess the patient's ability to care for himself or herself, childbearing status or plans, housing, financial resources, and psychosocial supports. The patient's self-report of symptoms may conflict with observation by others. Therefore, accurate assessment depends on information from several sources, including the patient, the patient's significant others, and records of past treatment.
Knowledge of a patient's pattern of illness is perhaps the most useful guide to treatment. Graphic representation of the illness, an example of which is shown in Figure 1, can be used to consolidate information about the sequence, polarity, severity, and frequency of illness episodes and their relationship to stressors and treatment (21). Such representations are also useful for patient education and may help in developing a therapeutic alliance (21).
Management
Treatment guidelines
APA developed the Practice Guideline for the Treatment of Patients With Bipolar Disorder (5), which is principally applicable to bipolar I disorder. The principles of psychiatric management and comments about the value of each principle are outlined in Table 3. A therapeutic alliance is crucial for managing the patient's symptoms, detecting recurrence of illness, enhancing compliance, and addressing psychosocial stressors. Patients require ongoing education about the illness, treatment options, and the impact of the illness on social and family relationships and on vocational and financial matters.
Pharmacologic treatment of bipolar disorder is detailed in the APA practice guideline (5) and is spelled out in algorithm form in the expert consensus guideline series paper on treatment of bipolar disorder (22). Medications have been shown to be effective in acute episodes and in prevention of future episodes. Medications include those that decrease symptoms of mania and depression, such as lithium, valproate, and carbamazepine, and those that may not act primarily on mood but are helpful in controlling other symptoms, such as antipsychotics and benzodiazepines.
Mood stabilizers for mania
Lithium is effective for the treatment of acute manic and depressive episodes and for the prevention of recurrent manic and depressive episodes (12). Pooled data from four placebo-controlled trials of lithium revealed a response rate of 78 percent (5). A recent review of 40 years' experience with lithium treatment reported that the dosage is generally between 600 and 2,400 mg per day (23). The therapeutic serum level is between .8 and 1.2 mEq/L. Common side effects of lithium include polydipsia, polyuria, weight gain, cognitive problems, tremor, gastrointestinal upset, acne, and hypothyroidism. Rare but potentially serious side effects include arrhythmias and toxicity resulting from an overdose.
Discontinuation of long-term lithium therapy has been associated with a significant short-term increase in risk of recurrence; in one study 50 percent of patients experienced recurrence within six months of discontinuation (24). Comparing a gradual versus rapid discontinuation of lithium, the overall median times to recurrence were 20 months and four months, respectively (25). It is of interest that patients may not respond to reinstitution of lithium therapy, even if they have been previously responsive to the medication (26).
Valproate was found to be as efficacious as lithium in a placebo-controlled trial of patients with acute mania (27). A collaborative study of valproate versus lithium in the maintenance treatment of bipolar mania is in progress. The dosage range of valproate is between 500 and 3,500 mg per day. The therapeutic plasma level is between 50 and 125 mcg/ml. No controlled trials of valproate have been carried out, but patients with acute mania appear to tolerate large initial doses of valproate—for example, a loading dose of 20 mg per kilogram of body weight per day (28). They may respond more quickly to this dose than to regular regimens developed by titrating up from initial doses of 250 mg, 500 mg, or 750 mg per day (28).
Common side effects of valproate include sedation, tremor, diarrhea, weight gain, alopecia, and benign elevation of liver transaminases. Rare but potentially serious side effects include leukopenia, thrombocytopenia, and hepatotoxicity. In a review of cases of hepatic failure coincident with use of valproate, risk factors included age of less than two years, anticonvulsant polytherapy, developmental disability, and metabolic disorders (29). For patients without those factors and who are age 11 or older, the risk of hepatic failure was approximately 1 in 500,000 (29). Patients with current or past hepatic disease may also be at risk for hepatotoxicity.
A review of 16 studies revealed that carbamazepine is efficacious for acute mania and that as a maintenance therapy it very likely reduces the frequency and severity of episodes for some patients (30). Carbamazepine has not been approved by the Food and Drug Administration (FDA) for the treatment of bipolar mania, but the authors of the 16-study review recommended its use as a standard option for treatment. The dosage range is generally between 200 and 1,800 mg per day, and the therapeutic plasma level is between 4 and 12 mcg/ml. Carbamazepine induces its own metabolism by the liver, as well as that of many other drugs. Common side effects include diplopia, blurred vision, fatigue, nausea, and ataxia. Rare but potentially serious side effects include skin rashes, leukopenia, hyponatremia, aplastic anemia, hepatic failure, exfoliative dermatitis (such as Stevens-Johnson syndrome), pancreatitis, and neurotoxicity on overdose (31).
Adjuvant medication for mania
Adjuvant medication includes the benzodiazepines and antipsychotics. Benzodiazepines have been studied alone and in combination with mood stabilizers. Generally, they are used as adjuvant therapy to decrease agitation and as a short-term treatment for insomnia (22). Patients whose insomnia is treated with sedating antidepressants have shorter asymptomatic periods between episodes of mood disorder compared with those treated with benzodiazepines (32). Antipsychotic medication is commonly used for treatment of psychotic symptoms and sometimes for severe agitation if benzodiazepines are not fully effective (22). Use of antipsychotics intermittently, or for the long term, may be necessary in treating patients whose psychotic symptoms have inadequately responded to standard mood-stabilizing agents (33).
Electroconvulsive therapy andnovel treatments for mania
Electroconvulsive therapy (ECT) is available for patients who are pregnant, unresponsive to more standard treatments, or unable to tolerate first-line treatments. ECT has been demonstrated to be rapidly effective as a treatment for acute mania, with about 80 percent of patients showing marked improvement (34). Prospective studies have considered it equally as effective or more effective than pharmacotherapy; 54 percent of medication-resistant patients responded in one study (35). For patients who are manic or depressed during the first trimester of pregnancy, ECT is usually the safest and most effective treatment (5). In an uncontrolled trial involving 22 patients with intractable bipolar disorder, monthly maintenance ECT over a two-year period reduced the rate of rehospitalization (36).
Other treatments are available for patients who are unresponsive to more standard treatments or unable tolerate first-line treatments. Clozapine is efficacious for refractory bipolar illness, particularly for patients who have bipolar mania rather than bipolar depression or rapid cycling (37,38). Calcium channel antagonists may also be used as an alternative to standard treatments (39).
