Substance Use and Psychiatric Problems of Homeless Native American Veterans
Abstract
OBJECTIVE: This study estimated the proportion and representation of Native Americans among homeless veterans and compared their psychiatric and substance abuse problems with those of other ethnic groups of homeless veterans. METHODS: The study was based on data from the Department of Veterans Affairs' Health Care for Homeless Veterans program, a national outreach program operating at 71 sites across the country. Alcohol, drug, and psychiatric problems of Native American veterans (N=950) reported during intake assessment were compared with problems reported by white, black, and Hispanic veterans (N=36,938). RESULTS: Native Americans constituted 1.6 percent of veterans in the program. Age-adjusted analyses suggested that relative to the general veteran population (of which 1.3 percent are Native Americans), Native Americans are overrepresented in the homeless population by approximately 19 percent. Regression analyses controlling for demographic characteristics found that Native American veterans reported more current alcohol abuse, more previous hospitalizations for alcohol dependence, and more days of recent alcohol intoxication than members of other ethnic groups. In contrast, Native American veterans reported fewer drug dependence problems than other minority groups and fewer current psychiatric problems and previous psychiatric hospitalizations than the reference group of white homeless veterans. CONCLUSIONS: Native Americans are overrepresented in the homeless veteran population. They have more severe alcohol problems than other minority groups but somewhat fewer psychiatric problems.
Although homelessness among some ethnic minority groups in the United States has been the subject of systematic empirical study (1,2,3), no studies have examined the problems faced by homeless Native Americans. Because Native Americans constitute a small portion of the U.S. population, .79 percent (4), previous studies of homelessness and related problems among minority groups have not included separate analyses of this group.
The Department of Veterans Affairs Health Care for Homeless Veterans program conducts outreach to more than 20,000 homeless veterans per year at 71 sites across the country (5). Sufficient numbers of homeless Native American veterans have been contacted through this program to allow subgroup analyses of the characteristics and service needs of this neglected population.
Native Americans have experienced a long history of social disadvantage, and their disproportionate substance abuse and psychiatric problems have been well documented (6). Alcohol-related mortality and hospitalization for alcoholism are higher in Native American populations than in the U.S. general population (7). Psychiatric illness, such as major depression, has also been observed to be higher in some Native American populations (8).
However, Native Americans may not experience uniformly more substance use and psychiatric problems than other groups. A recent study by Howard and associates (9) of inpatient treatment for substance use and psychiatric problems showed that Native American veterans were more likely to have been treated for alcohol-related disorders than other veterans, but they were no more likely than other veterans to have been treated for drug or psychiatric problems. Substance abuse and psychiatric problems among Native Americans need to be studied in relation to such problems among other groups.
The purpose of the study presented here was, first, to estimate the proportion and representation of Native Americans among homeless veterans. Second, it examined their distinctive demographic characteristics and mental health problems. Increasing our understanding of differences between ethnic groups on these measures will aid in the identification of gaps in mental health services and contribute to the planning of services targeted for this vulnerable population.
Methods
Sample
Three samples of veterans were analyzed in the current study. The first sample included veterans contacted by the Department of Veterans Affairs Health Care for Homeless Veterans (HCHV) program at all 71 sites between February 1, 1992, and September 30, 1996 (N=69,892). The second sample encompassed veterans from the general population who were interviewed for the 1992 National Survey of Veterans (N=11,603) (10). Ethnocultural characteristics of these two samples were compared to estimate the over- or underrepresentation of Native Americans in the homeless population relative to the general veteran population.
The third sample consisted of veterans in the HCHV program from only those sites having at least ten veterans who were Native Americans. This group, a subsample of the larger HCHV group noted above, included veterans from 35 HCHV sites (N= 36,938), 950 of whom were Native Americans. Analyses of demographic characteristics, substance abuse problems, and psychiatric problems were limited to this subsample in an effort to control for regional variations in these measures that might confound ethnocultural comparisons.
Study instrument and data collection
Data were obtained during intake interviews with homeless veterans entering the HCHV program. Trained program clinicians, predominantly social workers and nurses, individually administered a structured interview during outreach visits in community locations such as shelters and soup kitchens. Specific measures were taken to ensure privacy and confidentiality. A typical interview lasted 20 minutes, with additional time taken by the clinician after the interview to construct diagnoses.
