Mental Disorders Among Homeless People Admitted to a French Psychiatric Emergency Service
Homelessness, defined as the absence of customary and regular access to a conventional dwelling or residence ( 1 ), is a growing social and public health problem in developed countries. The number of homeless people living in the United States, the United Kingdom, and France has been estimated to be at least 740,000, 120,000, and 100,000, respectively ( 1 , 2 , 3 ), and these numbers are expected to rise in the current economic context. Between one-fourth and one-third of homeless people have a serious mental illness such as schizophrenia, bipolar disorder, or major depression ( 4 , 5 , 6 , 7 ). Management of these conditions remains challenging. Homeless people are often unable to pay for their treatment; their adherence to treatment and the continuity of the care they receive are often poor, and their already limited access to care is exacerbated by transport problems, self-neglect, and fear of being institutionalized ( 8 , 9 , 10 , 11 ). Homeless people with mental illness primarily use the emergency departments of general or psychiatric hospitals ( 12 ). A recent study found that 30% of the care episodes in psychiatric emergency wards in the United States are provided to homeless patients and that homeless patients use psychiatric emergency services repeatedly ( 13 ). Homeless people also have lower hospital admission rates than nonhomeless people ( 14 ). These factors contribute to the severity of their diseases and thus to their high management costs ( 15 ). This information should be used to plan appropriate intervention measures for identifying and managing various mental disorders among homeless people. Addressing the problem of homelessness requires a proper understanding of its size and association with psychiatric disorders, as well as factors such as homeless people's access to care, adherence to treatment, and follow-up.
Homelessness among people with a serious mental illness has received significant attention. However, because most studies have been conducted in countries where homeless people do not have universal health coverage, results may be subject to selection bias. The evaluation and management of homeless people in the French health care system, especially psychiatric emergency services, may contribute to a better analysis of their needs. The French health care system combines near-universal coverage with a public-private mix of hospital care and ambulatory care, as well as a higher volume of service provision than the American health care system ( 16 ). Patients are free to move between the different services. National Health Insurance (NHI) reimburses 70%–80% of medical care costs, and residents are able to purchase private complementary insurance, which can reimburse the remaining 20%–30% of costs. All residents are automatically enrolled within the NHI fund, and 90% of them subscribe to supplementary private health insurance. However, for socially disadvantaged persons who cannot subscribe to private insurance or for severely ill persons with high medical costs, the French health care system guarantees totally free health care and hence access to the most appropriate treatment, regardless of costs ( 17 , 18 , 19 ).
Few studies have examined the use of psychiatric emergency services by homeless people ( 13 , 20 , 21 ), although emergency services can be considered an interesting place of observation and intervention in studies of homeless persons.
Moreover, the majority of studies focused on a limited time period (cross-sectional studies ranging from a single day to several months). This may introduce bias to the representativeness of results, mainly because of the homeless population's heterogeneity ( 13 , 20 , 21 , 22 , 23 ). These studies also analyzed single episodes of care ( 21 , 23 , 24 ), rather than taking longitudinal approaches to homeless patients and their global management (including adherence to treatment and follow-up).
The aim of this work was to identify factors associated with homelessness status among patients admitted to the psychiatric emergency ward of a French public teaching hospital over a six-year study period (2001–2006).
Methods
Setting
Marseille, located in the southeastern part of France, is the second largest city in France, with a population of nearly one million inhabitants, of which an estimated 1,500 are homeless ( 25 ). Of these, about 800 sleep on the streets, 600 live in the two established shelters, and the remainder sleep in different hospitals in and around Marseille ( 25 ).
This study was conducted in the psychiatric emergency ward of a large French public teaching hospital in Marseille (Assistance Publique-Hôpitaux de Marseille), which is responsible for evaluating and treating persons with psychiatric disorders. Annual visits to this ward number approximately 3,500. It provides services to 95% of individuals living in Middletown Marseille who present with psychiatric emergencies or face involuntary admission. The ward also guarantees free medical service 24 hours a day, seven days a week to natives and immigrants, regardless of legal, social, or economic status.