One new treatment for bipolar disorder is gabapentin, which was recently approved by the FDA for the adjunct treatment of partial seizures. Gabapentin enhances gaba-ergic transmission. It has a half-life of five to seven hours, is relatively well tolerated and safe, and is almost entirely excreted by the kidneys (40). Gabapentin is an FDA category C drug for pregnant patients, which means that it carries less teratogenic risk than standard treatments in the first trimester (40). A dosage range of gabapentin for treatment of bipolar disorder has not been determined. The dosage for patients with seizures is between 900 and 1,800 mg per day, divided over three doses. Common adverse events include somnolence, ataxia, and fatigue. In a naturalistic case series of 28 patients with bipolar disorder who were prescribed gabapentin along with a concurrent mood stabilizer and antipsychotic medication, 18 had a moderate or marked response (41). Their average dose of gabapentin was 539 mg per day. No randomized controlled trials of monotherapy with gabapentin have been published.
Another new treatment for bipolar disorder is lamotrigine, which was recently approved by the FDA for the adjunct treatment of partial seizures. Lamotrigine decreases glutamate release. It has a half-life of 24 to 30 hours, is metabolized by the liver, and is also an FDA category C drug for pregnant patients. The dosage must be titrated over two to four weeks because of adverse events including dizziness, headache, double vision, somnolence, and rash (which rarely includes Stevens-Johnson syndrome) (42). The dosage for patients with seizures is between 300 and 500 mg per day, divided over two doses. Significant drug interactions occur, as carbamazepine, phenobarbital, and phenytoin decrease lamotrigine's half-life by nearly 50 percent, and valproate leads to a two- to threefold increase in its half-life (43). In a study of 67 patients with refractory bipolar disorder who were prescribed a concurrent mood stabilizer and antipsychotic medication, 82 percent of the group with depressive symptoms and 76 percent of the group with manic symptoms had a moderate or marked response to lamotrigine treatment (44,45). No randomized controlled trials examining its use as a monotherapy had been published at the time of this review.
Treatment of euphoric mania
The choice of a mood stabilizer for the treatment of mania can be guided by predictors of response, which are usually determined by the patient's history and the type of episode (46). Patients with euphoric or pure mania respond to lithium 59 to 91 percent of the time, and at slightly lower rates to valproate treatment (46). Other predictors of response to lithium include a prior history of response, relatively few lifetime episodes, excellent interepisode recovery, and an episode sequence of mania-depression-euthymia. All of the mood stabilizers are efficacious for elderly patients and those with secondary mania, but adverse events often limit the usefulness of lithium and carbamazepine (20). A review of polypharmacy by Solomon and others (47) discusses open trials of combinations of mood stabilizers for euphoric mania.
Treatment of dysphoric or mixed mania
Dysphoric or mixed mania of bipolar disorder is severe and difficult to treat. The incidence appears to be at least 30 to 40 percent of all manic episodes (12). A review of older and more recent studies revealed that dysphoric mania is more severe, is more likely to occur in women, is more likely to be associated with suicidality, has an earlier age of onset, has a longer duration, is associated with higher rates of personal and family depression, has higher concomitant alcohol or sedative-hypnotic abuse, is associated with more neuropsychiatric abnormalities, and has a poorer outcome (48).
Patients in acute episodes of mixed mania respond better to valproate than lithium (46). In a parallel-group, double-blind study of 179 patients, patients had a better response to valproate than lithium, even when the analysis statistically controlled for differences in overall severity, substance abuse, gender, age, or history (49). In uncontrolled trials, patients with mixed mania have also responded to combinations of standard mood stabilizers, clozapine, lamotrigine monotherapy (45), and lamotrigine in combination with other mood stabilizers and antipsychotic medication (44).
Treatment of rapid-cycling episodes
Many patients experience cycling of episodes. Rapid cycling consists of four or more episodes of mood disturbance a year. Ultra-rapid cycling consists of episodes occurring weeks to several days apart, and distinct, abrupt shifts of less than 24 hours constitute ultradian cycling (50). Rapid cycling occurs in 15 to 20 percent of patients with bipolar disorder (51). Compared with patients with bipolar disorder who do not have rapid cycling, those who became rapid cyclers are more likely to be female, to cycle between depression and hypomania (51), and to have associated hypothyroidism (52). Rapid cycling is associated with lower likelihood of recovery in the second year of follow-up, but not in the third, fourth, and fifth years (51).
No randomized controlled trials have assessed the treatment and prevention of rapid-cycling bipolar disorder. In acute episodes, patients with a rapid-cycling pattern appear to respond better to valproate than to lithium (46). In a 15-month prospective trial, 54 percent of patients with mania and 87 percent of patients with mixed mania had a marked response to valproate (53). In that trial, a marked prophylactic response was found for 72 percent of the patients with mania and 94 percent of those with mixed mania for the duration of the study (53). Other treatment options include adding thyroid hormone to a mood stabilizer at a dose to achieve 150 percent of normal thyroid function (52), using a combination of standard mood stabilizers, using clozapine as a monotherapy, and using clozapine in combination with lithium or valproate.
Treatment of bipolar depression
The treatment options for patients with bipolar disorder who have depressive episodes include psychiatric management, as outlined in Table 3, and use of mood-stabilizing medication, psychotherapy, antidepressant medication, and ECT (5). The treatment of bipolar depression has not been as well studied as the treatment of bipolar mania or unipolar depression. Data are also needed to distinguish the treatment of bipolar I depression from bipolar II depression.
For patients who are already taking an adequate dose of a mood stabilizer when they become depressed, the continued use of a mood stabilizer may be augmented with psychotherapy, an antidepressant, or ECT. For patients who are not taking a mood stabilizer when they become depressed or are not taking an adequate dosage, a mood-stabilizing medication should be used at adequate blood levels. Lithium is the mood stabilizer of choice for bipolar depression (22), although a full response may require four to six weeks (5).
The addition of an antidepressant to the medication regimen of patients with bipolar depression raises special concerns. First, the efficacy of antidepressants is not as well founded for bipolar depression compared with unipolar depression. Second, antidepressants can provoke manic or hypomanic symptoms. Whenever possible, the dose of the mood stabilizer and use of psychotherapy should be maximized before an antidepressant is added. Certain patients will very likely need and benefit from an antidepressant: those with severe depression who cannot wait four to six weeks until a mood stabilizer is efficacious, those who have not responded to maximal psychosocial interventions, and those with a history of response to the antidepressant. Patients and their families must be educated about the risk of a switch to mania, its warning signs, and the need for a plan for immediate intervention. The authors suggest a short duration of antidepressant treatment—one to three months—to reduce the risk of inducing mania.