The 87-item interview gathered self-report data in several areas, including information about demographic characteristics, military history, current living and employment situation, and medical and psychiatric problems. It also included a section to record clinical psychiatric diagnoses based on DSM-IV criteria (11). These diagnoses were derived from unstructured assessments and were therefore based on clinical judgment.
Data in three areas described below were selected for analyses.
Background characteristics.
All information in this section came from the veteran's self-report. Demographic information included ethnicity (white, black, Hispanic, or Native American-Alaska Native), sex, age, and marital status. Information about the veteran's military history included service era (ranging from pre-World War II to the Persian Gulf) and whether the veteran had been exposed to fire in a combat zone. Information on residence and employment situation included type of residence at the time of the interview, receipt of public support payments, and number of days worked in the 30 days before the interview.
Alcohol and drug use.
The assessment included four measures of alcohol use that were then repeated to assess drug use. Three came from the veteran's self-report. The item on current alcohol dependency asked, Do you have a problems with alcohol dependency now? The item on history of hospitalization for alcoholism asked, Have you been hospitalized for the treatment of alcoholism? The number of days that the veteran drank to intoxication in the past month was arrived at by asking, During the past 30 days, how many days would you say that you drank to the point of intoxication?
In addition to these self-report measures, an item was included to record the clinician's diagnosis (yes-no) of current alcohol abuse or dependence. Measures containing the same wording were used to assess drug use.
Psychiatric problems.
Five measures of psychiatric problems were obtained, two from the veteran's self-report and three based on the interviewer's diagnosis. The self-report items were constructed in a form similar to the substance use items. One addressed current psychiatric problems: Do you think you have any current psychiatric or emotional problems other than alcohol or drug use? The other addressed history of hospitalization: Have you ever been hospitalized for a psychiatric problem not including substance abuse treatment? Interviewers diagnosed the presence of a severe psychiatric disorder (any schizophrenia disorder, another psychotic disorder, or posttraumatic stress disorder). A dual diagnosis variable was constructed by a combination of the diagnosis of serious psychiatric disorder and the diagnosis of substance dependence.
Data analysis
Bivariate correlations between the dependent diagnostic variables and demographic characteristics were reviewed to select the most relevant variables for adjustment of the ethnic comparisons. These variables are listed in Table 1. Logistic regression (on dichotomous dependent variables) or linear multiple regression (on continuous dependent variables) was then conducted. The independent variable of interest was ethnic group membership (dummy variables coded for black, Hispanic, and Native American, with white as the reference group). Control variables were included as follows: sex (dummy variable for female gender), age at time of interview (continuous), marital status (coded 1 if married), Vietnam service era (coded 1 if yes), experience of combat fire (coded 1 if yes), literal homelessness (coded 1 if residence at the time of the interview was a shelter or the street), receipt of public support (coded 1 if the veteran was currently receiving service-connected disability payments, non-VA disability payments, a non-service-connected pension, or other public support), and days worked in the past month (continuous).
Results
Proportion of Native Americans
The proportion of Native Americans in the HCHV program sample was compared with the estimated proportion of Native Americans in the general veteran population based on data in the 1992 National Survey of Veterans (10). Because the age distributions of the two samples differed, the comparison was adjusted using the age distribution of the HCHV program population as the standard (12). The HCHV program intake sample included 1.56 percent Native Americans. The age-adjusted estimated percentage of Native Americans in the general veteran population was 1.31 percent. This comparison suggests that approximately 19 percent (1.56/1.31) more Native Americans are in the homeless population than would be expected, given the proportion of Native Americans in the general population and the age structure of the HCHV program population. The difference between these proportions was significant (z=2.01, p= .044).
Sample characteristics
The first section of Table 1 summarizes information on eight important demographic or background characteristics for which significant differences were found among the ethnic groups. These variables were used to statistically adjust comparisons between ethnic groups on all of the dependent measures.
Alcohol dependence measures
Table 1 also lists descriptive results from clinical measures of alcohol abuse. Analyses of comparisons of ethnic groups on variables related to alcohol problems are shown in Table 2. The differences between groups shown in Table 2 were fairly consistent over the four measures, with Native American homeless veterans reporting significantly and substantially greater alcohol-related problems than the other groups.
