A Randomized Controlled Study of the Effectiveness of Intensive Outpatient Treatment for Cocaine Dependence
Abstract
OBJECTIVE: A randomized controlled study design was used to compare the effectiveness of intensive outpatient treatment with individual outpatient counseling and a combination of individual and group outpatient counseling for cocaine-dependent patients. METHODS: Volunteers for this study were recruited from among first admissions to an inner-city, public-sector outpatient substance abuse clinic. In-treatment, end-of-treatment, and nine-month follow-up assessments were compared for participants randomly assigned for 12 weeks to one of three treatment modalities—weekly individual outpatient counseling, weekly individual counseling plus one weekly group session, or a newly designed intensive group treatment program consisting of three hours of group treatment three days a week. Results and conclusions: Patients who completed the intensive program showed significant improvement from intake to end-of-treatment scores on the Addiction Severity Index, the Beck Depression Inventory, and the Symptom Checklist. At nine-month follow-up, patients who had remained in treatment longer had fewer drug problems, a smaller proportion of positive urine drug screening tests, a better employment status, and fewer psychological problems compared with patients who left treatment earlier. Patients who remained in treatment were also more likely to be attending self-help meetings, continuing in outpatient treatment, or attending school. However, for the 447 patients randomly assigned to the three conditions, there were no significant differences between treatment modalities on any of the variables at nine-month follow-up. The new intensive treatment program was not shown to be superior to more traditional treatment programs.
In a previous paper by Weinstein and colleagues (1), we described the design of a new 12-week intensive outpatient treatment program for cocaine-dependent patients that included three hours of group counseling and activity sessions three times weekly. The paper also reported the initial findings of a five-year study comparing the outcomes of cocaine-dependent volunteers randomly assigned to either the new intensive program or to one of two more traditional modalities—individual counseling for one hour weekly or individual counseling plus a group session once a week.
Barely recognized a decade ago, intensive outpatient treatment has become a major treatment modality (2,3) and a widely accepted level of care (4). It is now considered a treatment of choice for many substance-dependent patients, and its popularity has continued to grow as clinicians have espoused its helpfulness (5,6,7,8). Nevertheless, with few exceptions (9,10,11), outcome evaluation studies of intensive outpatient treatment have not been conducted; our previous paper (1) represented, to the best of our knowledge, the first reported randomized controlled study of the effectiveness of this modality of care.
The purpose of the study described here was to expand on our earlier report by providing data on our entire sample of 447 patients, presenting nine-month follow-up results, and assessing the effect of treatment on AIDS risk behavior as well as on substance abuse at follow-up. We hypothesized that patients in the intensive outpatient treatment program would show significantly more improvement in substance use and problem severity at follow-up than those who received weekly individual counseling plus a group session, who would in turn do better than those who received weekly individual counseling. We also hypothesized that, irrespective of treatment modality, a better treatment outcome would be associated with a decrease in AIDS risk behavior.
Methods
Subjects
Study participants were recruited from among individuals entering an ongoing community-based, inner-city, publicly funded, 12-week outpatient cocaine treatment program in Philadelphia. Those asked to volunteer were first admissions above age 18 years who had a DSM-III-R diagnosis of cocaine dependence and who were not overtly psychotic, actively suicidal, or so cognitively impaired as to be unable to understand informed consent or to participate in the programming. Intake interviews and clinical ratings were done by members of our counseling staff with supervision of the senior counselor or psychiatrist medical director and assistance or intervention from them when appropriate. The subjects were recruited for the study between August 1990 and July 1994.
Assessments
Initial intake information obtained from research volunteers and regular patients was used to develop treatment plans and for record keeping, data reporting, and meeting state regulations. The set of forms and measures included a brief intake form covering basic demographic data, treatment and employment histories, and personal and family history of substance use; a self-administered Milcom, which provides a personal and family medical history and review of systems (12); a urine drug screen; the Risky AIDS Behavior (RAB) inventory (13), which combines items on risk from sexual behavior and sharing needles for intravenous drugs; the number of DSM-III-R criteria present; the AIDS Knowledge Survey (AKS), a modified version of a form used by agencies of the City of Philadelphia; the Addiction Severity Index (ASI), indicating difficulties in seven problem areas (14); the Beck Depression Inventory (BDI), a standard measure of depression (15); and the Symptom Checklist (SCL-90-R), a quick, multifactor measure of global psychopathology (16).