The use of mood stabilizers, antidepressants, and ECT for bipolar I depression has been best described in a compilation of 18 randomized trials (54). Eight of nine controlled trials revealed that lithium was superior to placebo, and three controlled trials reported that lithium's effectiveness was equal to that of tricyclic antidepressants. Three controlled trials that included patients with bipolar I depression and bipolar II depression found that carbamazepine was superior to placebo. At the time of this review there were no controlled trials of the use of valproate as an antidepressant for bipolar depression.
ECT remains the most effective treatment for bipolar depression (54). ECT was superior to tricyclic antidepressants in five of seven studies and equivalent to tricyclics in two other studies. Five of six studies suggested that bipolar depression responds as well as unipolar depression to ECT (54).
The use of antidepressants for the treatment of bipolar depression is based on data from clinical trials and expert consensus (22). A review of studies of the use of antidepressants for bipolar depression reported only nine trials with eight or more patients (55). In this review, imipramine, bupropion, and fluoxetine proved more efficacious than placebo. Maprotiline, moclobemide, and bupropion appeared to be as efficacious as imipramine. Tranylcypromine and fluoxetine were more efficacious than imipramine. The efficacy of antidepressants for bipolar depression was roughly 50 to 75 percent (55). Interestingly, not all of the patients in these trials were on mood stabilizers.
The first-line choices for antidepressants for bipolar depression include bupropion and selective serotonin reuptake inhibitors (22). An estimated 30 to 50 percent of patients do not respond to a first-line treatment and require a longer trial of six to 12 weeks, an alternate antidepressant, ECT, or augmentation of the antidepressant with lithium, psychotherapy, or thyroid hormone (22). Once the patient is in remission, the antidepressant should be tapered sooner than is typical for unipolar depression, that is, before six to 12 months (22).
Mania that follows a depressive episode could be due to the natural course of illness or to antidepressant medication. One study found that mania is likely to be antidepressant induced and not attributable to the expected course of illness among one-third of patients with treatment-refractory bipolar disorder (56). Another study reported that it is unclear whether the use of an antidepressant precipitates rapid cycling or whether the episode of major depression itself heralds an upcoming manic episode (51). A switch from depression to mania has been reported among 28 to 70 percent of patients taking tricyclic antidepressants and monoamine oxidase inhibitors (12). A one-year study found that a combination of bupropion and lithium had a lower switch rate (11 percent) than a combination of lithium and desipramine (50 percent) (57). Switch rates for selective serotonin reuptake inhibitors have not been well studied, although the authors believe they are lower than those for tricyclic antidepressants.
Psychosocial treatments
In addition to psychiatric management and pharmacologic therapy, psychotherapeutic treatments may be beneficial to some patients with bipolar disorder (5). Most patients struggle with psychosocial issues; some of the most common stressors are listed in Table 4.
Inpatients with bipolar disorder who were surveyed about their informational needs requested information about bipolar disorder, how to obtain support, how to manage symptoms such as suicidal ideation and anger, and how to improve interpersonal skills (58). Economic, interpersonal, and vocational problems may occur for years, even when patients do not suffer recurrence of illness leading to hospitalization (59).
It has been proposed that repeat episodes of bipolar disorder are independent of stressors (60), but a relationship between biological and emotional factors may exist. In one study, patients with therapeutic levels of lithium had better psychosocial functioning than those who received doses resulting in low serum lithium levels (61). In another study, some patients who suffered recurrence of their illness had more stressors in the three months before the recurrence than those who did not suffer recurrence (62).
Psychotherapeutic treatments have been studied in controlled trials. A cognitive-behavioral treatment strategy has been shown to help educate the patient about bipolar disorder and its treatment, teach cognitive-behavioral skills for coping with psychosocial stressors, facilitate compliance with treatment, and monitor recurrence of symptoms (63). Ongoing trials of outpatient interpersonally oriented psychotherapy for individuals and a family-focused psychoeducational treatment, which is also known as behavioral family management, suggested high patient retention rates over the first year of treatment (64). Family-focused interventions held in the inpatient setting may help some patients accept their illness, identify stressors and aversive family interactions, and manage stress (65). A pilot study of family therapy and psychoeducation, in addition to pharmacologic treatment, found lower rates of family separations, greater improvements in the level of family functioning, higher rates of full recovery for the patient, and lower rates of rehospitalization during a two-year follow-up period (66).
A number of service innovations and new treatments may be useful for treatment of bipolar disorder; they include some used successfully for unipolar depression, such as cognitive therapy and behavioral therapy. A Veterans Affairs program that offered medication, standardized psychoeducation, and easy access to a primary nurse provider was associated with improvement in patients' satisfaction with care, increased intensity of medication treatment and ambulatory clinic visits, and decreased emergency room visits and hospitalizations (67). Clinical experience and preliminary research have indicated that group psychotherapy in conjunction with pharmacologic treatment may help certain patients adhere to a treatment plan, adapt to a chronic illness, regulate self-esteem, and manage marital and other psychosocial issues (5). In open trials, group therapy has been associated with a reduction in the number of hospitalizations, enhanced compliance, and increased socioeconomic functioning (68).
Trials of additional treatments for bipolar disorder are under way. They include trials of marital couples psychotherapy; family therapy, compared with family education and with medication alone; and group therapy for couples, compared with medication alone. Each of these interventions deserves further evaluation.
Comorbidity in bipolar disorder
The rates of comorbid psychiatric disorders among individuals with bipolar disorder are important for several reasons. Of primary concern is the association of comorbidity with poorer outcome and poorer treatment response (69). Accurate diagnosis and aggressive treatment of comorbid disorders may influence treatment decisions and improve treatment response. With the increased attention to cost containment in the current medical practice environment, comorbidity may also directly influence patterns of treatment availability and reimbursement. Again, accurate assessment of comorbid psychiatric disorders is likely to be an important factor in providing the most cost-effective care.
Despite the clear importance of comorbidity in the assessment and treatment of bipolar disorder, this area remains relatively understudied. Epidemiologic data have indicated that several psychiatric disorders co-occur with bipolar disorder at higher rates than would be expected by chance alone. They include substance use disorders, attention-deficit hyperactivity disorder, panic disorder, and impulse control disorders.
