Availability of Mental Health Service Providers and Suicide Rates in Austria: A Nationwide Study
Access to mental health care is expected to have an impact on the health outcomes of local residents. Among persons who complete suicide, from 70% to 90% have mental disorders, mostly affective disorders ( 1 , 2 ). Therefore, access to services, which increases the possibility of diagnosis and treatment of mental disorders, should have an impact on regional suicide rates. On average, 55% of persons who complete suicide have no contact with mental health or primary care providers in the month before suicide ( 3 ). Thus the availability of services may be relevant in explaining geographical variations in suicide incidence.
It was recently proposed that the density of mental health professionals and the availability of primary health care providers can be used as core indicators of mental health service quality and that the distribution of such providers between urban and rural areas and the suicide rate qualify as indicators of service quality ( 4 ). Indeed, the availability and utilization of mental health services may vary substantially between and within countries ( 5 ); typically, psychiatrists ( 6 , 7 , 8 ) and other physicians are less available in rural areas than in urban areas ( 9 , 10 , 11 ). Suicide rates are generally higher in rural areas ( 12 , 13 ).
Studies of the relation between suicide rates and availability of mental health services are rare. The seminal Gotland study in Sweden showed that educating general practitioners to recognize and treat depression was effective in reducing suicides ( 14 ). In a later study in Hungary, the density of physicians was shown to correlate with the rate of diagnosed depression and suicide rates ( 15 ). In the United States the unbalanced relationship between demand and availability of access to mental health services was shown to be associated with suicide rates ( 16 ), and a proposed proxy of the quality of local mental health care—county-level prescriptions for selective serotonin reuptake inhibitors—was inversely associated with suicide rates ( 17 ). A separate U.S. cross-state analysis showed an inverse relationship between state suicide rates and parameters of access to mental health care (such as the density of psychiatrists, number of uninsured persons, and federal aid for mental health care) ( 18 ). However, the most convincing evidence was recently found in a nationwide small-area study in Finland ( 19 ). The study showed that several mental health indicators, such as the availability of 24-hour emergency services and mobile outpatient services, number of hospitalized patients, and number of involuntary admissions, were associated with suicide rates. However, after adjustment for regional socioeconomic factors, only one indicator, a greater number of outpatient mental health services compared with inpatient services, remained weakly associated with suicide rates ( 19 ).
Differences in regional suicide rates may be explained by the influence of regional socioeconomic factors on mental disorders and by a selective migration mechanism of the population ( 20 , 21 , 22 , 23 , 24 , 25 ). Regional economic factors may also effect the migration and availability of mental health providers ( 6 , 7 , 26 ). Thus regional contextual factors may confound the association between access to health services and suicide rates. Researchers who examine such associations should be aware that the extent and magnitude of such regional effects may depend on the conceptualization of place effects ( 27 ).
The aim of this study was to examine in a small-area analysis whether the availability of professionals providing mental health treatment had an effect on regional suicide rates in Austria. The hypothesis was that districts in Austria in which mental health care providers were more available, as measured by the density of general practitioners, psychiatrists, and psychotherapists, would have lower suicide rates than districts with a low density of providers. The models accounted for socioeconomic covariates that have been shown to be associated with suicide rates, such as population density ( 12 , 13 ), average income and unemployment ( 28 ), and religion ( 29 ).
Methods
Data
Statistics Austria provided the official mortality database for suicides in nine age groups and for both genders in all 99 districts of Austria for each year from 1991 to 2005. Population density, proportion of Roman Catholics, and average income were obtained from the official Austrian population census of 2001. The 1991–2005 unemployment rates for each district were obtained from the Public Employment Service of Austria. Numbers of general practitioners and psychiatrists for each district were available for 1997 and 2002 and were obtained from the Austrian Medical Chamber. The Austrian Institute of Health provided figures on the official numbers of nonphysician psychotherapists registered for 1997 and 2002 by the Austrian Ministry of Health and Women. There were no human subjects concerns in this study. Given the aggregated nature of the data, no institutional review board approval was necessary. The study complied with guidelines for good scientific practice of the Medical University of Vienna and followed the Declaration of Helsinki.
