Treatment Intensity in Child and Adolescent Mental Health Services and Health Care Reform in Norway, 1998–2006
Outpatient services are the dominant modality of specialized psychiatric treatment provided to children and adolescents ( 1 , 2 ). Treatment intensity, measured as number of consultations the patient receives within a given period, is influenced by the patient's psychopathology and needs ( 3 ) and hence differs at the patient level. Differences in culture and structure in the organizational context make it likely that treatment intensity will differ at the outpatient clinic level, even after adjustment for case mix differences ( 4 ). Also, treatment intensity tends to change over time in response to several factors: in the United States, treatment intensity trends have been associated with changes in clinical preferences and with the introduction of capitated financing, managed care, and carve-out arrangements where, for example, cost-containment mechanisms may influence treatment intensity as well as service utilization in general ( 2 ). Hence, from a health policy point of view, descriptions of treatment intensity trends are of interest in periods of major policy change. The aim of this study was to assess trends in treatment intensity in outpatient child and adolescent mental health services (CAMHS) in Norway during a period of substantial growth in resource availability and a recentralization of hospital ownership.
This study covered the period 1998–2006. Although we found no studies describing treatment intensity trends in European countries, several analyses of U.S. trends were carried out in this period. In a nationwide U.S. study of privately insured children and adolescents covered by health plans, Martin and Leslie ( 2 ) reported a decrease in outpatient visits per patient from 1997 to 2000. These plans included various managed care mechanisms for controlling costs. The observed decline was especially prevalent among patients with depressive and hyperactivity disorders, and it coincided with a shift toward medication-based outpatient treatment. A similar decline in the average number of treatment days per child was reported in a study of behavioral health services in the Tennessee Medicaid managed care program in the period 1995–2000 ( 5 ). However, although individual therapy declined, there was an increase in family therapy. Although cost-containment mechanisms within managed care seem to be associated with a trend toward lessened intensity but increased access to treatment, a review of the literature presents a mixed picture ( 6 ). At the same time, there are substantial methodological challenges in linking organizational and financial factors to treatment intensity trends. Thus a descriptive statistical approach and a careful interpretation of observed changes in behavior are necessary.
In this study, we used a panel data set covering the period 1998–2006 and a nonexperimental interrupted time-series design to describe trends in treatment intensity in Norwegian outpatient CAMHS units. These units provide treatment to more than 95% of young patients receiving mental health services each year, and the inpatient treatment modality is restricted to a small number of patients with severe illness ( 7 ). In Norway, the CAMHS system consists of multidisciplinary treatment units that are part of the public, secondary specialized health care system. This system is funded mainly from capitation but supplemented somewhat with minor income from a public fee-for-service model based on consultations (no user charges). CAMHS units are responsible for service delivery to the total population within a specific geographical catchment area and cover all types of diagnostic categories.
Increased access in terms of the proportion of persons below 18 years of age receiving treatment each year has been a major health policy concern because of long waiting times and large unmet needs. In 1998 Norway set a national target of a 5% access rate by 2006, and the Norwegian government financed an increase in outpatient CAMHS treatment capacity by increasing the number of therapists by more than 50%. In addition, a target of a 50% increase in consultations per full-time-equivalent (FTE) therapist was introduced ( 8 ). A detailed performance measurement system was implemented describing access rate, productivity (consultations per FTE therapist), and treatment intensity ( 9 ). Productivity improved ( 10 ), and the national access rate increased from 2.0% in 1998 to 4.6% in 2006.
In 2002 hospital ownership was transferred from 19 counties to five regional health enterprises owned by the Norwegian Ministry of Health ( 11 , 12 ). As a result, CAMHS transitioned into organizational units owned by health enterprises. The reform implied a renewed focus on professional management and performance measurement. A new target of a 30% productivity increase in two years was introduced in 2002 ( 13 ). In 2005 the fee-for-service component was expanded to cover appointments with cooperating services (indirect consultations) in addition to the former patient-therapist session tariffs (direct consultations).
The aim of this study was to describe time trends in treatment intensity, with adjustments for patient case mix and factors associated with the size of CAMHSs. We were interested in the evolution of treatment intensity within a period of strong growth in resources, as well as potential shifts in treatment intensity concurrent with the ownership reform in 2002. Finally, we explored whether time trends differed across patient groups.