Table 5 summarizes the results of several studies that have noted the high prevalence of comorbid disorders among individuals being treated for bipolar disorder (70,71,72,73,74,75). Alcohol abuse or dependence was the most common substance use disorder of the patients in these studies. A wide range of other substance abuse and dependence disorders was noted as well. All impulse control disorders can occur with bipolar disorder, with pathological gambling and kleptomania the most common comorbid diagnoses.
Data from the Epidemiologic Catchment Area (ECA) study indicated that bipolar disorder was associated with the highest risk (odds ratio of 6.6) of any axis I disorder for coexistence with a drug or alcohol use disorder (76). More than 60 percent of individuals with bipolar disorder met lifetime criteria for a substance use disorder. The National Co-Morbidity Study (77), a more recent epidemiologic survey, similarly found bipolar disorder to be commonly associated with substance use disorder (odds ratio of 6.8).
The diagnosis of bipolar disorder when the patient also has a substance use disorder is difficult because the effects of drug abuse, particularly chronic use, can mimic both mania and depression. The clinician should ask very specifically about affective symptoms that predated the onset of substance use and that occur during abstinent periods and should diagnose an affective disorder only if symptoms clearly predated the substance use or persist during periods of abstinence. In the absence of either of these criteria, the clinician must observe the patient prospectively for remission of symptoms during a period of abstinence. For depression, two to four weeks of abstinence may be necessary for accurate diagnosis because symptoms of withdrawal overlap substantially with those of depression. Because mania is likely to be mimicked by substance intoxication but not substance withdrawal, shorter periods of abstinence are necessary for diagnosis of patients with manic symptoms.
Few data about the best treatment for individuals with comorbid substance use and bipolar disorder are available. Some studies have indicated that these patients have a more difficult course of illness and are more treatment resistant (78,79). One open-label pilot study has shown promising results with valproate (80), but this finding has yet to be demonstrated in a controlled clinical trial. In general, adequate pharmacologic control of mood instability is an important component of treatment for these individuals, but this intervention alone is not sufficient. Involvement of the patient in psychosocial rehabilitation, specifically cognitive-behavioral, family, and 12-step groups for substance abuse, is essential. Residential or intensive outpatient programs may also be helpful. The use of pharmacologic adjuncts to promote abstinence, such as naltrexone or disulfram, is as yet unstudied in this population, but should be considered.
Substance abuse among patients with bipolar disorder should not be ignored because it is one of the major factors in medication noncompliance and suicidality (12). Thus it has a major impact on the morbidity and mortality associated with bipolar disorder.
Attention-deficit hyperactivity disorder (ADHD) is another psychiatric disorder that commonly occurs with bipolar disorder. Winokur and colleagues (19) reported that patients with bipolar disorder had significantly higher rates of childhood ADHD compared with patients with major depression. Similarly, in a family study of adolescent bipolar disorder, 24 percent of the adolescent probands had a history of ADHD (81).
As with the substance use disorders, differential diagnosis is somewhat difficult. Symptoms of ADHD include poor concentration, distractibility, impulsivity, restlessness, and agitation, which are also features of a manic or hypomanic episode. The similarities can be particularly problematic because the first-line treatments for ADHD—stimulants and antidepressant drugs—are relatively contraindicated for individuals with bipolar disorder.
A diagnosis of ADHD should not be made if the individual is in the midst of a manic or hypomanic episode. The mania should be aggressively treated, and when the patient's mood is stabilized, ADHD symptoms can be assessed. In making the distinction between bipolar disorder and ADHD on a historical basis, it is important to inquire about the episodic or chronic nature of the symptoms and about symptoms that are more specific to mania, such as elated mood, grandiosity, hypersexuality, and decreased need for sleep. Finally, if a decision is made to treat ADHD in an individual with bipolar disorder, it is important to avoid agents that might precipitate mania or worsen the course of bipolar disorder. Clonidine may be a reasonable alternative to stimulants or antidepressants (82).
Several investigators have reported higher rates of panic disorder among individuals with bipolar disorder than would be expected from the prevalence rates of panic disorder in the general population (70,71,83). Although further study of this relationship is necessary, it is likely that untreated panic disorder and other anxiety disorders may worsen the course and prognosis of bipolar disorder. As with the treatment of ADHD, many of the first-line pharmacologic treatments for panic disorder and other anxiety disorders—antidepressants—can precipitate mania and must be used with caution in treating individuals with comorbid bipolar disorder and panic disorder. Consideration should be given to alternative strategies, such as use of valproic acid, which may be helpful in the treatment of both panic disorder (84) and bipolar disorder (26).
Several recent studies have also demonstrated relatively high rates of co-occurrence of obsessive-compulsive disorder with bipolar disorder. Boyd and colleagues (83), in an analysis of ECA data, found obsessive-compulsive disorder to be much more common among individuals with bipolar disorder than in the general population (odds ratio of 18). Other studies have found high rates of comorbid mania among patients with obsessive-compulsive disorder (85,86).
In general, much remains unclear about the relationship of these disorders to each other. Obsessive-compulsive disorder among patients with bipolar disorder may be related to the presence of depressive symptoms during mania, or the obsessive-compulsive symptoms may be an atypical presentation of depression during the course of bipolar disorder. In any case, as with the disorders previously discussed, this comorbidity has important treatment implications because many medications used to treat obsessive-compulsive disorder can precipitate mania. Reports from clinical trials of antidepressants involving patients with obsessive-compulsive disorder have suggested that as many as 20 percent of patients may develop mania during antidepressant treatment (87).
The relationship between bipolar disorder and personality is a complex one, both from a theoretical and from a diagnostic perspective. The differentiation of enduring personality characteristics from changes that occur as a result of acute illness can be particularly difficult with affective illness because affect is one of the contexts through which personality is expressed. Akiskal and colleagues (88) have outlined a number of possible relationships between bipolar disorder and personality disorders, and the area is also well discussed in a recent review (17).
Studies of specific personality disorders among patients with bipolar disorder have found high rates of cluster B diagnoses and particularly high rates of borderline personality disorder (89,90). However, the literature has numerous reports of bipolar-spectrum disorders misdiagnosed as borderline personality disorder (91), and many of the criteria for borderline personality disorder and hypomania overlap.
Although a thorough review of the many complexities in this area is beyond the scope of this review, it is important to keep in mind that the symptom overlap between bipolar disorder and several personality disorders is substantial. The overlap is particularly pertinent when considering hypomania, cyclothymia, or more subtle affective disorder diagnoses. Diagnoses of personality disorder among patients with bipolar disorder should be made during times of affective stability to ensure the most accurate diagnosis.