Statistical analysis
The statistical analysis strategy has been described in previous reports ( 19 , 30 ). The suicide mortality rate of the Austrian districts was analyzed on the basis of standardized mortality ratios (SMRs). A SMR is the ratio between the observed and expected number of suicides. We calculated overall suicide rates for both sexes and the nine age groups. The expected suicide rates are obtained by multiplying the overall subgroup-specific suicide rates by the size of the subgroups in the district. To increase the number of events, for each district we pooled suicide data from 1991 to 2005. To adjust for random variation, the SMRs were estimated with a hierarchical Bayesian model that accounted for spatially correlated random effects by using an intrinsic conditional autoregressive prior that incorporated the neighborhood structure of districts and assumed a Poisson distribution for the observed number of suicides. All estimates were derived with R 2.9.2 ( 31 ) and OpenBUGS 3.0.3 ( 32 ) by using MCMC (Markov chain Monte Carlo) simulations with 10,000 iterations and two chains to validate the results.
To investigate confounding effects of socioeconomic covariables, we performed a principal components analysis for the following variables: logarithm of population density (2001), proportion of Roman Catholics (2001), local unemployment rate (averaged from 1991 to 2005), and average income (2001). From these variables we identified two principal components that accounted for 82% of the variance. The first component, accounting for 57% of the variance, was strongly associated with population density and average income and negatively associated with the proportion of Roman Catholics. It can be considered an indicator of districts that have a more urban population, a larger proportion of nondenominational residents (no religious affiliation) and non-Catholic immigrants, and a population density and income that are higher than average. The second component, accounting for 25% of the variance, corresponds essentially to the local unemployment rate.
To investigate the impact of the number of psychiatrists and psychotherapists on the SMR, we included the respective covariable in the Bayesian model and computed an estimate of the relative risk (RR) together with the Bayesian credible intervals (CIs). Absolute risk reduction (ARR) was computed for the Austrian annual suicide mortality rate of 18.5 per 100,000 population in 2001. The RR and the ARR are reported for the change of the covariable from the first to the third quartile. In the Bayesian model, we transformed the covariables by taking the square root followed by standardization (subtraction of the mean and division by the standard deviation) to account for the extremely skewed distribution.
We used an analogous model to estimate the impact of the number of general practitioners on the SMR. Because the distribution of this variable was less skewed, it was only standardized—that is, no square root was taken. To evaluate the impact of possible confounders, the analysis was repeated to include the two principal components. For all analyses, data for psychiatrists, psychotherapists, and general practitioners in 1997 were used. In addition, mean values from 1997 and 2002 were calculated and analyses were repeated to confirm stability of access to care over time ( 27 ). The Pearson correlation coefficients of the data sets between 1997 and 2002 for psychiatrists, general practitioners and psychotherapists were .89, .84, and .99, respectively, indicating no major shifts in their regional distribution during this time period.
Results
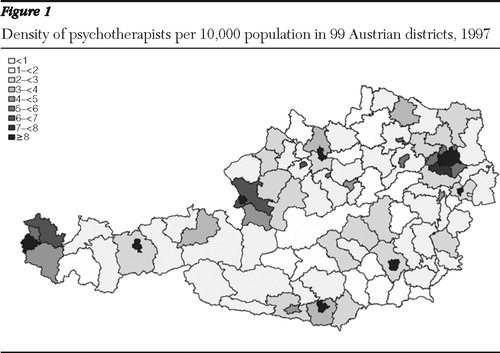
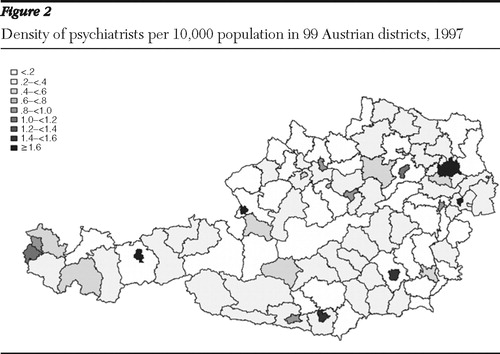
The Austrian suicide rate between 1991 and 2005 ranged between 22.3 and 17.3 per 100,000 inhabitants. Table 1 presents descriptive statistics of the variables studied. The spatial distribution of the density of psychotherapists and psychiatrists is shown in Figures 1 and 2 . Population density was found to be correlated with the density of psychiatrists (r=.42, p<.001) and psychotherapists (r=.6, p<.001) but not general practitioners.