Methods
Data
The data set consisted of patient observations from a balanced panel of 37 CAMHS outpatient clinics. Depersonalized information was collected from the Norwegian Patient Register for patients aged 0–17 years who participated in at least one treatment session with a therapist during the year of observation. The data set was constructed to allow the number of consultations received by a patient in a specific year to be compared with CAMHS characteristics for the same year. Patient observations with a missing value for age (N=19) or year of referral (N=58) were excluded, leaving a sample of 127,422 observations. Because treatment duration may have been longer than one year, it was possible for the same patient to appear in multiple years as separate observations within the data set. To enable independent observations, two subsamples were extracted: patients referred in the same year as the year of observation, termed first-year observations (N=53,115), and patients referred in the year before the year of observation, termed second-year observations (N=41,058). CAMHS personnel data were collected from Statistics Norway.
Analyses
A three-level hierarchical structure was used for data analysis. Patient observations (level 1) were nested within a specific CAMHS year (level 2, N=333), which was nested within a specific CAMHS location (level 3, N=37). Level 3 captured time-invariant characteristics of CAMHS locations, whereas level 2 included time trend and shift variables. We used multilevel regression analyses to account for clustering effects ( 14 ).
For each subsample the numbers of direct and indirect consultations were analyzed separately. A random intercept model was specified to allow the residual from the predicted mean number of consultations to be split into three components: a residual specific to each CAMHS location (level 3), a residual specific to the year of treatment within a location (level 2), and a residual specific to the individual patient within the CAMHS location in a specific year (level 1). A set of patient characteristics was included to adjust for patient heterogeneity: age, gender, and dummy variables describing the main reasons for referral. The following nine referral categories were used: symptoms of autism, suicidal thoughts, sadness or depression, inhibited behavior, anxiety, behavioral problems, hyperactivity, eating disorders, and a residual category. Patients with an unknown value for main reason for referral (first year, N=6,947; second year, N=4,583) or missing values (first year, N=4,757; second year, N=2,798) were included in the residual category.
A trend variable with equal value across CAMHS (with 1998 coded 0, 1999 coded 1, and so on, ending with 2006 coded 8) captured time trend, and a specific shift dummy variable (1998–2001 coded 0, 2002–2006 coded 1) was included to assess a potential shift during the hospital reform period. Two additional time-dependent CAMHS variables were included to adjust for potential treatment intensity changes related to capacity growth: size (number of FTE therapists) and proportion of FTE psychiatrists and psychologists. Grand-mean centering of size and skill mix was applied. In addition, CAMHS locations (level 3) were split into two categories depending on mean CAMHS size during the nine-year period. CAMHS locations with a mean size of fewer than eight FTE therapists (N=13 locations) were categorized as small, and a dummy variable was included to adjust for time-invariant size.
A linear regression multilevel analysis was performed with Stata, version 10.0 ( 15 ). The maximum likelihood procedure was applied, and p values from z scores (defined as estimated coefficients divided by their standard errors) were used to test the significance of parameter estimates.
Results
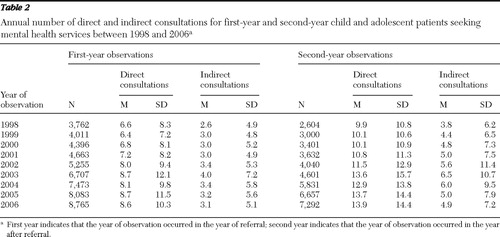
Table 1 and Table 2 present descriptive statistics for the patient observations in the two subsamples. Sadness or depression, behavioral problems, and hyperactivity were the most common reasons for referral ( Table 1 ). Table 2 shows annual mean number of direct consultations and indirect consultations per patient. In 2006 a first-year patient on average received two additional direct consultations and .5 additional indirect consultation compared with the number received in 1998. A second-year patient received on average four additional direct consultations and 1.1 additional indirect consultations in 2006 versus 1998. The observed differences served as background for the regression analysis taking patient characteristics and CAMHS factors into account.