Natural history and course
The first episode of bipolar disorder may be manic, hypomanic, mixed, or depressive. The natural course of bipolar disorder is characterized by high rates of relapse and recurrence (12) at rates of 80 to 90 percent (79). In prospective outcome studies extending up to four years, less than half of patients followed after an initial manic episode had sustained a good response to treatment (79). Full functional recovery between affective episodes often lags behind symptomatic recovery (59,92). Following recovery from a mood episode, patients with bipolar disorder had an average of .6 episodes per year over a five-year period (19). Compared with multiple-episode mania, first-episode mania was associated with a significantly shorter hospitalization; however, gender, age at onset of illness, comorbidity, and family history were similarly distributed in the two groups (93). Data have largely been derived from naturalistic studies, in which treatment is prescribed by clinicians in response to patients' needs and becomes an outcome in itself, as the clinical condition largely determines the choice of treatment. In controlled trials, treatments are standardized, but the study population is likely to be biased by an increased adherence to treatment regimens. Therefore, data from naturalistic studies may better represent the course of patients under typical clinical conditions.
Many questions about the predictors of recurrence remain. The cumulative probability of recurrence has been reported to be more than 50 percent during the first year of follow-up, about 70 percent by the end of four years, and nearly 90 percent by five years (79,94). Recurrence of mood episodes has been associated with comorbid nonaffective psychiatric disorder, particularly substance abuse; the presence of psychotic features; and a family history of mania or schizoaffective mania (68). One study found that patients who are symptomatic six months after their first episode had a 45 percent greater chance of experiencing a recurrence of mania or major depression at least once during the remainder of a four-year study (79). There are conflicting data about whether age at illness onset, gender, premorbid psychosocial functioning, number of years of illness, and number of prior episodes predict recurrence (68). As stated before, after gradual versus rapid discontinuation of lithium, the overall median time to recurrence was found to be 20 months and four months, respectively (25).
Preliminary data about the efficacy of maintenance treatment with mood stabilizers have been published, but further studies are needed. A review of pharmacologic maintenance therapies reported that approximately 33 percent of patients on lithium remained symptom free at five years, and that combining lithium with other mood stabilizers, benzodiazepines, or antipsychotics may provide greater prophylaxis (95). Patients with lithium blood levels greater that .8 mEq/L clearly have a better outcome (95). Several studies reported equivalent efficacy of carbamazepine and lithium for maintenance therapy, but methodological flaws raise serious questions about the results (96).
A recent randomized trial involving 144 patients that compared lithium to carbamazepine found no differences in rates of hospitalization and recurrence at 2.5-year follow-up (96). However, lithium was superior in preventing recurrences when combined with other medications, and fewer patients had side effects that prompted its discontinuation. As a result, recurrence among patients who completed the study was less frequent among patients who received lithium (28 percent) than among those who received carbamazepine (47 percent) (96). In one study full compliance with maintenance therapy over a one-year period was accomplished by only 49 percent of patients (97).
Conclusions
Bipolar disorder is a major public health problem, associated with significant morbidity and a high mortality risk. Several factors make treatment complex, including the fluctuation of mood episodes and the effects of these episodes on patient well-being, lack of adherence to treatment, and comorbid psychiatric disorders. Standardized management guidelines have been developed for acute bipolar mania but are not yet available for acute bipolar depression or maintenance treatment. A number of pharmacologic and psychosocial treatments are under study in randomized trials.
Dr. Hilty is assistant professor of clinical psychiatry and Dr. Hales is professor and chair of psychiatry at the University of California, Davis, 4430 V Street, Sacramento, California 95817 (e-mail, [email protected]). Dr. Brady is associate professor of psychiatry at the Medical University of South Carolina College of Medicine in Charleston.
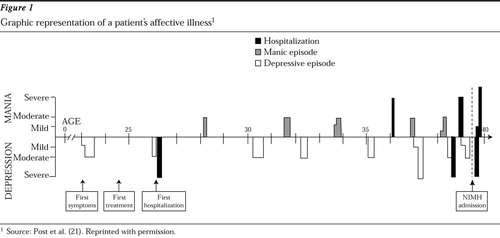
Figure 1. Graphic representation of a patient's affective illness1
1 Source: Post et al. (12)
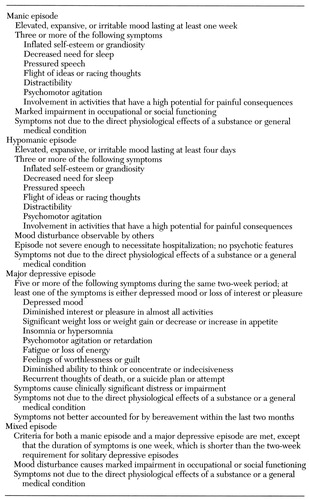 |
Table 1. DSM-IV diagnostic criteria for mood disorder episodes characteristic of bipolar disorder
 |
Table 2. Organic causes of manic and hypomanic symptoms1
1Source: Goodwin and Jamison (12)
2Meets criteria of Krauthammer and Klerman for cause of secondary mania—a manic syndrome occurring shortly after medical, pharmacological, or other somatic dysfunction in a patient with no history of affective illness. The criteria are discussed in Manic-Depressive Illness(12, p. 111).
