Does Outreach Case Management Improve Patients' Quality of Life?
Abstract
OBJECTIVE: This study examined whether enhancing standard aftercare with an outreach case management intervention would improve patients' quality of life. METHODS: A sample of 292 patients discharged from an inpatient psychiatry service at an urban general hospital were randomly assigned either to an intervention group (N=147), which received outreach case management services in addition to standard aftercare service, or to a control group (N=145), which received only standard aftercare services. The follow-up period was 15 to 52 months. Individuals in both groups were reinterviewed by an independent research team about 21.6 months after discharge. The groups were compared using 39 measures of quality of life. The interviews elicited information about patients' physical well-being and competence in performing activities of daily living; their emotional well-being as shown in emotional expressiveness, sadness, suicidal thoughts, and substance abuse; and their interpersonal relationships, living arrangements, friendships, income maintenance, and employment. RESULTS: No difference was found between the groups on any of the quality-of-life variables. CONCLUSIONS: Outreach case management was not associated with improved quality of life.
Since the 1970s outreach case management has been generally accepted as an effective means of providing support services to deinstitutionalized psychiatric patients (1). In such approaches, an individual case manager or a case management team negotiates for, coordinates, and advocates for mental health care, medical care, housing, income maintenance, and other services that patients need (1,2,3,4). Although it has been tacitly assumed that outreach case management would reduce psychiatric rehospitalization rates, improve social functioning and health care, and possibly reduce mortality, until recently these assumptions have not been subjected to critical and scientific review.
Two previous studies in our department of psychiatry showed that a group of 147 patients receiving outreach case management for periods ranging from 15 to 52 months after leaving the hospital did not have lower rehospitalization rates or better mortality outcomes than a comparable control group of 145 patients who received routine aftercare services but no outreach case management (5,6). From October 1, 1985, through June 30, 1988, a total of 48 of the 147 patients in the intervention group (32.6 percent) were rehospitalized at Harlem Hospital Center, whereas only 22 of the 145 control group patients (15.2 percent) were rehospitalized (χ2=11.30, df=1, p<.001) (5).
Of the total group of 292 patients, 21 (7.2 percent) died during the study period. About half of these deaths were above the expected number based on the overall mortality rate in Central Harlem in 1986 (6), an area known to have much excess mortality compared with the U.S. overall (7). The 7.5 percent mortality rate in the intervention group (11 patients) and the 6.9 percent mortality rate in the control group (ten patients) did not significantly differ. Both groups had the same pattern of cause of death, to which substance abuse contributed heavily. Death from suicide in Central Harlem was 4.9 per thousand in 1986 (8). Both study groups had suicide rates considerably higher than expected. In the intervention group, one death was a suicide, and two others were suspected suicides; in the control group, two deaths were suicides (6).
In our previous reports (5,9), we emphasized that case management has been variously defined. Our form of case management is different from two other commonly used models: assertive case management and brokered case management. As we define it, case management differs from assertive community treatment (10,11) in that it is only one component of a complete community treatment program. Our form of case management has been inaccurately equated with the brokered case management model (12). However, it does not include the purchase of services for patients, the central element of the brokered model.
A distinctive feature of the case management intervention in this study was the high level of professional involvement with patients and families. The case management team consisted of an attending psychiatric consultant, a certified social worker, and a physician assistant, as well as traditional case managers who were community liaison workers. This was a high level of staffing (12), aimed at facilitating referral to aftercare services to carry out the treatment plan formulated at the time the patient was discharged.
Case management services were designed to implement the plan and to continue monitoring patients' physical health problems, psychological status, family and housing problems, and social service needs. The team's mission was to help the patient enroll in and attend an appropriate ambulatory care service, such as our day hospital, adult mental health clinic, rehabilitation day treatment center, or alcohol treatment program. For patients who were unwilling or unable to comply with the treatment plan, the team provided home-based or other interim treatment until the patient accepted the usual aftercare services. We were thereby providing a unique form of case management.
In this study, we examined whether or not certain aspects of quality of life were improved for patients who received outreach case management compared with a control group. Specifically, data from follow-up research interviews were used to compare patients' reported sense of improvement in physical well-being and competence in performing activities of daily living; in emotional well-being as shown in emotional expressiveness, sadness, suicidal thoughts, and substance abuse; and in interpersonal relationships, living arrangements, friendships, income maintenance, and employment.