Population
We retrospectively analyzed data for all episodes of care in the psychiatric emergency ward from January 1, 2001, to December 31, 2006, delivered to persons aged at least 15 years. Living situation and homelessness were assessed at each admission by a health care professional by using the French National Institute (Institut National de la Statistique et des Etudes Economiques) definition of homeless: "an individual who, the night preceding emergency admission: 1) Slept in a place not intended for housing, or 2) Used a hosting service" ( 26 ) (a hosting service is a service that provides individuals with meals and a place to sleep for one or several nights). On the basis of these criteria, homelessness status during our six-year study period was defined in two different ways: if the person received health care at least once while homeless ( 8 ) or if homelessness was the living situation most frequently reported during various contacts with the psychiatric emergency department.
Data collection
The study involved a retrospective review of administrative and medical databases from the psychiatric emergency ward. For each episode of care, data on the patient's demographic, financial, clinical, and therapeutic characteristics were available.
The French National Commission for Data Protection (CNIL) approved this study. Founded in 1978, the CNIL is an independent administrative authority protecting privacy and personal data ( 27 ). Because the project involved the retrospective analysis of anonymous administrative data sets—patient names were replaced by a unique identification number—informed consent was not necessary. Principles outlined in the Declaration of Helsinki were followed ( 28 ).
Units of analysis and definition of parameters
Because some individuals received multiple episodes of care during the study period, two analysis sets were used: episodes of emergency care and individual patients. If readmission rates varied significantly between patients, the exclusive use of episode data could bias the results.
The episode approach involved the comparison of care episodes for homeless and nonhomeless patients, and the individual approach involved the comparison of individual homeless and nonhomeless patients.
For emergency care episodes, the following data were examined: reasons for referral, referral source (self-referral, referred by a health care professional, or referred by a non-health care professional), nature of therapeutic crisis management, and whether the care episode was followed by psychiatric hospitalization.
For individual patients, the following data were examined: demographic and financial information and diagnosis. Demographic information consisted of age (defined as the mean age during the various contacts), gender, living situation, marital status (defined as the most frequently reported status), and dependent children (yes or no). Financial information included whether the patient received unemployment benefits or financial assistance payments of 600 to 900 Euros per month through government social programs. Clinical information included psychiatric diagnosis. Because patients may present with more than one psychiatric diagnosis in one or several care episodes, we described the diagnostic characteristics only for the individual patients. Diagnoses were based on the ICD-10 sections ( 29 ): mental and behavioral disorders resulting from psychoactive substance use (F1); schizophrenia and schizotypal and delusional disorders (F2); mood (affective) disorders (F3); neurotic, stress-related, and somatoform disorders (F4); and disorders of adult personality and behavior (F6). Personality disorders were also considered on the basis of the DSM-IV ( 30 ) concerning three clusters: A (odd or eccentric disorders), B (dramatic, emotional, or erratic disorders), and C (anxious or fearful disorders). Dual diagnosis was defined as the co-occurrence of a mental disorder and a substance-related disorder ( 31 , 32 ).
Other data regarding the emergency psychiatric ward analyzed during the study period included number of emergency care episodes, interval between discharge and readmission (days), and number of emergency care episodes followed by psychiatric hospitalization.
Statistical analysis
The demographic and clinical characteristics of homeless and nonhomeless patients were compared using Student's t test for continuous variables and chi square analysis for categorical variables. The comparisons were made first for care episodes and then for individual patients.
A logistic regression analysis was used to estimate odds ratios for the association of sociodemographic or diagnosis factors with homelessness, after adjustment for confounding factors. Models were developed with backward selection procedure. Variables relevant to the model were selected on the basis of their clinical interest or a threshold p value (≤.005) during univariate analysis. The following variables were included in the analysis, with the respective reference groups listed in parentheses: age, male (female), married (single), children (none), unemployment benefits (none), social financial assistance payments (none), psychiatric diagnosis with no dual diagnosis (none), and dual diagnosis (none). The final model included odds ratios and 95% confidence intervals.
All the tests were two-tailed, and the alpha value was set at <.005 to correct for multiple comparisons ( 8 , 24 , 33 ). Data were analyzed using the SPSS, version 15.0, software package.
Results
Only the results based on the first definition of (having received care in the psychiatric emergency ward at least once while homeless) are reported here. The analysis of the results using the second definition (homelessness was the living situation most frequently reported during various contacts) did not change our findings (data not shown).