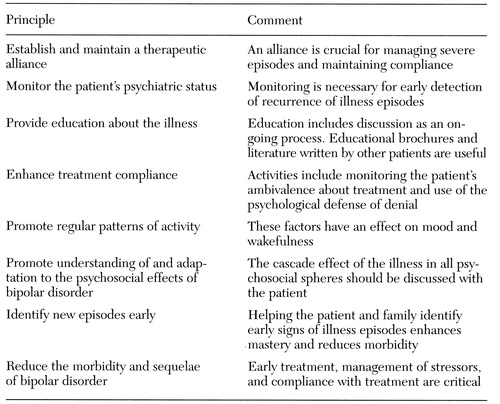 |
Table 3. Principles of psychiatric management of patients with bipolar disorder and comments on their application1
1Based on Practice Guideline for the Treatment of Patients With Bipolar Disorder (5)
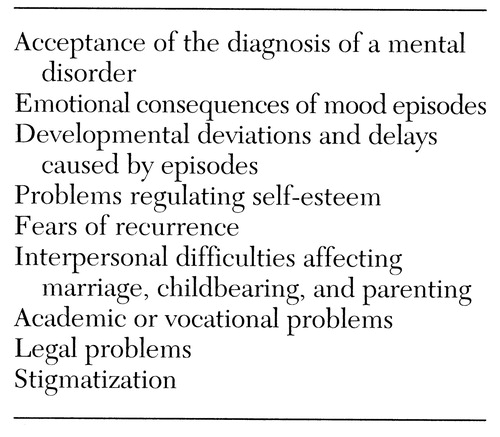 |
Table 4. Common Psychological stressors for patients with bipolar disorder
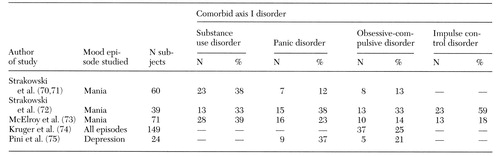 |
Table 5. Study Findings on the prevalence of comorbidity of bipolar disorder and other axis I disorders
1. Robins LN, Regier DA (eds): Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, Free Press, 1991Google Scholar
2. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Co-Morbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
3. Weissman MM, Bland RC, Canino GJ, et al: Cross-national epidemiology of major depression and bipolar disorder. JAMA 276:293-299, 1996Crossref, Medline, Google Scholar
4. Prien RF, Potter WZ: NIMH workshop report on treatment of bipolar disorder. Psychopharmacology Bulletin 26:409-427, 1990Medline, Google Scholar
5. Hirschfeld RMA, Clayton PJ, Cohen I, et al: Practice Guideline for the Treatment of Patients With Bipolar Disorder. American Journal of Psychiatry 151(suppl 12):1-36, 1994Google Scholar
6. Hatfield AB, Gearon JS, Coursey RD: Family members' ratings of the use and value of mental health services: results of a national NAMI survey. Psychiatric Services 47:825-831, 1996Link, Google Scholar
7. Weissman MM, Bruce ML, Leaf PJ, et al: Affective disorders, in Psychiatric Disorders in America. Edited by Robins L, Regier DA. New York, Free Press, 1990Google Scholar
8. Weissman MM, Leaf PJ, Tischer GL, et al: Affective disorders in five United States communities. Psychological Medicine 18:141-153, 1988Crossref, Medline, Google Scholar
9. National survey of NDMDA members finds long delay in diagnosis of manic-depressive illness. Hospital and Community Psychiatry 44:800-802, 1993Medline, Google Scholar
10. Greenberg PE, Stiglin LE, Finkelstein SN, et al: The economic burden of depression in 1990. Journal of Clinical Psychiatry 54:405-418, 1993Medline, Google Scholar
11. Keck PE, Bennett JA, Stanton SP: Health-economic aspects of the treatment of manic-depression illness with divalproex. Review of Contemporary Pharmacotherapy 6:597-604, 1995Google Scholar
12. Goodwin FK, Jamison KR: Manic-Depressive Illness. New York, Oxford University Press, 1990Google Scholar
13. Reus VI, Freimer NB: Understanding the genetic basis of mood disorders: where do we stand? American Journal of Human Genetics 60:1283-1288, 1997Google Scholar
14. Altshuler LL, Curran JG, Hauser P, et al: T2 hyperintensities in bipolar disorder: magnetic resonance imaging comparison and literature meta-analysis. American Journal of Psychiatry 152:1139-1144, 1995Link, Google Scholar
15. Post RM, Rubinow DR, Ballenger JC: Conditioning, sensitization, and kindling: implications for the course of affective illness, in The Neurobiology of Mood Disorders. Edited by Post RM, Ballenger JC. Baltimore, Williams & Wilkins, 1984Google Scholar
16. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
17. Kopacz DR, Janicak PG: The relationship between bipolar disorder and personality. Psychiatric Annals 26:644-650, 1996Crossref, Google Scholar
18. Akiskal HS, Maser JD, Zeller PJ, et al: Switching from "unipolar" to bipolar II. Archives of General Psychiatry 52:114-123, 1995Crossref, Medline, Google Scholar
19. Winokur G, Coryell W, Endicott J: Further distinctions between manic-depressive illness (bipolar disorder) and primary depressive disorder (unipolar depression). American Journal of Psychiatry 150:1176-1181, 1993Link, Google Scholar
20. Evans DL, Byerly MJ, Greer RA: Secondary mania: diagnosis and treatment. Journal of Clinical Psychiatry 56(suppl 3):31-37, 1995Medline, Google Scholar
21. Post RM, Roy-Byrne PP, Uhde TW: Graphic representation of the life course of illness in patients with affective disorder. American Journal of Psychiatry 145:844-848, 1988Link, Google Scholar
22. Frances A, Docherty JP, Kahn DA: Treatment of bipolar disorder. Journal of Clinical Psychiatry 57(suppl 12A):1-88, 1996Google Scholar
23. Schou M: Forty years of lithium treatment. Archives of General Psychiatry 54:9-13, 1997Crossref, Medline, Google Scholar
24. Faedda GL, Tondo L, Baldessarini RJ, et al: Outcome after rapid versus gradual discontinuation of lithium treatment in bipolar disorders. Archives of General Psychiatry 50:448-455, 1993Crossref, Medline, Google Scholar
25. Baldessarini RJ, Tondo L, Faedda GL, et al: Effects of the rate of discontinuing lithium maintenance treatment in bipolar disorders. Journal of Clinical Psychiatry 57:441-448, 1996Crossref, Medline, Google Scholar
26. Maj M, Pirozzi R, Magliano L: Nonresponse to reinstituted lithium prophylaxis in previously responsive bipolar patients: prevalence and predictors. American Journal of Psychiatry 152:1810-1811, 1995Link, Google Scholar
27. Bowden CL, Brugger AM, Swann AC, et al: Efficacy of divalproex versus lithium and placebo in the treatment of mania. JAMA 271:918-924, 1994Crossref, Medline, Google Scholar
28. Keck PE, McElroy SL, Tugrul KC, et al: Valproate oral loading in the treatment of acute mania. Journal of Clinical Psychiatry 54:305-308, 1993Medline, Google Scholar
29. Bryant AE, Dreifuss FE: Valproic acid hepatic fatalities: III. US experience since 1986. Neurology 46:465-469, 1996Crossref, Medline, Google Scholar
30. Janicak PG, Davis JM, Preskorn SH, et al: Principles and Practice of Psychopharmacology. Baltimore, Williams & Wilkins, 1993Google Scholar
31. Pellock JM, Willmore LJ: A rational guide to routine blood monitoring in patients receiving antiepileptic drugs. Neurology 41:961-964, 1991Crossref, Medline, Google Scholar