 |
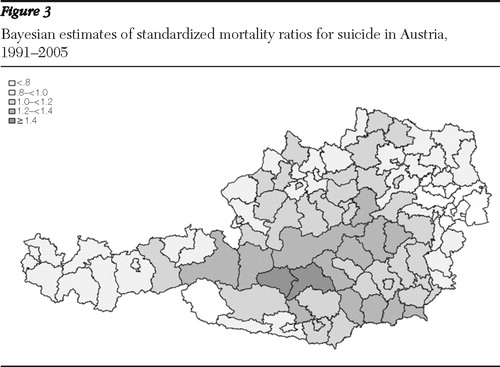
The mean±SD SMR according to the Bayesian estimates was 1.02±.17, with a range from .63 to 1.47, indicating a large heterogeneity across districts ( Figure 3 ). In the analysis in which socioeconomic factors were not included, the density of psychotherapists per 10,000 population showed a significant effect (RR=.97, CI=.94–.99; ARR=-.62, CI=-1.20 to -.11). However, no significant effects were found for the density of psychiatrists or of general practitioners per 10,000 population. [Figures showing scatter plots of the SMR and the density of psychotherapists and psychiatrists are available in an online supplement to this article at ps.psychiatryonline.org .]
The same results were found for psychotherapists and for psychiatrists when the mean density from 1997 to 2002 was used instead of the density in 1997: unadjusted analysis for psychotherapists, RR=.97, CI=.94–.997, and ARR=-.56, CI=-1.14 to -.06; unadjusted analysis for psychiatrists, RR= .99, CI=.97–1.02, and ARR= -.12, CI=-.65 to .38.
When the analysis adjusted for socioeconomic variables by including both principal components in the model, the association between density of psychotherapists and SMR was no longer significant. However, the first principal component showed a significant effect on the SMR in this model (RR=.94, CI=.88–.99, and ARR= -1.17, CI=-2.34 to -.05). The second component showed no significant effect. The density of psychotherapists and of psychiatrists were both positively correlated with the first principal component (Spearman r=.69 and r=.64, respectively).
Discussion
The hypothesis of this study was that regional access to mental health care providers has an impact on regional suicide rates. Neither the density of general practitioners nor the density of psychiatrists was associated with SMR. However, the density of psychotherapists had a weak association with SMR. A further finding of this study was that the first principal socioeconomic component was highly correlated with the density of psychiatrists and of psychotherapists. This component reflects an urban population with a higher proportion of nondenominational (no religious affiliation), non-Catholic inhabitants and higher-than-average income and population density.
General practitioners
In Austria 77%–79% of all psychopharmacological agents are prescribed by general practitioners ( 33 ). The density of general practitioners varied little across districts, which may explain the lack of association between access to general practitioners and suicide rates. The assumption of heterogeneity in exposure of a population is vital to determining relative risk ( 34 ). The relatively homogeneous distribution of general practitioners across districts may result from demand-oriented planning by the social insurance system of its contracts with general practitioners. In 1997 approximately 70% of general practitioner practices and 20% of psychiatric practices were contract based, according to the Austrian Medical Chamber; however, in 1997 and currently, no psychotherapist has a contract with the social insurance system ( 33 ).
We found no correlation between the first principal component and the population density of general practitioners. However, this component was correlated with the density of psychiatrists and of psychotherapists. As previous studies have shown, most mental health services in rural areas are provided by general practitioners ( 4 , 6 ).
Psychiatrists and psychotherapists
The density of psychotherapists was found to vary considerably between districts. The average density of psychotherapists was 1.73 per 10,000, which is about ninefold higher than the density of psychiatrists in Austria. The higher density could account for the finding of a weak crude effect of psychotherapist density on suicide rates but no effect of psychiatrist density. In the United States, where the density of psychiatrists is considerably higher (1.4 per 10,000) ( 8 ) than in Austria (.2 per 10,000), a crude effect of the density of psychiatrists on suicide rates has been described ( 18 ). After adjustment for the first principal component of covariates in our study, the weak effect of psychotherapist density on suicide rates was lost. In addition, the first principal component was a significant predictor of suicide rates.