Administration of the battery, including a treatment planning session and interview with a counselor, usually required about two hours. On a second visit, patients completed a detailed, self-administered Psychosocial History Form, attended an AIDS instructional module, repeated the AKS, and met with their therapists. Research volunteers were paid $30 for participating in an additional testing session.
Follow-up interviews were done by an independent contractor nine months after admission. Patients received $20 for participating in the follow-up, which included telephone administration of the ASI and RAB and questions about the patients' experience with additional treatment, their legal and employment status, and their attendance at 12-step self-help groups during the period after discharge from the treatment program.
Assignment to treatment
After completing the initial assessments, patients who met criteria for admission into the study were informed about the study and invited to participate and give written consent. Volunteers were randomly assigned to the intensive program, individual counseling, or individual counseling plus group sessions for 12-week programs. Patients who did not meet study criteria—for example, repeat admissions and patients who declined to participate—as well as the study volunteers assigned to the intensive program entered the regular, ongoing 12-week intensive program. The three groups of volunteers and the nonvolunteers were treated by the same staff members in rotation.
A persistent methodological problem in comparing individual and group therapies has been the issue of an equivalent dose of treatment exposure. Although it does not seem reasonable to expect one hour of individual therapy and one hour of group therapy to have equal effects, guidelines for comparing group hours with individual hours are not available (17).
Because we were concerned with the cost-effectiveness of the treatment models, we attempted to keep staff time utilization and costs equivalent for the three treatments. One hour a week of individual counseling, for example, would require nine staff hours per week for nine patients. Treatment for those assigned to one hour weekly of individual counseling plus one hour of group counseling would require ten staff hours per week for nine patients, and treatment for those assigned to nine hours weekly of group counseling would require nine staff hours per week for nine patients. With staff hour costs across treatments held roughly comparable, recommendations could be made according to which of the treatments best served the needs of the patients according to the outcome results of the trial.
Treatment approach
In accordance with public-sector policies and procedures, our general treatment approach, for regular and research patients alike, was problem oriented and focused on attaining specifically defined behavioral objectives through action steps delineated in a treatment plan prepared with the patient during the intake process and updated monthly. Attendance at self-help meetings on- and off-site was encouraged. Techniques appropriate to addressing particular problem areas and action steps were drawn from several treatment models (18,19,20,21). Although pharmacotherapy was not routinely used, it was available as needed. This multimodal approach adapting behavioral, exploratory, supportive, and expressive techniques to the particular problem areas of the patients seemed compatible with approaches recommended in literature reviews on cocaine treatment (22,23,24). We believe this approach was also fairly typical of most treatment programs in our state and many others.
Results
Of the 862 patients asked to participate in the study, 488 were male (56.6 percent), 804 were African American (93.3 percent), 781 were unemployed (90.6 percent), and 646 had never married (75.4 percent). The mean± SD age was 31.75±6.58 years.
All met DSM-III-R criteria for cocaine use disorder. They were judged to exhibit a mean±SD of 7.33±1.6 of the nine DSM-III-R substance use dependence criteria. They reported having used cocaine for a mean of 6.88±5.56 years and on 8.03±8.95 of the last 30 days. The admission urine analysis of 52.9 percent of the patients was positive for cocaine. The mean±SD ASI score was 6.39±1.2 on a scale from 0 to 9, with higher scores indicating greater severity. The mean number of previous drug treatments was 1.14±1.39. More than 60 percent (N=525) of the patients used a second substance of abuse, most commonly alcohol; 78.5 percent (N=412) of those patients reported alcohol abuse.