During the six-year study period (2001–2006), 16,754 episodes of care in the psychiatric emergency ward were experienced by 8,860 different persons, including 591 homeless patients (6.7%) and 8,269 nonhomeless patients (93.3%). Homeless patients accounted for 2,886 of the 16,754 care episodes (17.2%).
Episode of emergency care
As shown in Table 1 , self-referral to the psychiatric emergency ward was more frequent in care episodes for homeless patients than in those for nonhomeless patients (68.3% versus 53.3%) (p<.001). Homeless patients were more likely than nonhomeless patients to have substance use disorders (12.4% versus 7.6%) and social problems (7.0% versus 2.4%). Agitation, anxiety, disruptive behavior, depressive symptoms, and suicide attempts were less frequent in care episodes for homeless patients than in those for nonhomeless patients. Also, aggressive behavior, mental confusion, psychotic symptoms, manic symptoms, cognitive disorders, and somatic and relational problems did not differ statistically between the two groups. Homeless patients were less likely than nonhomeless patients to have a psychiatric hospitalization after an emergency care episode (47.8% versus 51.1%; p=.002).
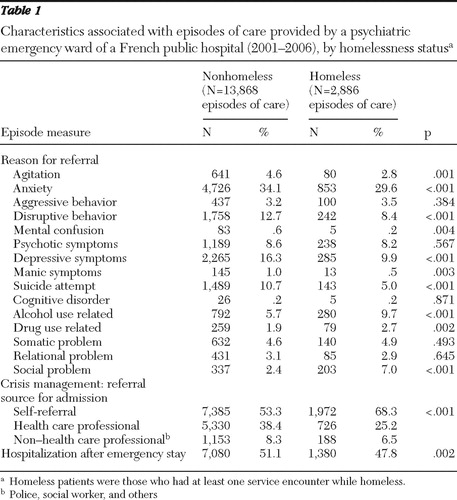 |
Individual patients
As shown in Table 2 , univariate analysis showed that age was not associated with homelessness. Compared with nonhomeless patients, homeless patients were significantly more likely to be male and single and less likely to have dependent children. Homeless patients were more likely than nonhomeless patients to be beneficiaries of financial assistance from government social programs, but no statistical difference was found between the groups for unemployment benefits. Mental and behavioral disorders due to psychoactive substance use ( ICD-10 section F1), schizophrenia and schizotypal and delusional disorders ( ICD-10 section F2), disorders of adult personality and behavior ( ICD-10 section F6), and dual diagnosis were more frequent in the homeless group than in the nonhomeless group. In the personality and behavior disorder category ( ICD-10 section F6), only cluster B—dramatic, emotional, or erratic disorders—was associated with homeless patients.
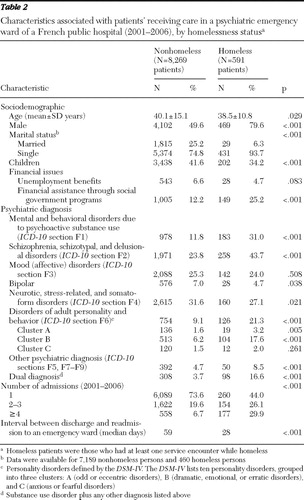 |
The mean±SD number of visits to the psychiatric emergency ward was higher for homeless patients (4.9± 12.3) than for nonhomeless patients (1.7±2.4) (p<.001). Readmission to the emergency psychiatric ward was higher for homeless patients than for nonhomeless patients. A total of 331 homeless patients (56.0%) compared with 2,180 (26.3%) nonhomeless patients benefited from more than one episode of care (p<.001); 29.9% of homeless patients versus 6.7% of nonhomeless patients had four or more visits during the study period (p<.001). Readmission also occurred earlier for homeless patients (28 versus 59 days) (p<.001).