 |
 |
The first step in the analysis was to estimate the amount of variance associated with the grouping structure from models with intercept and random terms only (empty models), which was measured by the intraclass correlation coefficient (ICC), defined as the proportion of variance at levels 2 and 3 of the total variance ( 14 ). The estimated ICC was significant but modest for CAMHS location (level 3) and CAMHS year (level 2) ( Table 3 ). CAMHS factors explained a larger proportion of indirect consultations compared with direct consultations. Patient-level factors were the main source of variation in the number of consultations.
 |
Table 4 presents results from entering explanatory variables into the random intercept models. The patient factor estimates show that the mean number of direct consultations for boys was lower than that for girls (no difference for indirect consultations), that first-year patients younger than 13 years of age received fewer direct and indirect consultations (with minor differences for second-year patients), and, likewise, that reason-for-referral estimates differed. These results illustrate the estimated influence of patient characteristics and symptomatology on treatment intensity, independent of CAMHS location and point in time.
 |
Significant trend, shift, and CAMHS size associations with treatment intensity were found ( Table 4 ). Size was positively associated with direct consultations in both subsamples and negatively associated with indirect consultations for second-year patients. Skill mix of therapists had no significant influence. A significant trend increase was found only for direct consultations for second-year patients. An estimated annual increase of .37 consultation implies 2.97 additional consultations over eight years, which is a 26% increase relative to the intercept. We compared the period 2002–2006 with the previous period. A significant positive shift was found for both consultation types and both subsamples. For example, from 2002 the mean number of direct consultations was 1.11 more than the previous period for first-year patients. The estimated shifts were of comparable size across consultation types and subsamples, but the relative increase was higher for indirect consultations.
To investigate whether the observed trend and shifts differed between patient groups, alternative models were estimated that included interaction effects from reasons for referral and gender. The trend estimate for direct consultations for second-year patients with inhibited behavior was lower than the sadness or depression reference estimate (reference=.47, p<.01; interaction effect=-.33, p<.05). Shift estimates for direct consultations for first-year patients with suicidal thoughts and eating disorders were higher than the reference estimate of 1.27 (p<.01). The interaction effects were 1.48 (p<.01) and 1.20 (p<.05), respectively. A lower estimate was found for hyperactivity (interaction effect=-.83, p<.05). For second-year patients with behavioral problems, the estimate was higher than the reference estimate of 1.46 (p<.05). The interaction effect was .78 (p<.10), whereas the anxiety estimate was lower (interaction effect=-1.43, p<.05). In addition, second-year boys received fewer direct consultations (interaction effect=-.52, p<.10). Interaction effects were mainly found for direct consultations.
Models with alternative specifications of the shift variable were estimated to assess the sensitivity of the results to choice of shift period. No significant shift was found by including years before 2002 in the shift period. Alternative models applying log-transformed dependent variables were also analyzed because of skewed data. Taking the alternative empirical specifications into account, the results presented appear to be robust.
Discussion
Norwegian outpatient mental health services for children and adolescents experienced a major increase in overall treatment capacity in the period 1998 to 2006. As a result, access to treatment improved, especially for patients given lower priority on the basis of the criteria of accepted waiting time for treatment. The proportion of patients with attention-deficit hyperactivity disorder (long waiting time accepted), for example, increased compared with, for another example, patients suffering from severe depression (short waiting time) ( 16 ). At the same time, mean treatment intensity increased. Adjusting for case mix and size of outpatient CAMHS unit, we found two main patterns: a trend increase throughout the period for direct consultations for patients in the second-year phase of treatment and a marked positive shift in number of consultations from 2002 regardless of type of consultation and time since referral. Trend and shifts differed partly between patient groups according to the main reason for referral and gender.
A lack of complete diagnostic information was a limitation of this study. Diagnosis would have given a more precise description of case mix changes because varied use of referral categories has been reported. This variance is partly associated with media attention to, for example, child and adolescent depression ( 17 ). In addition, data describing medication-based treatment were not available, and hence no comparison with treatment intensity could be performed.
Another limitation was that we were not able to identify individuals across years, which led us to analyze two subsamples. Because information about the exact dates of treatment commencement and completion was not available, we were not able to control for duration of treatment within the year of observation. Therefore, one implication is that increased treatment intensity might partly be the result of increased duration. A more in-depth assessment of treatment intensity for specific diagnostic groups would require more precise information, but in this case, the available information was considered sufficient to describe a broad picture of treatment intensity developments.