Methods
Setting
The study site was described in a previous report (5). Briefly, at the time the study began (1984-1985), the Harlem Hospital Center department of psychiatry was the only full-service psychiatric facility for the 250,000 residents of Central Harlem. Its patient population was low income, and about 90 percent African American and 6 percent Hispanic. Each day ten to 20 patients entered our emergency room; almost three-quarters had substance abuse problems, with or without additional psychopathology. At least half required inpatient admission; however, our 47 inpatient beds allowed only two or three admissions a day.
When the study began, more than 95 percent of our inpatient admissions were emergency and involuntary, meaning the patients were assessed as being a danger to self or others. After a customary average stay of 22 days, about 80 percent were referred to an ambulatory care program provided by our department. Around 20 percent failed to keep a single follow-up appointment, and an estimated 50 percent left ambulatory care after one month.
Selection criteria
For this study we excluded patients who did not reside in Manhattan, who were not between the ages of 18 and 64, whose only axis I diagnosis was substance abuse or organic mental disorder, and who stayed in the hospital less than seven days. Also excluded were patients who were already entitled to receive limited case management services from another agency due to the chronicity of their illness.
The remaining patients were randomly assigned to either the case management group (N=147) or the control group (N=145). All patients were enrolled between April 1984 and September 1985. All gave informed consent to participate in the study.
Study plan
The study can be described as a randomized prospective intervention study. The period of postdischarge case management services for patients in the intervention group ranged from 15 to 52 months depending on the date of discharge. The follow-up interval was the same for both groups, because equal random assignments to the groups were made during the same weeks throughout the study period.
After completion of the study, a case manager was retained on staff to continue to maintain services for patients in the intervention group who desired such services. No patient was discharged from the intervention group. The control group patients had no contact with the case management team after their index discharge from the hospital. Patients in both groups were referred to appropriate aftercare treatment programs for medical, psychiatric, substance abuse, and social problems.
The case management services provided by our team to the intervention group are more completely described in previous reports (5,6). Briefly, as noted above, the case management team provided home-based or other interim treatment until the patient accepted the usual aftercare services.
Evaluation interview procedure
Outreach case management team members were not involved in follow-up interviews of patients in the intervention or control groups. The research interviewer team consisted of three paraprofessional community liaison workers supervised by two of the authors (ELS and AD'E).
Locating study patients in the community for reinterview was a complicated and labor-intensive activity. Many patients in both the intervention and the control groups lacked a valid address. To find patients, the interviewers reviewed the data on patients at baseline; monitored all psychiatric treatment facilities of Harlem Hospital; made informal inquiries in Central Harlem; made on-line inquiries on the shared medical systems computer billing system; visited shelters, prisons, and voluntary municipal and state treatment facilities (residential and nonresidential facilities both inside and outside hospital centers); and searched archival databases for records of inpatients treated at facilities of the Health and Hospitals Corporation other than Harlem Hospital Center. Informed by these data, they visited each location in the community where patients may have either lived or visited (for example, for treatment) and recruited patients to be interviewed in a location satisfactory to the patient.
The patients were reinterviewed between 1986 and 1987. The mean± SD interval between index discharge and reinterview was 1.8±.6 years for the 113 intervention group patients and 1.8±.7 years for the 98 control group patients who were located in the community. Thus these 211 patients were reinterviewed 21.6±7.3 months after their index discharge, an average of 3.6 months later than the 18 months initially planned.
Measures
At baseline during the index hospitalization, all patients completed a client personal information form developed for this study. The 88-item questionnaire took about an hour to complete as administered by members of the case management team. It elicited extensive information used by the research interviewer team, including the patient's address and telephone number and the names and addresses of possible contacts.
In addition to information obtained during routine physical examinations and medical histories done for all inpatients, a special physician assistant form (PAF) was developed for use by the physician assistant on the case management team to gather information on various physical health problems experienced within the past year and in patients' lifetimes (13). The physician assistant was able to complete the PAF for 269 of the 292 patients (92.1 percent). He also reviewed current medical records, as well as records of previous hospitalizations on medical and surgical services.
Patients relocated by the research interviewer team were asked to complete an evaluation of aftercare form (EAF) for their care at Harlem Hospital Center. The form, also developed for this study, elicited information about the patients' biopsychosocial status (current and past) and living circumstances after discharge from the index hospitalization. This 150- to 200-item questionnaire took from one to two hours to complete as administered by research interviewers. The number of items varied due to the presence of probing items asked only when triggered by patients' responses.