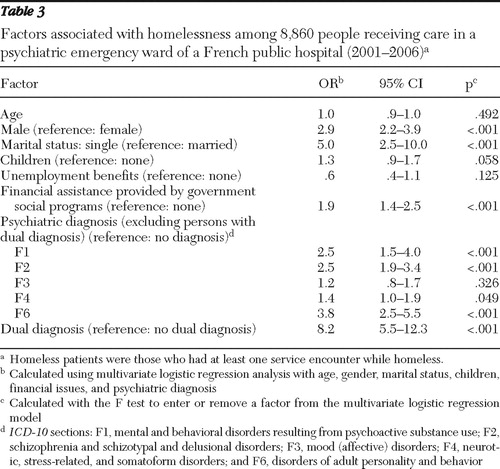
As shown in Table 3 , in multivariable analyses, being male, being single, and having financial assistance provided by government social programs were associated with homelessness. Substance use, schizophrenia and related disorders, personality and behavioral disorders, and dual diagnosis were also associated with homelessness.
 |
Discussion
Homeless people represented 6.7% of patients who visited the psychiatric emergency ward during the six-year study period, and they accounted for 17.2% of the care episodes. They were less likely than nonhomeless people to be hospitalized after receiving care. Schizophrenia (43.7%) and substance use disorders (31.0%), were the most common psychiatric disorders among homeless patients, and 16.6% had a dual diagnosis.
Several crucial points related to the management of health care for homeless people with mental disorders must be discussed and clarified. Can we affirm that better health insurance coverage improves access to care for homeless people, leading to better mental health care management? Does a health care policy of universal coverage, as opposed to nonuniversal coverage, have a significant impact on the management of care for homeless people with mental disorders?
Access to mental health care for homeless people in France
One of our study's strengths was the psychiatric emergency ward's inclusion in a health care system characterized by near-universal access. This is one of the first studies conducted in this type of health care system, following a recent Spanish study ( 24 ). Our study can be considered as representative of a population with mental disorders admitted to a psychiatric emergency ward, which limited selection bias and enabled us to simultaneously accomplish two analyses often separated in previous studies ( 2 , 13 , 24 ): first, almost all persons in the center of Marseille who were homeless with mental disorders and who visited our emergency service, and second, assessments of their care management in a psychiatric emergency ward. A total of 2,886 care episodes were provided for 591 of the estimated 1,500 homeless persons in Marseille. More than one-third (39%) of homeless people visited the emergency ward, which approximately corresponds to the prevalence of serious mental illness among homeless people (between one-fourth and one-third) ( 4 , 5 , 6 , 7 ). Previous studieshave reported lower rates of access to care. Differences in the definition of homelessness and sample selection may account for lower rates. Folsom and colleagues ( 8 ) examined the prevalence of homelessness among patients treated for serious mental illnesses in a public mental health system (San Diego) over a one-year period, but they did not take into account the use of the emergency psychiatric ward. Among 15,000 homeless persons in the study area, 1,569 were treated (10% of homeless patients). McNiel and Binder ( 13 ) examined the use of psychiatric emergency wards by homeless people in San Francisco: 829 episodes of care were provided to a homeless population of 15,000 (6%).
In view of our findings, we could hypothesize that access to care for homeless people seems to be higher in France, with its near-universal coverage and free mental health system. This hypothesis still needs to be explored and confirmed. Only the study of Pascual and colleagues ( 24 ), conducted in Spain on the use of psychiatric emergency wards, presented a similarly high rate of visits for homeless patients: 560 care episodes were provided to homeless patients in an area with a homeless population of 2,428 (23%). In our study, the fact that 68% of homeless people receiving treatment visited the emergency ward on their own initiative could also reflect easy access to personalized care. The emergency service seems to be considered by homeless people as more able to take care of their health problems, compared with other ambulatory or hospital services. An in-depth analysis of this finding is needed to better adapt the health care system organization to meet the expectations and needs of homeless patients, which are different from those of nonhomeless patients. However, although these results indicate that contact with psychiatric wards was easily made, they do not necessarily indicate that the homeless patients' mental health needs were being met ( 34 ).