Relative to the white reference group, blacks were significantly less likely and Native Americans were significantly more likely to indicate current alcohol abuse. Similarly, Native Americans reported significantly more days of drinking to intoxication than whites (5.4 and 3.9 days, respectively). Relative to whites, blacks and Hispanics were significantly less likely to report previous hospitalization for alcohol problems, while Native Americans were significantly more likely to report such hospitalization. These self-report measures were consistent with the clinician's diagnosis of dependence. Compared with whites, blacks were significantly less likely and Native Americans significantly more likely to be judged alcohol dependent. On each of the measures of alcohol abuse, the proportion of Native Americans was about 40 percent greater than the proportion of the white reference group.
Drug dependence measures
The pattern of ethnic differences on drug dependence measures was quite different from that observed for alcohol dependence. As Table 2 shows, Native American homeless veterans were significantly less likely than whites to indicate current drug abuse, while blacks were almost three times more likely and Hispanics were more than two times more likely than whites to indicate current abuse. Native Americans reported the fewest mean number of days of drug use (1.6 days), while blacks reported the most days (4.3 days). Native Americans did not differ from whites on this measure.
The percentage of Native Americans reporting previous hospitalization for drug dependence was lower than for all other ethnic groups (22.3 percent); the highest percentage was among blacks (45.8 percent). Native Americans also had the lowest percentage of diagnoses of drug dependence (24.6 percent), while blacks had the highest (55.8 percent). Relative to the white reference group, blacks were more than three times as likely and Hispanics were more than two times as likely to be judged drug dependent by the interviewing clinician, while Native Americans did not differ from whites on this measure. Thus compared with white veterans, on all four measures of drug dependence, blacks and Hispanics showed a consistent pattern of greater dependence and Native Americans a nonsignificantly lower level of dependence.
Psychiatric problem measures
As shown in Table 3, the percentage of homeless veterans in the sample indicating current psychiatric problems was high, 46.5 percent overall. The prevalence of such reports was lowest among Native Americans (41 percent) and highest among Hispanics (50.1 percent). Native Americans and blacks were significantly less likely to report current psychiatric problems than whites (34 percent and 25 percent less likely, respectively). A similar pattern was observed for reports of previous psychiatric hospitalization. Native Americans had the lowest percentage of such reports (24.5 percent), while whites had the highest (33.8 percent). All ethnic minorities were less likely to report previous hospitalization than whites; Native Americans were 49 percent less likely, Hispanics 33 percent less likely, and blacks 17 percent less likely.
Clinicians' ratings of serious psychiatric problems were least prevalent among Native Americans (40.6 percent) and most prevalent among Hispanics (48.5 percent). Blacks and Native Americans were significantly less likely than whites to be diagnosed as having these problems. Blacks and Hispanics were significantly more likely than whites to receive a dual diagnosis, although the magnitude of the difference was small (8 percent and 15 percent, respectively). Finally, on mean number of psychiatric diagnoses, Native Americans had significantly fewer psychiatric disorders than whites (1.7 versus 1.8 disorders), while blacks and Hispanics had significantly more (1.9 in each group); however, the differences were small. In summary, consistently fewer Native Americans than whites presented with psychiatric problems at intake. The pattern was less consistent for black and Hispanic veterans.
Discussion and conclusions
This study addressed two questions. First, are Native American veterans over- or underrepresented in the homeless veteran population? The answer appears to be that Native Americans are somewhat overrepresented. An age-controlled comparison of veterans in the Health Care for Homeless Veterans program to a sample of the general veteran population suggested that there are about 19 percent more Native American veterans in the homeless population than would be expected. This estimate is likely to be conservative because the national survey includes veterans from both urban and rural areas, while the homeless sample includes veterans predominantly from urban areas. More Native Americans tend to be in rural areas than urban areas. Had the comparison of the national sample and the homeless sample adjusted for geographic differences, the difference in the proportion of Native Americans might have been even higher.
The second question asked by this study was, What are the alcohol-dependence, drug-dependence, and psychiatric problems presented by homeless Native American veterans, and how are they different from those presented by members of other ethnic groups? The answer is that homeless Native American veterans, like other homeless veterans, have high levels of mental health problems and substance abuse problems. However, compared with other ethnocultural groups, their problems are mainly alcohol related. Consistently, Native Americans were about 40 percent more likely than whites to report problems with alcohol abuse, previous hospitalization for alcoholism, and more days intoxicated.