Of the 862 patients, 447 volunteered to participate in the study and 415 declined. In a previous paper we reported finding no differences between the volunteers and decliners in demographic characteristics, psychiatric symptomatology, addiction severity, or treatment retention (25). Of the 447 participants, 146 were randomly assigned to individual counseling, 151 to individual counseling plus group counseling, and the 150 to the intensive program. To evaluate the success of the randomization procedure, the three groups were compared on 91 intake variables. Only six differences occurred, which is approximately what might be expected by chance.
In-treatment and end-of-treatment results have been reported previously (1). Briefly, for patients who completed intake and returned for at least one treatment session, retention in individual counseling, in individual counseling plus group counseling, and in the intensive program was 42.7, 42.5, and 47.6 days, respectively. The 12-week program was completed by 20 percent of the patients in individual counseling, 20.4 percent of the patients in individual counseling plus group counseling, and 31.7 percent of the patients in the intensive program. These differences were not significant. Patients who remained in treatment did well and showed significant improvement from intake to the end of treatment on the alcohol, drug, legal, family, and psychological composite scores of the ASI; the number of days of cocaine use in the last 30 days; the BDI; and all scales of the SCL-90. Despite overall improvement, there were no significant differences on any in-treatment or end-of-treatment variables across the three treatment groups (1).
Nine-month follow-up data further supported the effectiveness of treatment retention in reducing drug use and associated problems. For the 316 of the 447 patients who were successfully followed up, those who had remained in treatment for six weeks or more were doing significantly better than those who had left earlier as indicated by their ASI employment, alcohol, drug, and psychological composite scores, as well as by their being more likely to have attended outpatient treatment, self-help meetings, and school and less likely to have been in jail (Table 1). They also reported fewer days of cocaine use in the last 30 days, and their urine drug screens were less likely to be positive for cocaine.
Follow-up was successfully completed for 102 patients (69.9 percent) of the 146 patients in individual counseling, 110 patients (72.4 percent) of the 151 patients in individual counseling plus group counseling, and 104 patients (69.3 percent) of the 150 patients in the intensive program. The differences in completion rates were not significant. Table 2 compares intake and follow-up ASI composite and RAB scores within and across the three treatment groups. Significant improvement was found on most of the variables within each modality. Once again, however, there were no differences in degree of improvement across the modalities.
To examine patient outcomes in relation to more specific lengths of stay, the 316 individuals for whom follow-up data were obtained were placed in four comparably sized, mutually exclusive groups. The groups were those who dropped out before attending one treatment visit (N=79), those who entered treatment but remained for less than four weeks (N=81), those who remained more than four weeks but did not complete the program (N=93), and those who completed 12 weeks of treatment (N=63).
As Table 3 shows, the results were similar to those described above and again indicated that longer retention, regardless of treatment modality, was associated at follow-up with fewer drug problems, a smaller proportion of cocaine-positive urine tests, a better employment status, and fewer psychological problems. Those who spent more time in treatment were also more likely to be attending self-help meetings, continuing in outpatient treatment, or attending school.
The likelihood of being interviewed for follow-up increased with length of stay in treatment; 64 percent of patients who dropped out before one treatment visit were interviewed at follow-up, compared with 66 percent of patients who remained in treatment less than four weeks, 75.2 percent of patients who remained five to 12 weeks, and 81.8 percent of patients who completed 12 weeks of treatment. Thus if those who were not found were not doing as well as those who were found, the differences reported above would be even more impressive.
As for AIDS risk behavior, the mean intake RAB score of 8.54±4.83 for the 285 patients for whom data were available decreased significantly to 7.67±4.49 (t=2.86, df=284, p<.005) at nine-month follow-up. The degree of improvement was not associated with time in treatment (r=.09, ns). Nevertheless, as Table 4 shows, follow-up RAB scores were related to substance use, and, more important, improvement in risk behavior was related to decreased substance use. Thus individuals whose risk behaviors decreased were those whose substance use had decreased.
Discussion and conclusions
Intensive outpatient treatment was rapidly embraced during the last decade to provide care for patients who did not meet criteria for inpatient or residential treatment but who were judged to need more than one session of outpatient counseling a week, which seemed to provide too much time for temptation and relapse between visits. The purpose of the study reported here was to compare this new modality with the more traditional treatments of individual counseling and individual counseling plus group counseling.