Characteristics of homeless patients
There were several notable demographic factors associated with homelessness. As in previous studies, we found no association between age and homelessness ( 13 , 24 ); however, the sample of homeless patients in our study had a higher percentage of males than did other studies ( 8 , 24 ). This may be partly explained by the prevalence of social support structures for women and children at risk of homelessness. Recent studies in France showed that access to social care and informal support is particularly developed in France and that women were more likely than men to ask for and access specific psychological care, especially if they were experiencing social deprivation and poverty ( 35 , 36 ). Homeless patients in our sample also tended to be single and were less likely to have dependent children. Predictably, homeless psychiatric patients were less satisfied with their social support networks than domiciled patients, and they appraised them as being less supportive, reliable, and available. Previous reports have found that homelessness predisposes individuals toward poor social relations ( 37 ). In our study, only one-fourth of homeless patients received financial support provided by social agencies, which is an indirect indication of social precariousness. This observation suggests that noneconomic barriers may prevent people who are homeless or impoverished from receiving financial help that they may legitimately ask for and obtain.
With respect to clinical factors, the most frequent mental disorders were schizophrenia and substance use disorders, and many had a dual diagnosis, in line with previous investigations ( 13 , 24 ). Other studies have shown that alcohol abuse, intravenous drug use, and heavy tobacco use were significantly higher among homeless persons than in the general population ( 10 ). If serious mental illness is more prevalent among homeless people, it represents just one of many important vulnerability factors for homelessness ( 38 ). For example, substance abuse is associated with weakened immunity, and it predisposes users to specific infections. This should be considered when treating mental disorders among homeless patients. The absence of any difference between homeless and nonhomeless patients regarding somatic problems indicates the lack of interest that psychiatric services take in these problems. It reflects fragmented care and a lack of coordination between general and mental health care professionals in the treatment of these patients. Homeless individuals have substantial and complex needs, requiring care management programs to improve communication, cooperation, and understanding among health care professionals to enhanced continuity and coordination of care ( 39 ). It is also important to develop and employ specific measurements, such as quality of life or satisfaction instruments, to assess the needs of homeless people and improve their adherence to treatment ( 40 , 41 ).
Unlike previous investigations ( 13 , 24 , 42 ), our study did not find any difference between homeless and nonhomeless patients in aggressive behavior and violence. This may be due to the representativeness of our sample, which is higher than in other studies. Because of better care access, our study population included homeless people with only slight mental disorders, who were not involved in the criminal justice system, and who had "a more tolerable level of social disturbance." For the same reason, we recorded fewer visits for agitated and disruptive behavior among homeless patients.
Homeless patients also presented with less anxiety and fewer depressive symptoms, compared with nonhomeless patients. Although these results are concordant with literature ( 24 ), they should be considered with caution, because these symptoms are often less expressed among homeless patients and thus underdiagnosed by professionals ( 2 , 43 ). In the emergency context, it is difficult for health care professionals to correctly diagnose patients, notably homeless patients, who often fail to communicate emotional problems and therefore are not treated. The diagnostic validity of depression, as defined by the ICD-10 ( 29 ) and the DSM-IV ( 30 ) and by means of psychometric evaluations such as the Hamilton Rating Scale for Depression ( 44 ), should be explored in these populations. Homeless patients also presented with fewer suicide attempts than nonhomeless patients, although their social situation and precariousness can be considered a risk factor for suicide, and other studies have reported higher suicide attempt rates for homeless patients than for nonhomeless patients ( 43 , 45 ). In a study conducted with a large homeless sample in 2003, the prevalence of suicidal ideation was high (66.2% lifetime prevalence) ( 46 ). One explanation for the discrepancy between our study and others could be that a significant portion of suicide attempts by homeless people are more violent than those of domiciled patients and result in nonpsychiatric emergencies ( 46 ).
Use of the psychiatric emergency ward and care management
During the six-year study period, 17.2% of the care episodes in the psychiatric emergency ward were provided to homeless patients. This result is in line with previous studies. Rosenheck and Seibyl ( 20 ) reported that 20% of veterans were homeless at the time of admission to a psychiatric ward, and McNiel and Binder ( 13 ) reported that homeless individuals accounted for approximately 30% of the care episodes in a psychiatric emergency service. In a study by Folsom and colleagues ( 8 ), homeless patients received 15% of the care episodes. Culhane and colleagues ( 47 ) reported that 10% of patients treated for schizophrenia and 7% of those treated for affective disorders used a public shelter during a three-year study period. Heterogeneity in the findings of homelessness studies is well known. It has been argued that sample selection, definition of homeless, and diagnostic criteria contribute to this heterogeneity ( 2 ).