In Norway, cost containment received minor attention within CAMHS in the study period. A national mental health policy plan was implemented that involved a substantial increase in financial resources and number of therapists. The results show that increased CAMHS size was associated with increased treatment intensity, and this finding might be explained by a higher degree of specialization within the outpatient CAMHS system. In addition, we observed a trend increase throughout the period for direct consultations for second-year patients. This trend might partly reflect increased treatment duration, and some critics have claimed that CAMHS might strategically have extended treatment duration in order to cope with performance targets ( 18 ).
A shift in treatment intensity seems to have occurred in 2002, and one can speculate about whether the increase was associated with the implementation of hospital ownership reform. Professional hospital leadership inspired by experiences from sectors other than health care was introduced, and CAMHS incentives to expand the number of consultations increased because of new productivity targets and a renewed focus on fee-for-service income. CAMHS changes in record-keeping practices should be taken into account. In general, changes in the way data are registered in local information systems might produce more thorough and accurate, and thus legitimate, documentation but render data less comparable over time. The problem of upcoding services in response to financial incentives is well known in the hospital sector ( 19 ). In this study financial incentives seem to have been of minor importance, but health enterprises extensively utilized performance measurement.
One can also speculate about whether outpatient CAMHS to some extent responded to the reform by trading wider accessibility for increased intensity, in contrast to the main national objective of the policy. Although a substantial increase in access rate was observed during the nine-year period, the rate remained below the national target. Efficient allocation of treatment resources between patients is an important health policy concern, and in principle the patient outcome of increased service intensity should be considered in the context of admissions of new patients to treatment. For children and adolescents, a positive relationship between dose and effect has been questioned ( 20 , 21 ). Unfortunately, no outcome measures were available for this study, but outcome measurement has received increased attention ( 22 ).
Not surprisingly, we found that patient-related factors were the main source of variation in treatment intensity, and the observed differences between patient groups seem to be in accordance with findings from U.S. studies ( 3 ). A previous Norwegian study of specific diagnostic groups, such as depression and attention-deficit hyperactivity disorder, demonstrated huge variations in treatment intensity within CAMHS units ( 23 ), and national treatment guidelines have recently been published ( 24 ). Variation in treatment intensity can be related to the complex nature of outpatient service provision to children and adolescents. CAMHS provides diagnostic assessment and treatment within the context of patients' overall environments (relatives, schools, primary care, social services, and so on), and patient heterogeneity necessitates taking this broad set of factors into account when assessing the individual.
In Norway, municipalities have received increased financial support to improve preventive mental health services. Unfortunately, no data were available to assess the association between local service provision and treatment intensity in CAMHS units. Our results show that compared with the number of direct consultations, the number of indirect consultations was more sensitive to CAMHS differences. CAMHS discretion concerning indirect consultations might partly be influenced by level of resources and competence in local service provision, in addition to geographical constraints such as travel distances to service points. The link between local service provision and treatment intensity in specialized services seems to be an important area for future research.
Conclusions
In Norway, treatment intensity in outpatient mental health services for children and adolescents increased from 1998 to 2006. A marked increase in intensity was observed from 2002, after adjustment for patient-level factors, increased therapist capacity within outpatient units, and a general trend increase throughout the period. One can speculate about whether inherent organizational incentives in the 2002 hospital ownership reform have stimulated increased CAMHS treatment intensity in contrast to the main health policy objective of improved access.
Acknowledgments and disclosures
This work was supported by grants from the Norwegian Research Council and from the Norwegian Ministry of Health and Social Affairs, sponsored through SINTEF Health Services Research.
The author reports no competing interests.