Because psychotherapist density and the first principal component were correlated, the results should be considered with caution. Much evidence has been reported supporting the view that suicide rates are influenced by regional socioeconomic characteristics, such as per capita income, deprivation, unemployment rates, and population density ( 13 , 22 , 35 , 36 ). Our finding that the density of psychotherapists had a crude effect on suicide rates is new. However, it is likely that psychotherapist density is a function of the urban component. This multicollinearity makes it difficult to understand the separate effects of each factor on suicide rates, especially when the question of conceptualization of place effects is raised ( 27 ).
Studies examining the influence of access to mental health care on suicide rates are rare. Only one small-area study from Finland has been reported that used a similar statistical method ( 19 ). Although the Finnish study was based on more mental health care access variables than ours, it was not adjusted for spatial correlation of districts. Such spatial correlation takes into account the argument that local access to care can have an impact on local suicide rates ( 27 , 30 ). This argument supports the appropriateness of our analysis, even though it did not quantify the availability of psychiatric inpatient facilities: such facilities serve large catchment areas that typically cover more than one district. In the Finnish study, adjustment for socioeconomic variables similarly attenuated most of the significant associations between mental health access proxies and suicide rates, and only a higher ratio of outpatient services to inpatient services remained significant.
Urbanicity and mental health specialists
It has been shown that a region's economic situation determines physician supply and utilization ( 26 ). Our results show that access to psychiatrists and psychotherapists is better in urbanized and privileged districts than in deprived regions. On the other hand, the low availability of psychiatrists resulting from long waiting lists and the minimal reimbursement for psychotherapy from nonpsychiatrists increase barriers to the professional mental health care needed by suicidal patients. Poorer access to mental health professionals partly explains how socioeconomic conditions may influence suicide rates. A previous study noted an increasing gap between rural and urban suicide rates in Austria ( 13 ). At the beginning of the 1970s, urban regions experienced higher suicide rates than rural ones; however, this ratio changed by the mid-1980s, and the disparity between rural and urban suicides continues to grow, with suicide rates falling more notably in urban areas than in rural ones ( 13 ). Further studies should examine whether improvements in access to mental health care and socioeconomic changes in urban areas are in line with the greater reductions in urban suicide rates compared with rural rates.
Barriers to psychotherapist and psychiatrist care
Although social insurance expenditures for psychotherapy have grown in recent years in Austria, demand-planning authorities have recognized that the need for reimbursement of psychotherapy visits is far from met. Waiting periods of up to 30 weeks are common. Of a total of 1.4 million reimbursed visits for psychotherapy in 2007, 36% were only partially reimbursed—at approximately 30% of the cost per visit ( 33 ). Thus access to psychotherapy depends on patients' socioeconomic situation. Similarly, because only 20% of all psychiatrist practices in Austria are contracted with social insurance, waiting periods of up to three months are typical for a first appointment covered by social insurance ( 33 ).
Economic conditions also determine the behavior of psychiatrists and psychotherapists. It is recognized and has been shown in this study that psychotherapists and psychiatrists are not as likely to reside in more deprived rural areas with a low mean income as they are in more urban areas ( 6 , 7 ). In addition, psychiatrists who contract with the social insurance system in Austria receive lower fees compared with fees received from self-payers. A similar situation appears to exist in the United States, where psychiatrists who accept new patients have been shown to prefer self-payers rather than patients with private insurance, Medicare, or Medicaid ( 37 ).
Limitations
The naturalistic design of this study does not allow conclusions about the effects of individual access to mental health providers on suicidality or about causal relationships. Although the statistical model accounted for the most common covariates and for spatial correlation, other factors not included could affect the results. For example, the proportion of persons divorced in each district was not available, although divorce has been described as a factor in suicide rates ( 38 ). Similarly, it is not known to what extent the population density of psychiatrists, psychotherapists, and general practitioners reflects service utilization or how different waiting periods could affect this relationship. Finally, we had to pool suicide data from 1991 to 2005 because of low incidences in some districts; however, pooling probably had little effect because of the temporal stability of suicide patterns in a given district.