The research took place on the premises of, and with patients recruited from, an ongoing community-based, inner-city, publicly funded clinic operated and staffed according to policies and procedures common to public-sector outpatient substance abuse programs. Coming from this context, the findings could be seen as more closely relevant and judged more acceptable by clinical service providers. Most patients in the study were African American, unmarried, and unemployed. Although this setting and group need to be studied to determine what treatment services might be most appropriate and helpful, the results might be limited in generalizability and not be applicable to other settings and groups.
The study design was a randomized controlled trial. The three treatments being compared were roughly equal in resource utilization, each requiring nine or ten staff hours per week for nine patients. Follow-up was conducted by an independent contractor.
Regardless of the treatment modality, patients improved significantly from intake to follow-up with respect to drug use, severity of problems associated with drug use, and AIDS risk behavior. Remaining in treatment longer was associated at follow-up with fewer drug problems, a smaller proportion of positive urine drug tests, a better employment status, and fewer psychological problems. Those who spent more time in treatment were more likely to be attending self-help meetings, continuing in outpatient treatment, or attending school. However, no significant differences were found between the treatment modalities on any in-treatment, end-of-treatment, or follow-up variable.
Although RAB scores decreased from intake to follow-up, the decrease was not related to time in treatment. However, the decrease in RAB scores was related to decreased drug use. Apparently, improvement in risk behaviors required not only remaining in treatment but also active involvement in treatment and improvement as indicated, for example, by decreased drug use.
Despite the findings on improvement in relation to time in treatment, we are limited in our ability to propose a causal relationship between treatment and outcome because we did not randomly assign subjects to different lengths of treatment. Retention, then, could be an effect of treatment, of "better motivated" patients' staying longer, or of both in some combination. Nevertheless, the results are encouraging; it does appear that individuals who remain in treatment longer do have better outcomes.
Earlier studies reported significant improvement among patients in varieties of intensive outpatient treatment (9,10), although Campbell and associates (9) emphasized the need for controlled comparisons. McLellan and colleagues (11) compared the intake characteristics, treatment services received, and outcomes of six samples of patients in intensive outpatient programs and ten samples in traditional outpatient programs selected from their national database of "real-world" treatment programs. At six-month follow-up, the patients in both modalities had improved significantly, but the intensive programs were not associated with more improvement compared with the traditional programs. The randomized controlled study reported here did not show that a model of intensive outpatient programming involving nine hours of group and activity sessions per week was more effective than traditional one-hour-a-week individual counseling.
Researchers commonly express unhappiness with the "research-clinical gap." They tend to be inpatient about the length of time often taken by clinicians to accept their results and translate them into clinical practice. One might note that "clinical-research gaps" also occur. Based on clinical observations and writings, intensive outpatient treatment appeared promising and was rapidly accepted into common practice. This growth occurred, however, without a basis of research support, and, indeed, the comparisons recently reported by McLellan and associates (11) and Weinstein and colleagues (1) did not show any advantage for intensive over traditional modalities of treatment.
Our results are limited to the model of intensive outpatient treatment program we instituted and studied. We do not suggest that intensive outpatient treatment is not useful or helpful but only that its effectiveness has not yet been demonstrated. Many models for intensive treatment are possible, and they may differ in the frequency and number of visits, the length of visits, the approach to treatment, and the number and varieties of services and modalities used.
Clearly many more controlled comparisons of different models are needed. In all likelihood, the issue of matching will again be paramount, and when enough information becomes available, the question will not be whether intensive or traditional treatment is better but which patients do better in which variations of intensive and traditional programs. In the meantime, intensive outpatient treatment is well established clinically, while the research story remains to be told (26).
Acknowledgments
This research was partly supported by grant 1-R18-DA-06166 from the National Institute on Drug Abuse and performed under the auspices of the Commonwealth Office of Drug and Alcohol Programs and the Philadelphia Department of Public Health, Coordinating Office for Drug and Alcohol Abuse Programs.