1. Ringel JS, Sturm R: National estimates of mental health utilization and expenditures for children in 1998. Journal of Behavioral Health Services and Research 28:319–333, 2001Google Scholar
2. Martin A, Leslie D: Psychiatric inpatient, outpatient, and medication utilization and costs among privately insured youths, 1997–2000. American Journal of Psychiatry 160:757–764, 2003Google Scholar
3. Harpaz-Rotem I, Leslie D, Rosenheck RA: Treatment retention among children entering a new episode of mental health care. Psychiatric Services 55:1022–1028, 2004Google Scholar
4. Glisson C: The organizational context of children's mental health services. Clinical Child and Family Psychology Review 5:233–253, 2002Google Scholar
5. Saunders RC, Heflinger CA: Access to and patterns of use of behavioral health services among children and adolescents in TennCare. Psychiatric Services 54:1364–1371, 2003Google Scholar
6. Frank RG, Garfield RL: Managed behavioral health care carve-outs: past performance and future prospects. Annual Review of Public Health 28:303–320, 2007Google Scholar
7. Bjørngård J, Pedersen P, Kaspersen S, et al: SAMDATA Sector Report Specialized Mental Health Services 2006 [in Norwegian]. Report no 2/07. Trondheim, Norway, SINTEF Health Research, 2007Google Scholar
8. National Mental Health Plan 1999–2006 [in Norwegian]. No 63 (1997–98). Oslo, Ministry of Health and Care Services, 1998Google Scholar
9. Antun KS, Bjerkan AM, Bjørngård JH, et al: SAMDATA Key Indicators for Specialized Health Care Services 2006 [in Norwegian]. Report no 1/07. Trondheim, Norway, SINTEF Health Research, 2007Google Scholar
10. Halsteinli V, Kittelsen S, Magnussen J: Productivity growth in Norwegian psychiatric outpatient clinics for children and youths. Journal of Mental Health Policy and Economics 8:183–191, 2005Google Scholar
11. Hagen TP, Kaarbøe OM: The Norwegian hospital reform of 2002: central government takes over ownership of public hospitals. Health Policy 76:320–333, 2005Google Scholar
12. Magnussen J, Hagen TP, Kaarboe OM: Centralized or decentralized? A case study of Norwegian hospital reform. Social Science and Medicine 64:2129–2137, 2007Google Scholar
13. Steering Document for Helse Midt-Norge RHF [in Norwegian]. Oslo, Ministry of Health and Care Services, 2003Google Scholar
14. Hox J: Multilevel Analysis: Techniques and Applications. Hillsdale, NJ, Erlbaum, 2002Google Scholar
15. Rabe-Hesketh S, Skrondal A: Multilevel and Longitudinal Modeling Using Stata. College Station, Tex, Stata Corp, 2008Google Scholar
16. Pedersen PB, Lilleeng SE, Sitter M: Evaluation of the National Mental Health Plan in Norway: Supplementary Analyses of Specialized Services [in Norwegian]. Report A6400. Trondheim, Norway, SINTEF Health Research, 2008Google Scholar
17. Reigstad B, Jorgensen K, Wichstrom L: Changes in referrals to child and adolescent psychiatric services in Norway 1992–2001. Social Psychiatry and Psychiatric Epidemiology 39:818–827, 2004Google Scholar
18. Examining Services to Children and Adolescents With Mental Health Problems [in Norwegian]. Document no 3:7. Oslo, Office of the Auditor General in Norway, 2007Google Scholar
19. Steinbusch PJM, Oostenbrink JB, Zuurbier JJ, et al: The risk of upcoding in casemix systems: a comparative study. Health Policy 81:289–299, 2007Google Scholar
20. Salzer MS, Bickman L, Lambart EW: Dose-effect relationship in children's psychotherapy services. Journal of Consulting and Clinical Psychology 67:228–238, 1999Google Scholar
21. Foster EM: Is more better than less? An analysis of children's mental health services. Health Services Research 35:1135–1158, 2000Google Scholar
22. Hanssen-Bauer K, Gowers S, Aalen OO, et al: Cross-national reliability of clinician-rated outcome measures in child and adolescent mental health services. Administration and Policy in Mental Health and Mental Health Services Research 34:513–518, 2007Google Scholar
23. Bremnes R, Bjerkan AM, Halsteinli V: From Referral to Closure: An Analysis of Differences in Outpatient Practice in Mental Health Services for Children and Adolescents: A National Register Study 2006 [in Norwegian]. Report no A6800. Trondheim, Norway, SINTEF Health Research, 2008Google Scholar
24. Treatment Guidelines for Attention Deficit Hyperactivity Disorder Among Children, Adolescents and Adults [in Norwegian]. Oslo, Norwegian Directorate of Health, 2005Google Scholar