Conclusions
Pirkola and colleagues ( 19 ) pointed to a possible advantage of community-based outpatient treatment over inpatient treatment in terms of suicide prevention. This analysis of Austrian data points to another aspect of outpatient-based suicide prevention. A remarkable nationwide increase in antidepressant prescriptions has occurred in Austria since the introduction of selective serotonin reuptake inhibitors. In addition, there was a simultaneous increase in the density of psychotherapists between 1991 and 2005. Both of these factors have been shown to correlate with an overall decrease in the suicide rate in Austria, which suggests an improvement in Austrian mental health care ( 39 ).
Nevertheless, this small-area analysis has provided evidence that access to mental health care cannot be viewed as independent from regional socioeconomic factors: the density of psychiatrists and psychotherapists is higher in urbanized areas with higher income, where suicide rates are low. Thus access and demand are unbalanced in Austria. As recommended in the United States ( 40 ) and many other countries ( 41 ), reducing socioeconomic barriers to mental health care, such as by increasing reimbursement of psychotherapy and promoting settlement of psychiatrists and psychotherapists in rural areas, is a desirable goal for the Austrian mental health system.
Acknowledgments and disclosures
The authors report no competing interests.
1. Harris EC, Barraclough B: Suicide as an outcome for mental disorders: a meta-analysis. British Journal of Psychiatry 170:205–228, 1997Google Scholar
2. Hawton K, van Heeringen K: Suicide. Lancet 373:1372–1381, 2009Google Scholar
3. Luoma JB, Martin CE, Pearson JL: Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry 159:909–916, 2002Google Scholar
4. Chisholm D, Flisher AJ, Lund C, et al: Scale up services for mental disorders: a call for action. Lancet 370:1241–1252, 2007Google Scholar
5. Salvador-Carulla L, Tibaldi G, Johnson S, et al: Patterns of mental health service utilisation in Italy and Spain: an investigation using the European Service Mapping Schedule. Social Psychiatry and Psychiatric Epidemiology 40:149–159, 2005Google Scholar
6. Freeman-Cook A, Hoas H: Hide and seek: the elusive rural psychiatrist. Academic Psychiatry 31:419–422, 2007Google Scholar
7. Nelson WA, Pomerantz A, Schwartz J: Putting "rural" into psychiatry residency training programs. Academic Psychiatry 31:423–429, 2007Google Scholar
8. Scully JH, Wilk JE: Selected characteristics and data of psychiatrists in the United States, 2001–2002. Academic Psychiatry 27:247–251, 2003Google Scholar
9. Johnson ME, Brems C, Warner TD, et al: Rural-urban health care provider disparities in Alaska and New Mexico. Administration and Policy in Mental Health and Mental Health Services Research 33:504–507, 2006Google Scholar
10. Johnstone B, Nossaman LD, Schopp LH, et al: Distribution of services and supports for people with traumatic brain injury in rural and urban Missouri. Journal of Rural Health 18:109–117, 2002Google Scholar
11. Odisho AY, Fradet V, Cooperberg MR, et al: Geographic distribution of urologists throughout the United States using a county level approach. Journal of Urology 181:760–765, 2009Google Scholar
12. Hirsch JK: A review of the literature on rural suicide: risk and protective factors, incidence, and prevention. Crisis 27:189–199, 2006Google Scholar
13. Kapusta ND, Zorman A, Etzersdorfer E, et al: Rural-urban differences in Austrian suicides. Social Psychiatry and Psychiatric Epidemiology 43:311–318, 2008Google Scholar
14. Rutz W, Wålinder J, Eberhard G, et al: An educational program on depressive disorders for general practitioners on Gotland: background and evaluation. Acta Psychiatrica Scandinavica 79:19–26, 1989Google Scholar
15. Rihmer Z, Rutz W, Barsi J: Suicide rate, prevalence of diagnosed depression and prevalence of working physicians in Hungary. Acta Psychiatrica Scandinavica 88:391–394, 1993Google Scholar