32. Saiz-Ruiz J, Cebollada A, Ibanez A: Sleep disorders in bipolar depression: hypnotics versus sedative antidepressants. Journal of Psychosomatic Research 38(suppl):55-60, 1994Google Scholar
33. Sernyak MJ, Woods SW: Chronic neuroleptic use in manic-depressive illness. Psychopharmacologic Bulletin 29:375-381, 1993Medline, Google Scholar
34. Mukherjee S, Sackeim HA, Schnurr DB: Electroconvulsive therapy of acute manic episodes: a review. American Journal of Psychiatry 151:169-176, 1994Link, Google Scholar
35. Mukherjee S, Sackeim HA, Lee C: Unilateral ECT in the treatment of manic episodes. Convulsive Therapy 4:74-80, 1988Medline, Google Scholar
36. Vanelle JM, Loo H, Galinowski A, et al: Maintenance ECT in intractable manic-depressive disorders. Convulsive Therapy 10:195-205, 1994Medline, Google Scholar
37. Banov MD, Zarate CA Jr, Tohen M, et al: Clozapine therapy in refractory affective disorders: polarity predicts response in long-term follow-up. Journal of Clinical Psychiatry 55:295-300, 1994Medline, Google Scholar
38. Calabrese JR, Kimmel SE, Woyshville MJ, et al: Clozapine for treatment-refractory mania. American Journal of Psychiatry 153:759-764, 1996Link, Google Scholar
39. Dubovsky SL, Buzan RD: Novel alternatives and supplements to lithium and anticonvulsants for bipolar affective disorder. Journal of Clinical Psychiatry 58:224-242, 1997Crossref, Medline, Google Scholar
40. Ramsey RE: Clinical efficacy and safety of gabapentin. Neurology 44(suppl 5):523-530, 1994Google Scholar
41. Schaffer CB, Schaffer LC: Gabapentin in the treatment of bipolar disorder. American Journal of Psychiatry 154:291-291, 1997Link, Google Scholar
42. Richens A: Safety of lamotrigine. Epilepsia 35(suppl):37-40, 1994Google Scholar
43. Pellock JM: The clinical efficacy of lamotrigine as an antiepileptic drug. Neurology 44(suppl 8):29-35, 1994Google Scholar
44. Calabrese JR, Bowden CL, Rhodes LJ, et al: Lamotrigine in treatment-refractory bipolar disorder. Presented at the annual meeting of the American Psychiatric Association, New York City, May 4-9, 1996Google Scholar
45. Sporn J, Sachs G: The anticonvulsant lamotrigine in treatment-refractory manic-depressive illness. Journal of Clinical Psychopharmacology 17:185-189, 1997Crossref, Medline, Google Scholar
46. Bowden CL: Predictors of response to divalproex and lithium. Journal of Clinical Psychiatry 56(suppl 3):25-30, 1995Medline, Google Scholar
47. Solomon DA, Keitner GI, Ryan CE, et al: Polypharmacy in bipolar I disorder. Psychopharmacology Bulletin 32:579-587, 1996Medline, Google Scholar
48. McElroy SL, Keck PE Jr, Pope HG, et al: Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. American Journal of Psychiatry 149:1633-1644, 1992Link, Google Scholar
49. Swann AC, Bowden CL, Morris D, et al: Depression during mania. Archives of General Psychiatry 54:37-42, 1997Crossref, Medline, Google Scholar
50. Kramlinger KG, Post RM: Ultra-rapid and ultradian cycling in bipolar affective illness. British Journal of Psychiatry 168:314-323, 1996Crossref, Medline, Google Scholar
51. Coryell W, Endicott J, Keller M: Rapidly cycling affective disorder. Archives of General Psychiatry 49:126-131, 1992Crossref, Medline, Google Scholar
52. Bauer MS, Whybrow PC: Rapid cycling bipolar affective disorder. Archives of General Psychiatry 47:435-440, 1990Crossref, Medline, Google Scholar
53. Calabrese JR, Markovitz PJ, Kimmel SE, et al: Spectrum of efficacy of valproate in 78 rapid-cycling bipolar patients. Journal of Clinical Psychopharmacology 12(suppl 1):53S-56S, 1992Google Scholar
54. Zornberg GL, Pope HG: Treatment of depression in bipolar disorder: new directions for research. Journal of Clinical Psychopharmacology 13:397-408, 1993Crossref, Medline, Google Scholar
55. Sachs GS: Treatment-resistant bipolar depression. Psychiatric Clinics of North America 19:215-236, 1996Crossref, Medline, Google Scholar
56. Altshuler LL, Post RM, Leverich GS, et al: Antidepressant-induced mania and cycle acceleration: a controversy revisited. American Journal of Psychiatry 152:1130-1138, 1995Link, Google Scholar
57. Sachs GS, Lafer B, Stoll AL: A double-blind trial of bupropion versus desipramine for bipolar depression. Journal of Clinical Psychiatry 55:391-393, 1994Medline, Google Scholar
58. Pollack LE: Informational needs of patients hospitalized for bipolar disorder. Psychiatric Services 46:1191-1194, 1995Link, Google Scholar
59. Coryell W, Scheftner W, Keller M, et al: The enduring psychosocial consequences of mania and depression. American Journal of Psychiatry 150:720-727, 1993Link, Google Scholar
60. Post RM: Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry 149:999-1010, 1992Link, Google Scholar
61. Solomon DA, Ristow WR, Keller MB, et al: Serum lithium levels and psychosocial function in patients with bipolar disorder. American Journal of Psychiatry 153:1301-1307, 1996Link, Google Scholar
62. Hammen C, Gitlin M: Stress reactivity in bipolar patients and its relation to prior history of disorder. American Journal of Psychiatry 154:856-857, 1997Link, Google Scholar
63. Basco MR, Rush AJ: Cognitive-Behavioral Therapy for Bipolar Disorder. New York, Guilford, 1997Google Scholar
64. Miklowitz DJ, Frank E, George EL: Clinical trials: bipolar disorder: new psychosocial treatments for the outpatient management of bipolar disorder. Psychopharmacology Bulletin 32:613-621, 1996Medline, Google Scholar
65. Clarkin JF, Glick ID, Haas GL, et al: A randomized clinical trial of inpatient family intervention: V. results for affective disorders. Journal of Affective Disorders 18:17-28, 1990Crossref, Medline, Google Scholar
66. Miller IW, Keitner GI, Epstein NB, et al: Families of bipolar patients: dysfunction, course of illness, and pilot treatment study, in Proceedings of the 22nd Meeting of the Society for Psychotherapy Research, Lyon, France, July 2-6, 1991Google Scholar