In our study, homeless patients were less likely than nonhomeless patients to be hospitalized after receiving care in the emergency ward, even though their disorders tended to be more severe. The readmission rate to the emergency ward was higher, and readmission occurred earlier. Factors associated with early and repeated admission are now well known: living alone, poor treatment adherence, inadequate medical management, premature discharge, and poor discharge planning ( 48 ). Lauber and colleagues ( 22 ) showed that homeless people received psychotropic medication and adequate treatment less often than nonhomeless patients, although they had more severe disorders. Previous research has also reported that substance abuse predicted decreased adherence to community treatment among individuals with mental disorders ( 49 ). Although these different factors are well known, health systems have difficulty taking them into account. The French health care system has three main problems. First, the principle stating that all psychiatric teams should have a similar and general competence in mental health care has limited the development of tertiary structures that are specialized in the assessment and treatment of specific mental disorders. Second, despite massive hospital bed closures over the past 15 years, hospital care is still predominant, while community treatment and sheltered housing for persons with the highest levels of disability are markedly underdeveloped. Hence, most French psychiatric hospitals have major difficulties finding beds for acutely ill patients ( 18 ). Finally, the French health care system tends to focus on either mental health or substance abuse treatment services. The elevated rates of co-occurring substance abuse and severe mental disorders among homeless patients in the psychiatric emergency ward may be an indication of insufficient and fragmented dual diagnosis services.
Limitations
This study has several limitations. First, the data source was an administrative database. Diagnoses made in an emergency context by a large panel of psychiatrists may not be as accurate as those made with diagnostic research instruments and structured interviews. Also, information regarding illness severity was not available.
Second, because our study was conducted in a large French teaching hospital, our findings may not be extrapolated to all of the other hospitals in France and to health care systems without universal coverage. The fact that our population included only individuals older than 15 years may also limit the scope of our results. However, these results are useful for monitoring policy and practice change in a community, because our study was conducted in a system with universal coverage, a domain that is poorly understood.
Finally, an important methodological aspect of our investigation was the definition of homelessness. Published definitions of homelessness have ranged from living on the street or in a homeless shelter ( 4 ) to using a public homeless shelter at least once over the course of several years ( 47 ) to being homeless at the time of admission to a psychiatric unit ( 20 ). One of our definitions of homelessness—that is, at least one service encounter while homeless over a six-year period—is not within this range of definitions. We chose a definition associating homelessness and an impoverished status (precariousness) that was less restrictive than, for example, being homeless at the time of admission. However, repeating our analyses with a more restrictive definition of homelessness—as the living situation most frequently reported during various contacts—did not change our findings (data not shown).
Conclusions
Homelessness is a serious problem among people with mental illness, and it is associated with several potentially modifiable factors. The French health care system seems to provide better access to care than health care systems without universal coverage. However, its management still needs to be improved for homeless patients, as suggested by the high rate of emergency service readmissions and the low hospitalization rate following the emergency visit. Universal coverage is only one dimension; being able to provide sufficient services must also be considered.
Homeless people require careful clinical evaluation. Suicide risk and major depression are clearly underestimated. Multidisciplinary and collaborative solutions are needed between social workers, emergency physicians, psychiatrists, substance abuse health services, and other specialized professionals, such as infectiologists, to improve the management of health care for homeless patients. Our study found that homeless patients were less likely than nonhomeless patients to be hospitalized. However, hospitalization of homeless patients should be encouraged, when appropriate. Health services currently do not take into account social welfare problems of homeless persons, and they should be encouraged to work with social services on the behalf of clients. Homeless people are best treated as inpatients because of the lack of treatment adherence associated with outpatient treatment. Adherence to therapy may be achieved through directly observed therapy in a monitored setting. We believe that specific and multidisciplinary ambulatory systems for homeless persons, which have already been developed in some areas, should be employed in all large cities. Managed care programs associating all involved parties must be developed to optimize long-term follow-up and global management. Application of these measures would likely increase the health status of homeless people.
Acknowledgments and disclosures
The authors report no competing interests.