16. Leff HS, McPartland JC, Banks S, et al: Service quality as measured by service fit and mortality among public mental health system service recipients. Mental Health Services Research 6:93–107, 2004Google Scholar
17. Gibbons RD, Hur K, Bhaumik DK, et al: The relationship between antidepressant medication use and rate of suicide. Archives of General Psychiatry 62:165–172, 2005Google Scholar
18. Tondo L, Albert MJ, Baldessarini RJ: Suicide rates in relation to health care access in the United States: an ecological study. Journal of Clinical Psychiatry 67:517–523, 2006.Google Scholar
19. Pirkola S, Sund R, Sailas E, et al: Community mental-health services and suicide rate in Finland: a nationwide small-area analysis. Lancet 373:147–153, 2009Google Scholar
20. Ying YH, Chang K: A study of suicide and socioeconomic factors. Suicide and Life Threatening Behavior 39:214–226, 2009Google Scholar
21. Berk M, Dodd S, Henry M: The effect of macroeconomic variables on suicide. Psychological Medicine 36:181–189, 2006Google Scholar
22. Rehkopf DH, Buka SL: The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychological Medicine 36:145–157, 2006Google Scholar
23. Gunnell DJ, Peters TJ, Kammerling RM, et al: Relation between parasuicide, suicide, psychiatric admissions, and socioeconomic deprivation. British Medical Journal 311:226–230, 1995Google Scholar
24. Lester D: Explaining regional differences in suicide rates. Social Science and Medicine 40:719–721, 1995Google Scholar
25. Middleton N, Sterne JAC, Gunnell D: The geography of despair among 15- to 44-year-old men in England and Wales: putting suicide on the map. Journal of Epidemiology and Community Health 60:1040–1047, 2006Google Scholar
26. Cooper RA, Getzen TE, Laud P: Economic expansion is a major determinant of physician supply and utilization. Health Services Research 38:675–696, 2003Google Scholar
27. Macintyre S, Ellaway A, Cummins S: Place effects on health: how can we conceptualise, operationalise and measure them? Social Science and Medicine 55:125–139, 2002Google Scholar
28. Pritchard C: New patterns of suicide by age and gender in the United Kingdom and the Western World 1974–1992: an indicator of social change? Social Psychiatry and Psychiatric Epidemiology 31:227–234, 1996Google Scholar
29. Colucci E, Martin G: Religion and spirituality along the suicidal path. Suicide and Life Threatening Behavior 38: 229–244, 2008Google Scholar
30. Congdon P: Monitoring suicide mortality: a Bayesian approach. European Journal of Population 16:251–284, 2000Google Scholar
31. R: A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing, 2009. Available at www.R-project.org Google Scholar
32. Thomas A, O'Hara B, Ligges U, et al: Making BUGS Open. R News 6:12–17, 2006. Available at CRAN.R-project.org/doc/Rnews Google Scholar
33. Provision of Psychotherapy and Psychopharmacotherapy 2007 [in German]. Vienna, Austrian Health Institute, 2009Google Scholar
34. Rose G: Sick individuals and sick populations. International Journal of Epidemiology 14:32–38, 1985Google Scholar
35. Mortensen PB, Agerbo E, Erikson T, et al: Psychiatric illness and risk factors for suicide in Denmark. Lancet 355:9–12, 2000Google Scholar
36. Stuckler D, Basu S, Suhrcke M, et al. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet 374:315–323, 2009Google Scholar
37. Wilk JE, West JC, Narrow WE, et al: Access to psychiatrists in the public sector and in managed health plans. Psychiatric Services 56:408–410, 2005Google Scholar
38. Stack S: Suicide: a 15 year review of the sociological literature: part II. modernization and social integration. Suicide and Life Threatening Behavior 30:163–176, 2000Google Scholar
39. Kapusta ND, Niederkrotenthaler T, Etzersdorfer E, et al: Influence of psychotherapist density and antidepressant sales on suicide rates. Acta Psychiatrica Scandinavica 119:236–242, 2009Google Scholar
40. Miller CL, Druss B: Suicide and access to care. Psychiatric Services 50:1566, 2001Google Scholar
41. Jacob KS, Sharan P, Mirza I, et al: Mental health systems in countries: where are we now? Lancet 370:1061–1077, 2007Google Scholar