The prevalence of a clinician's diagnosis of alcohol dependence among Native Americans was also about 40 percent higher than among whites. At the same time, Native Americans were no more likely than whites to have drug abuse or dependence, and they were significantly less likely to report psychiatric problems or previous hospitalization or to be diagnosed by the clinician as having a serious psychiatric disorder. This pattern among Native Americans contrasts sharply with those among blacks and Hispanics, whose problems centered around drug dependence rather than alcohol.
Although comparisons of this type are useful, we reiterate that the majority of veterans in this study are extremely disadvantaged and that the overall prevalence of substance use and psychiatric disorders was quite high.
These results are consistent with those of Howard and colleagues' study (9) of substance-abuse-related VA hospital admissions. Like the study reported here, that study found that Native American veterans were more likely than others to be admitted with a diagnosis of an alcohol-related disorder and less likely to be admitted with a drug-related diagnosis or other psychiatric diagnoses. Similarly, Westermeyer and Neider (13) noted that Native Americans admitted to a substance abuse treatment program were more likely to have a diagnosis of alcohol dependence or alcohol dependence plus drug dependence; that is, they were less likely to have a diagnosis of drug dependence only. The study reported here extends this pattern of results to the homeless veteran population and adds controls for potentially confounding demographic characteristics.
The nature of the alcohol abuse and dependence observed in this study is not clear. Native Americans reported both more days intoxicated in the past month (Table 2) and more days using any alcohol (results not shown). Previous studies have argued that the predominant form of alcohol abuse in at least some Native American tribes is "binge drinking" (14). Moreover, Levy and Kunitz (15) found a higher percentage of abstainers in their study of the Navajo population relative to the general population. In this study, Native Americans were less likely than other veterans to abstain from alcohol (results not shown). Thus insufficient behavioral data were gathered to elaborate on the veterans' self-reports of current alcohol abuse.
Several limitations of the study must be noted. First, these data are based only on veterans who were contacted by the HCHV program for treatment and case management; they may not represent the entire population of homeless veterans. Second, the data are based on self-report and clinicians' impressions. The possibility of bias in reporting must be acknowledged. Because of the history of alcohol misuse among Native Americans, veterans in this group may be more aware of their alcohol problems or may be more willing to report them than veterans in other ethnic groups. Similarly, the interviewing clinician may be more likely to record an impression of alcohol dependence for a Native American due to sensitization or stereotyping.
Third, the measures of alcohol, drug, and psychiatric problems used in this study were based on single items rather than fully developed assessment scales. Thus they depend heavily on face validity. However, the extremely large number of individuals included in the study may have minimized the impact of these problems. That is, such biases would have to be consistently applied by dozens of independent clinicians to almost a thousand Native American veterans for the results reported here to be affected.
This study has documented a specific pattern of a high level of alcohol problems and a relatively low level of drug and psychiatric problems among homeless Native American veterans. The results argue for providing preventive treatment services targeted toward alcohol abuse to this population. Further work should be directed toward assessing the appropriateness and effectiveness of services for this population, as well as the relevance of specific culturally sensitive services.
Acknowledgments
The ongoing evaluation of the Health Care for Homeless Veterans program is funded by the Department of Veterans Affairs. The authors thank Janine Chapdelaine, M.A., and Loretta Manware for assistance with data collection and Jane Tollett for discussions that motivated this research.
The authors are affiliated with the Northeast Program Evaluation Center of the Department of Veterans Affairs and the department of psychiatry at Yale University School of Medicine in New Haven, Connecticut. Send correspondence to Dr. Kasprow at the VA Connecticut Health Care System (182), 950 Campbell Avenue, West Haven, Connecticut 06516. This research was presented at the annual meeting of the American Public Health Association held November 9-13, 1997, in Indianapolis.