1. Rossi PH, Wright JD, Fisher GA, et al: The urban homeless: estimating composition and size. Science 235:1336–1341, 1987Google Scholar
2. Fazel S, Khosla V, Doll H, et al: The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Medicine 5:e225, 2008Google Scholar
3. Lowry F: Impact on health care adds to the social cost of homelessness. Canadian Medical Association Journal 155:1737–1739, 1996Google Scholar
4. Breakey WR, Fischer PJ, Kramer M, et al: Health and mental health problems of homeless men and women in Baltimore. JAMA 262:1352–1357, 1989Google Scholar
5. Folsom D, Jeste DV: Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatrica Scandinavica 105:404–413, 2002Google Scholar
6. Folsom DP, McCahill M, Bartels SJ, et al: Medical comorbidity and receipt of medical care by older homeless people with schizophrenia or depression. Psychiatric Services 53:1456–1460, 2002Google Scholar
7. Sullivan G, Burnam A, Koegel P, et al: Quality of life of homeless persons with mental illness: results from the course-of-homelessness study. Psychiatric Services 51:1135–1141, 2000Google Scholar
8. Folsom DP, Hawthorne W, Lindamer L, et al: Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. American Journal of Psychiatry 162:370–376, 2005Google Scholar
9. Foucault C, Barrau K, Brouqui P, et al: Bartonella quintana bacteremia among homeless people. Clinical Infectious Diseases 35:684–689, 2002Google Scholar
10. Raoult D, Foucault C, Brouqui P: Infections in the homeless. Lancet Infectious Diseases 1:77–84, 2001Google Scholar
11. Rosenheck RA, Dennis D: Time-limited assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry 58:1073–1080, 2001Google Scholar
12. Herrman H, McGorry P, Bennett P, et al: Prevalence of severe mental disorders in disaffiliated and homeless people in inner Melbourne. American Journal of Psychiatry 146:1179–1184, 1989Google Scholar
13. McNiel DE, Binder RL: Psychiatric emergency service use and homelessness, mental disorder, and violence. Psychiatric Services 56:699–704, 2005Google Scholar
14. Appleby L, Desai PN: Documenting the relationship between homelessness and psychiatric hospitalization. Hospital and Community Psychiatry 36:732–737, 1985Google Scholar
15. Salit SA, Kuhn EM, Hartz AJ, et al: Hospitalization costs associated with homelessness in New York City. New England Journal of Medicine 338:1734–1740, 1998Google Scholar
16. Rodwin VG: The health care system under French national health insurance: lessons for health reform in the United States. American Journal of Public Health 93:31–37, 2003Google Scholar
17. Verdoux H: Psychiatry in France. International Journal of Social Psychiatry 49:83–86, 2003Google Scholar
18. Verdoux H: The current state of adult mental health care in France. European Archives of Psychiatry and Clinical Neuroscience 257:64–70, 2007Google Scholar
19. Verdoux H, Tignol J: Focus on psychiatry in France. British Journal of Psychiatry 183:466–471, 2003Google Scholar
20. Rosenheck R, Seibyl CL: Homelessness: health service use and related costs. Medical Care 36:1256–1264, 1998Google Scholar
21. Saliou V, Fichelle A, McLoughlin M, et al: Psychiatric disorders among patients admitted to a French medical emergency service. General Hospital Psychiatry 27:263–268, 2005Google Scholar
22. Lauber C, Lay B, Rossler W: Homeless people at disadvantage in mental health services. European Archives of Psychiatry and Clinical Neuroscience 256:138–145, 2006Google Scholar
23. Cougnard A, Grolleau S, Lamarque F, et al: Psychotic disorders among homeless subjects attending a psychiatric emergency service. Social Psychiatry and Psychiatric Epidemiology 41:904–910, 2006Google Scholar
24. Pascual JC, Malagon A, Arcega JM, et al: Utilization of psychiatric emergency services by homeless persons in Spain. General Hospital Psychiatry 30:14–19, 2008Google Scholar
25. Badiaga S, Menard A, Tissot Dupont H, et al: Prevalence of skin infections in sheltered homeless. European Journal of Dermatology 15:382–386, 2005Google Scholar
26. Brousse C, De la Rochère B: Hosting and Distribution Casting of Warm Meals: The Case of Homeless Subjects [in French]. Paris, France, Institut National de la Statistique et des Etudes Economiques, 2002. Available at www.insee.fr Google Scholar