The EAF elicited detailed information in the domains of physical and mental health status, hospitalization, aftercare, living situation, contacts with any service provider, entitlements, work experience, critical and disruptive life events, social network, activities of daily living, depressive symptom formation, suicidal behavior, drug use, and alcohol use. Within the EAF, depressive symptom formation was measured by a revised Center for Epidemiological Studies—Depression scale (14), drug use by a section of the Structured Clinical Interview for DSM-III (15,16), and alcohol use by the Short Michigan Alcoholism Screening Test (17).
In addition, the interviewers made 21 ratings based on what they learned about patients during the interview. These ratings included an estimate of the accuracy of the patient's answers to the interview questions and ratings of the patients' appearance, their general psychological status, whether they were under the influence of alcohol, and whether they would accept help from agencies and other services. A rating was also made of family members' role in the interview when they were present.
The EAF measures, which included the interviewer ratings, differed in scoring of responses depending on the area of inquiry. Thirty-nine items were selected for analysis as indicators of patients' quality of life.
Among reinterviewed subjects, two or three responses were missing in some areas covered by the client personal information form; they included employment, marital status, origin, and education. Ten reinterviewed patients in the control group and four in the intervention group were not interviewed at baseline by the physician assistant, not a statistically significant difference. Finally, eight responses to questions in the EAF about income were missing, four in each group.
Statistical power and methods
We used the normal curve test procedure (18) to estimate statistical power. The average sample size of our two groups of patients was 106. The size was sufficient to reject a false null hypothesis of no difference between any proportional measure of the two groups when the observed difference is moderate (two-tailed test, p=.05; power=.99), and also when the observed difference is midway between small and moderate (power=.81).
The distribution of nominal variables among the study groups was assessed for statistical significance (p<.05) with the chi square test. When the test had one degree of freedom, the continuity correction was applied unless otherwise noted. Student's t test with two tails was used for interval variables. To correct for increased type 1 error due to multiple comparisons of the intervention and control groups, which totaled 39, the least-significant-difference method (19) was used. Therefore, any single statistical test had to be significant at the .001 level (.05/39) to make an inference at the .05 level.
Results
Background characteristics
As we reported previously (5,6,8), baseline demographic and biosocial data were complete for 289 patients, of whom 211 were reinterviewed (73 percent). Of 146 patients in the intervention group, 113 were reinterviewed (77.4 percent), and of 143 patients in the control group, 98 were reinterviewed (68.5 percent), not a statistically significant difference.
Demographic and clinical characteristics of the reinterviewed patients in the intervention and control groups are shown in Table 1. The groups did not differ significantly in ethnicity, gender, age, education, entitlements, residential status, or clinical characteristics. Table 1 also shows that at baseline, the mean number of health problems for both groups was similar, as assessed by the PAF.
Follow-up interview
Patients in the intervention and control groups were compared on 39 measures of quality of life obtained in the reinterview. None of the comparisons were statistically significant when the least-significant-differences adjustment was applied (p<.001). Of the 13 measures for which the individual significance levels were lower than .05, six indicated higher quality of life in the intervention group, and seven indicated higher quality in the control group. (A report on the observed trends is available from the first author.) Therefore, we concluded that the quality of life of the patients in the intervention group was not demonstrably improved in comparison with the control group patients.
Discussion and conclusions
Quality of life was not demonstrably improved in a global sense for patients in the intervention group compared with those in the control group. However, because this study was of patients hospitalized at Harlem Hospital Center who were not eligible for community support services—that is, their illnesses were not regarded as chronic—these findings cannot be generalized either to patients in case management programs serving persons eligible for community support services or to patient populations whose biopsychosocial characteristics differ substantially from those of patients treated at Harlem Hospital Center.
Acknowledgments
This work was supported by a demonstration grant from the New York City Health and Hospitals Corporation, Robert Wood Johnson grant 09898, and a contract with the National Institute on Disability and Rehabilitation under grant G0085C3504. The authors acknowledge the valuable assistance of the late Sharon Horowitz in training and supervising the case management team and the research interviewers.
Dr. Curtis is director and Dr. Millman is research coordinator in the department of psychiatry at Harlem Hospital Center in New York City. Dr. Curtis is also clinical professor of psychiatry at Columbia University College of Physicians and Surgeons in New York City. Dr. Struening is director of the epidemiology of mental disorders research department at New York State Psychiatric Institute and associate professor at Columbia University School of Public Health. Dr. D'Ercole is adjunct associate professor in the department of psychology at New York University in New York City. Send correspondence to Dr. Millman, Harlem Hospital Center-Columbia University Affiliation, Department of Psychiatry, 506 Lenox Avenue WP-5, New York, New York 10037.