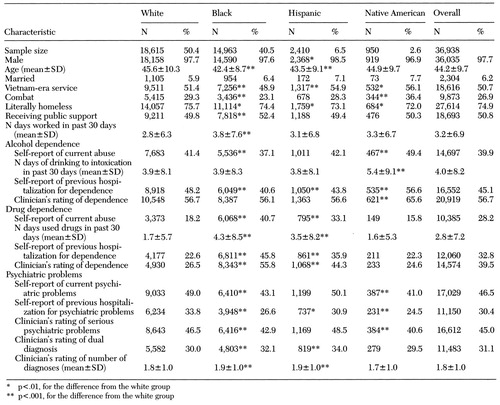 |
Table 1. Characteristics of veterans in the Health Care for Homeless Veterans program, by ethnic group
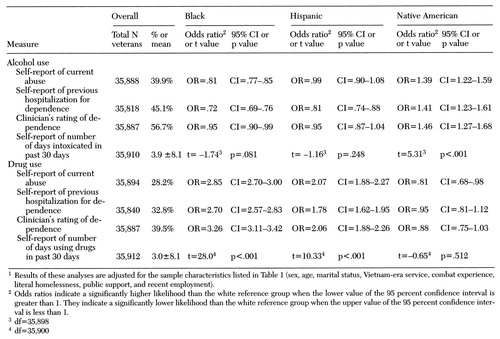 |
Table 2. Differences between ethnic groups of homeless veterans on alcohol- and drug-related measures1
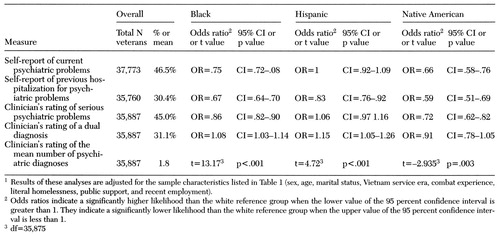 |
Table 3. Differences between ethnic groups of homeless veterans on measures of psychiatric problems1
1. Hopper K, Milburn NG: Homelessness among African-Americans: a historical and contemporary perspective, in Homelessness in America. Edited by Baumohl J. Phoenix, Ariz, Oryx Press, 1996Google Scholar
2. Roth D, Toomey BG, First RJ: Gender, racial, and age variations among homeless persons, in Homelessness: A National Perspective. Edited by Robertson MJ, Greenblatt M. New York, Plenum, 1992Google Scholar
3. Leda C, Rosenheck RA: Race in the treatment of homeless mentally ill veterans. Journal of Nervous and Mental Disease 183:529-537, 1995Crossref, Medline, Google Scholar
4. 1990 Census of Populations: Population Characteristics. Washington, DC, US Bureau of the Census, 1993Google Scholar
5. Kasprow WJ, Rosenheck R, Chapdelaine JD: Health Care for Homeless Veterans: Tenth Annual Report. West Haven, Conn, Northeast Program Evaluation Center, 1997Google Scholar
6. Lamarine RJ: Alcohol abuse among Native Americans. Journal of Community Health 13:143-155, 1988Crossref, Medline, Google Scholar
7. Mail PD, Johnson S: Boozing, sniffing, and toking: an overview of the past, present, and future of substance use by American Indians. American Indian and Alaska Native Mental Health Research 5:1-33, 1993Crossref, Medline, Google Scholar
8. Nelson SH, McCoy GF, Stetter M, et al: An overview of mental health services for American Indians and Alaska Natives in the 1990s. Hospital and Community Psychiatry 43:257-261, 1992Abstract, Google Scholar
9. Howard MO, Walker RD, Suchinsky RT, et al: Substance-use and psychiatric disorders among American Indian veterans. Substance Use and Misuse 31:581-598, 1996Crossref, Medline, Google Scholar
10. National Survey of Veterans. Washington, DC, Department of Veterans Affairs, 1995Google Scholar
11. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
12. Rothman KJ: Modern Epidemiology. Boston, Little, Brown, 1986Google Scholar
13. Westermeyer J, Neider J: Substance disorders among 100 American Indian versus 200 other patients. Alcoholism: Clinical and Experimental Research 18:692-694, 1994Crossref, Medline, Google Scholar
14. Westermeyer J: Opinions regarding alcohol use among the Chippewa. American Journal of Orthopsychiatry 42:398-403, 1972Crossref, Medline, Google Scholar
15. Levy JE, Kunitz SJ: Indian Drinking: Navajo Practices and Anglo-American Theories. New York, Wiley, 1974Google Scholar