The authors are affiliated with the department of psychiatry and human behavior at Jefferson Medical College, Thomas Jefferson University, 1201 Chestnut Street, 15th Floor, Philadelphia, Pennsylvania 19107. An earlier version of this paper was presented at the annual meeting of the American Psychiatric Association held May 17-22, 1997, in San Diego.
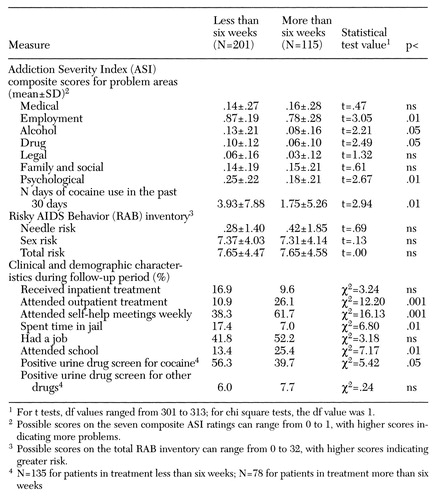 |
Table 1. Measures of functioning at nine-month follow-up for patients in three 12-week cocaine treatment programs who remained in treatment less than six weeks and more than six weeks
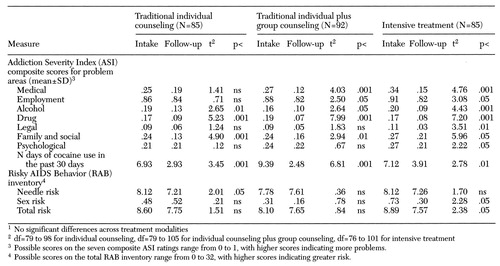 |
Table 2. Mean intake and follow-up scores on measures of functioning for patients with cocaine use disorder in two traditional outpatient treatment modalities and intensive outpatient treatment1
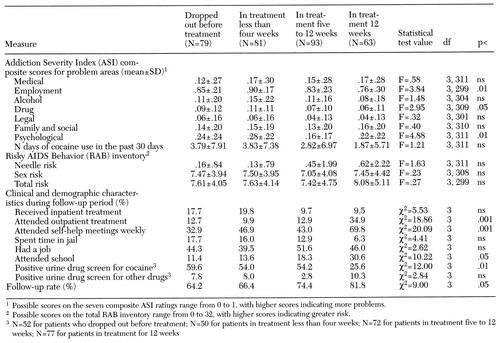 |
Table 3. Measures of functioning at nine-month follow-up for patients in three 12-week cocaine treatment programs, by the amount of time patients remained in treatment
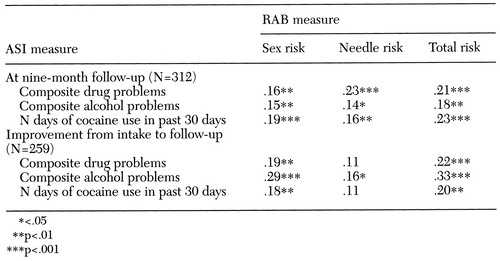 |
Table 4. Correlations between measures on the Addiction Severity Index (ASI) and Risky AIDS Behavior (RAB) inventory at nine-month follow-up and improvement in those measures from intake to follow-up for patients in three cocaine treatment programs
1. Weinstein SP, Gottheil E, Sterling RC: Randomized comparison of intensive outpatient vs individual therapy for cocaine abusers. Journal of Addictive Diseases 16:41-56, 1997Crossref, Medline, Google Scholar
2. Washton AM: Cocaine Addiction: Treatment, Recovery, and Relapse Prevention. New York, Norton, 1989Google Scholar
3. Washton AM: Evolution of intensive outpatient treatment (IOP) as a "legitimate" treatment modality (edtl). Journal of Addictive Diseases 16:xix-xxv, 1997Google Scholar
4. Patient Placement Criteria for the Treatment of Psychoactive Substance Use Disorders. Washington, DC, American Society of Addiction Medicine, 1991Google Scholar
5. Kang SY, Kleinman PH, Woody GE, et al: Outcomes for cocaine abusers after once-a-week psychosocial therapy. American Journal of Psychiatry 148:630-635, 1991Link, Google Scholar
6. McAuliffe WE, Albert J: Clean Start: An Outpatient Program for Initiating Cocaine Recovery. New York, Guilford, 1992Google Scholar
7. Rawson RA: The Neurobehavioral Treatment Model: An Outpatient Model for Cocaine Addiction Treatment. Beverly Hills, Calif, Matrix Center, 1989Google Scholar
8. Wallace BC: Crack cocaine: what constitutes state of the art treatment? Journal of Addictive Diseases 11:79-95, 1991Google Scholar
9. Campbell J, Gabrielli W, Laster LJ, et al: Efficacy of outpatient intensive treatment for drug abuse. Journal of Addictive Diseases 16:15-25, 1997Crossref, Medline, Google Scholar