27. Act n o 78-17 of 6 January 1978 on Data Processing, Data Files and Individual Liberties (amended by the Act of 6 August 2004 relating to the protection of individuals with regard to the processing of personal data). Journal officiel de la République Française. Assemblée Nationale et Sénat, France, 1978 Google Scholar
28. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Seoul, World Medical Association, General Assembly, Oct 2008Google Scholar
29. International Classification of Diseases, 10th ed. Geneva, World Health Organization, 2007Google Scholar
30. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington DC, American Psychiatric Association, 1994Google Scholar
31. Drake RE, Osher FC, Wallach MA: Homelessness and dual diagnosis. American Psychologist 46:1149–1158, 1991Google Scholar
32. Gonzalez G, Rosenheck RA: Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services 53:437–446, 2002Google Scholar
33. Bland JM, Altman DG: Multiple significance tests: the Bonferroni method. British Medical Journal 310:170, 1995Google Scholar
34. Bonin JP, Fournier L, Blais R: Predictors of mental health service utilization by people using resources for homeless people in Canada. Psychiatric Services 58:936–941, 2007Google Scholar
35. Firdion JM, Marpsat M: An advantage under stress: the lower risk of women to living in the street [in French]. Population 54:885–932, 1999Google Scholar
36. Saias T, Greacen T, Brengard D, et al: Mental health disorders, medical care and social support in a vulnerable population: the example of the maternal centres in Paris. Encephale 34:584–588, 2008Google Scholar
37. Caton CL, Shrout PE, Eagle PF, et al: Risk factors for homelessness among schizophrenic men: a case-control study. American Journal of Public Health 84:265–270, 1994Google Scholar
38. North CS, Smith EM, Pollio DE, et al: Are the mentally ill homeless a distinct homeless subgroup? Annals of Clinical Psychiatry 8:117–128, 1996Google Scholar
39. Boyer L, Francois P, Fourny M, et al: Managed care's clinical and economic impact on patients with type II diabetes in France: a controlled population-based study. International Journal of Health Care Quality Assurance 21:297–307, 2008Google Scholar
40. Barlesi F, Boyer L, Doddoli C, et al: The place of patient satisfaction in quality assessment of lung cancer thoracic surgery. Chest 128:3475–3481, 2005Google Scholar
41. Boyer L, Francois P, Doutre E, et al: Perception and use of the results of patient satisfaction surveys by care providers in a French teaching hospital. International Journal for Quality in Health Care 18:359–364, 2006Google Scholar
42. Martell DA, Rosner R, Harmon RB: Base-rate estimates of criminal behavior by homeless mentally ill persons in New York City. Psychiatric Services 46:596–601, 1995Google Scholar
43. Prigerson HG, Desai RA, Liu-Mares W, et al: Suicidal ideation and suicide attempts in homeless mentally ill persons: age-specific risks of substance abuse. Social Psychiatry and Psychiatric Epidemiology 38:213–219, 2003Google Scholar
44. Hamilton M: Rating depressive patients. Journal of Clinical Psychiatry 41:21–24, 1980Google Scholar
45. Babidge NC, Buhrich N, Butler T: Mortality among homeless people with schizophrenia in Sydney, Australia: a 10-year follow-up. Acta Psychiatrica Scandinavica 103:105–110, 2001Google Scholar
46. Desai RA, Liu-Mares W, Dausey DJ, et al: Suicidal ideation and suicide attempts in a sample of homeless people with mental illness. Journal of Nervous and Mental Disease 191:365–371, 2003Google Scholar
47. Culhane DP, Averyt JM, Hadley TR: The rate of public shelter admission among Medicaid-reimbursed users of behavioral health services. Psychiatric Services 48:390–392, 1997Google Scholar
48. Williams EI, Fitton F: Factors affecting early unplanned readmission of elderly patients to hospital. British Medical Journal 297:784–787, 1988Google Scholar
49. Binder RL, McNiel DE, Sandberg DA: A naturalistic study of clinical use of risperidone. Psychiatric Services 49:524–526, 1998Google Scholar