67. Bauer MS, McBride L, Shea N, et al: Impact of an easy-access VA clinic-based program for patients with bipolar disorder. Psychiatric Services 48:491-496, 1997Link, Google Scholar
68. Solomon DA, Keitner GI, Miller IW, et al: Course of illness and maintenance treatment for patients with bipolar disorder. Journal of Clinical Psychiatry 56:5-13, 1995Medline, Google Scholar
69. Keitner GI, Ryan CE, Miller IW, et al:12-month outcome of patients with major depression and comorbid psychiatric or medical illness (compound depression). American Journal of Psychiatry 148:345-350, 1991Google Scholar
70. Strakowski SM, Tohen M, Stoll AL, et al: Comorbidity in mania at first hospitalization. American Journal of Psychiatry 149:554-556, 1992Link, Google Scholar
71. Strakowski SM, Tohen M, Stoll AL, et al: Comorbidity in psychosis at first hospitalization. American Journal of Psychiatry 150:752-757, 1993Link, Google Scholar
72. Strakowski SM, Keck PE Jr, McElroy SL, et al: Chronology of comorbid and principal syndromes in first-episode psychosis. Comprehensive Psychiatry 36:106-112, 1995Crossref, Medline, Google Scholar
73. McElroy SL, Strakowski SM, Keck PE Jr, et al: Differences and similarities in mixed and pure mania. Comprehensive Psychiatry 36:187-194, 1995Crossref, Medline, Google Scholar
74. Kruger S, Cooke RG, Hasey GM, et al: Comorbidity of obsessive compulsive disorder in bipolar disorder. Journal of Affective Disorders 34:117-120, 1995Crossref, Medline, Google Scholar
75. Pini S, Cassano GB, Simonini E, et al: Prevalence of anxiety disorders comorbidity in bipolar depression. Journal of Affective Disorders 42:145-153, 1997Crossref, Medline, Google Scholar
76. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
77. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:17-31, 1996Crossref, Medline, Google Scholar
78. Brady K, Casto S, Lydiard RB, et al: Substance abuse in an inpatient psychiatric sample. American Journal of Drug and Alcohol Abuse 17:389-397, 1991Crossref, Medline, Google Scholar
79. Tohen M, Waternaux CS, Tsuang MT: Outcome in mania: a 4-year prospective follow-up of 75 patients utilizing survival analysis. Archives of General Psychiatry 47:1106-1111, 1990Crossref, Medline, Google Scholar
80. Brady KT, Sonne SC, Anton R, et al: Valproate in the treatment of acute bipolar affective episodes complicated by substance abuse: a pilot study. Journal of Clinical Psychiatry 56:118-121, 1995Medline, Google Scholar
81. Strober M, Morrell W, Burroughs J, et al: A family study of bipolar I disorder in adolescence: early onset of symptoms linked to increased familial loading and lithium resistance. Journal of Affective Disorders 15:255-268, 1988Crossref, Medline, Google Scholar
82. Spencer T, Biederman J, Wilens T, et al: Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. Journal of the American Academy of Child and Adolescent Psychiatry 35:409-432, 1996Crossref, Medline, Google Scholar
83. Boyd JH, Burke JD Jr, Gruenberg E, et al: Exclusion criteria of DSM-III: a study of co-occurrence of hierarchy-free syndromes. Archives of General Psychiatry 41:983-989, 1984Crossref, Medline, Google Scholar
84. Keck PE Jr, McElroy SL, Friedman LM: Valproate and carbamazepine in the treatment of panic and posttraumatic stress disorders, withdrawal states, and behavioral dyscontrol syndromes. Journal of Clinical Psychopharmacology 12(suppl 1):36S-41S, 1992Google Scholar
85. Karno M, Golding J: Obsessive compulsive disorder, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991Google Scholar
86. Rasmussen SA, Tsuang MT: Clinical characteristics and family history in DSM-III obsessive-compulsive disorder. American Journal of Psychiatry 143:317-322, 1986Link, Google Scholar
87. Jefferson JW, Greist JH, Perse TL, et al: Fluvoxamine-associated mania/hypomania in patients with obsessive-compulsive disorder (ltr). Journal of Clinical Psychopharmacology 11:391-392, 1991Crossref, Medline, Google Scholar
88. Akiskal HS, Hirschfeld RM, Yerevanian BI: The relationship of personality to affective disorders. Archives of General Psychiatry 40:801-810, 1983Crossref, Medline, Google Scholar
89. Turley B, Bates GW, Edwards J, et al: MCMI-II personality disorders in recent-onset bipolar disorders. Journal of Clinical Psychology 48:320-329, 1992Crossref, Medline, Google Scholar
90. Peselow ED, Sanfilipo MP, Fieve RR: Relationship between hypomania and personality disorders before and after successful treatment. American Journal of Psychiatry 152:232-238, 1995Link, Google Scholar
91. Akiskal HS: Subaffective disorders: dysthymic, cyclothymic, and bipolar II disorders in the "borderline" realm. Psychiatric Clinics of North America 4:25-46, 1981Crossref, Medline, Google Scholar
92. Dion GL, Tohen M, Anthony WA, et al: Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hospital and Community Psychiatry 39:652-657, 1988Abstract, Google Scholar
93. Keck PE Jr, McElroy SL, Strakowski SM, et al: Outcome and comorbidity in first-compared with multiple-episode mania. Journal of Nervous and Mental Disease 183:320-324, 1995Crossref, Medline, Google Scholar
94. Keller MB, Waternaux CM, Tsuang MT: Bipolar I: a five-year prospective follow-up. Journal of Nervous and Mental Disease 181:238-245, 1993Crossref, Medline, Google Scholar
95. Keck PE Jr, McElroy SL: Outcome in the pharmacologic treatment of bipolar disorder. Journal of Clinical Psychopharmacology 16(suppl 1):15-23, 1996Google Scholar
96. Griel W, Ludwig-Mayerhofer W, Erazo N, et al: Lithium versus carbamazepine in the maintenance treatment of bipolar disorders: a randomized study. Journal of Affective Disorders 43:151-161, 1997Crossref, Medline, Google Scholar
97. Keck PE Jr, McElroy SL, Strakowski SM, et al: Compliance with maintenance treatment in bipolar disorder. Psychopharmacology Bulletin 33:87-91, 1997Medline, Google Scholar