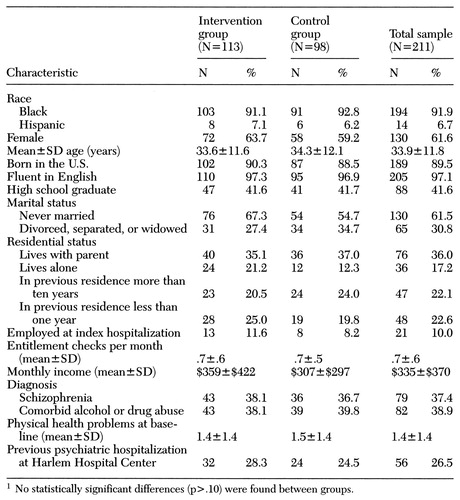 |
Table 1. Demographic and clinical characteristics of reinterviewed patients who received case management services (intervention group) and those who did not (control group) after discharge from Harlem Hospital Center1
1. Turner J, TenHoor W: NIMH community support program: pilot approach to a needed social reform. Schizophrenia Bulletin 4:319-348, 1978Crossref, Google Scholar
2. Langsley DG: Community psychiatry, in Comprehensive Textbook of Psychiatry, 3rd ed. Edited by Kaplan HL, Freedman AM, Sadock BJ. Baltimore, Williams & Wilkins, 1980Google Scholar
3. Shadish WR, Lurigio AJ, Lewis DA: After deinstitutionalization: the present and future of mental health long-term-care policy. Journal of Social Issues 45:1-15, 1989Google Scholar
4. Surles RC: Chartbook of Mental Health Information. Albany, New York State Office of Mental Health, 1990Google Scholar
5. Curtis JL, Millman EJ, Struening E, et al: Effect of case management on rehospitalization and utilization of ambulatory care services. Hospital and Community Psychiatry 43:895-899, 1992Abstract, Google Scholar
6. Curtis JL, Millman EJ, Struening E, et al: Deaths among former psychiatric inpatients in an outreach case management program. Psychiatric Services 47:398-402, 1996Link, Google Scholar
7. McCord C, Freeman HP: Excess mortality in Harlem. New England Journal of Medicine 322:173-177, 1990Crossref, Medline, Google Scholar
8. Vital Statistics by Health Areas and Health Center Districts, 1986. New York, Department of Health, Bureau of Health Statistics and Analysis, 1987Google Scholar
9. D'Ercole A, Struening EL, Curtis JL, et al: Effects of diagnosis, demographic characteristics, and case management on rehospitalization. Psychiatric Services 48:682-688, 1997Link, Google Scholar
10. De Cangas J: Case management: reasons for its effectiveness. International Journal of Psychiatric Nursing Research 2:225-240, 1996Google Scholar
11. Wolff N, Helminiak TW, Morse GA, et al: Cost-effectiveness evaluation of three approaches to case management for homeless mentally ill clients. American Journal of Psychiatry 154:341-348, 1997Link, Google Scholar
12. Burns BJ, Santos AB: Assertive community treatment: an update of randomized trials. Psychiatric Services 46:669-675, 1995Link, Google Scholar
13. D'Ercole A, Skodal AE, Struening E, et al: Diagnosis of physical illness in psychiatric patients using axis III and a standardized medical history. Hospital and Community Psychiatry 42:395-400, 1991Medline, Google Scholar
14. Radloff LS: The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1:385-401, 1977Crossref, Google Scholar
15. Spitzer RL, Williams JB, Gibbon M: Structured Clinical Interview for DSM-III. New York, New York State Psychiatric Institute, Biometrics Research Department, 1984Google Scholar
16. Spitzer RL, Williams JB, Gibbon M, et al: The Structured Clinical Interview for DSM-III-R (SCID): I. history, rationale, and description. Archives of General Psychiatry 49:624-629, 1992Crossref, Medline, Google Scholar
17. Selzer MD, Vinokur A, von Rooyen L: A self-administered Short Michigan Alcoholism Screening Test (SMAST). Journal of Studies on Alcohol 36:117-126, 1975Crossref, Medline, Google Scholar
18. Cohen J: Statistical Power Analysis for the Behavioral Sciences. New York, Academic Press, 1977Google Scholar
19. Winer BJ: Statistical Principles in Experimental Design. 2nd ed. New York, McGraw-Hill, 1971Google Scholar