10. Campbell WG: Evaluation of a residential program using the Addiction Severity Index and stages of change. Journal of Addictive Diseases 16:27-39, 1997Crossref, Medline, Google Scholar
11. McLellan AT, Hagan TA, Meyers K, et al: "Intensive" outpatient substance abuse treatment: comparisons with "traditional" outpatient treatment. Journal of Addictive Diseases 16:57-85, 1997Crossref, Medline, Google Scholar
12. Milcom. Libertyville, Ill, Hollister, Milcom Systems, 1989Google Scholar
13. Metzger DS, Woody GE, DePhillipis D, et al: Risk factors for needle sharing among methadone-treated patients. American Journal of Psychiatry 148:636-640, 1991Link, Google Scholar
14. McLellan AT, Luborsky L, Cacciola J, et al: New data from the Addiction Severity Index: reliability and validity in three centers. Journal of Nervous and Mental Disease 173:412-423, 1985Crossref, Medline, Google Scholar
15. Beck AT, Steer RA: Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1986Google Scholar
16. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometrics, 1983Google Scholar
17. Gottheil E, McLellan AT, Druley KA: Reasonable and unreasonable methodological standards for the evaluation of alcoholism treatment, in Matching Patient Needs and Treatment Methods in Alcoholism and Drug Abuse. Edited by Gottheil E, McLellan AT, Druley AK. Springfield, Ill, Thomas, 1981Google Scholar
18. Beck AT: Cognitive Therapy and the Emotional Disorders. New York, International Universities Press, 1976Google Scholar
19. Marlatt GA, Gordon JR: Relapse Prevention. New York, Guilford, 1985Google Scholar
20. Rounsaville BJ, Gawin FH, Kleber HD: Interpersonal psychotherapy adapted for ambulatory cocaine abusers. American Journal on Drug and Alcohol Abuse 11:171-191, 1985Crossref, Medline, Google Scholar
21. Washton AM: Outpatient treatment techniques, in Cocaine: A Clinician's Handbook. Edited by Washton AM, Gold MJ. New York, Guilford, 1987Google Scholar
22. Kleber HD, Gawin FH: Cocaine abuse: a review of current and experimental treatments. National Institute on Drug Abuse Research Monograph 50:111-129, 1984Google Scholar
23. Millman RB: Evaluation and clinical management of cocaine abusers. Journal of Clinical Psychiatry 49(Feb suppl):27-33, 1988Google Scholar
24. O'Brien CP, Childress AR, Arndt IO, et al: Pharmacological and behavioral treatments of cocaine dependence: controlled studies. Journal of Clinical Psychiatry 49(Feb suppl):17-22, 1988Google Scholar
25. Gottheil E, Sterling RC, Weinstein SP: Generalizing from controlled treatment outcome studies: sample data from a cocaine treatment program. American Journal on Addictions 4:331-338, 1995Google Scholar
26. Gottheil E. Intensive outpatient treatment: methods and outcomes. Journal of Addictive Diseases 16:xv-xix, 1997Google Scholar



