Outcomes of Critical Time Intervention Case Management of Homeless Veterans After Psychiatric Hospitalization
People with serious mental illness are at high relative risk of homelessness ( 1 ). Previous research has suggested that transitions from institutional settings to community settings represent especially high-risk periods because of the potential for gaps in both mental health and housing assistance services ( 2 ). Community case management can be an important tool in bridging services gaps during these transitions ( 3 ).
Critical time intervention (CTI) is a case management model developed at Columbia University to address the needs of homeless people with chronic mental illness during transitions from institutional settings to the community ( 2 , 4 , 5 ). CTI was developed in response to observed high recurrences of homelessness after community placement from a shelter-based mental health program in New York. CTI case managers provide time-limited intensive support and assess resources for the transition to community living, identify potential crises, monitor treatment plans, and focus on the transfer of care to mainstream community resources. CTI can be distinguished from many case management models in its application to the transition from institution to community and its emphasis on transfer of care to community resources.
A randomized clinical trial showed CTI to be effective in reducing the recurrence of homelessness among men with severe mental illness who were entering community housing from a long-term shelter. CTI clients experienced 33% fewer days homeless relative to a "usual services" comparison group ( 4 ).
There has been increasing interest in recent years in methods for disseminating evidence-based practices in large service systems ( 6 ). From 2001 to 2004, the Department of Veterans Affairs (VA) implemented a modified version of CTI at eight VA medical centers (VAMCs) for homeless veterans with serious mental illness who were current inpatients. Homeless inpatients are at high risk of continued homelessness as well as rehospitalization and were thus identified as a priority group for this intervention ( 7 ). This report summarizes the implementation of this project and presents a multisite evaluation of its effectiveness.
Methods
Program design and implementation
The project was implemented at eight VAMCs with the use of a nonrandomized pre-post cohort design with a one-year quarterly follow-up. The eight sites were located in Chicago and Hines, Illinois; Houston; Lyons, New Jersey; Montrose, New York; Richmond and Salem, Virginia; and San Diego. These sites were selected because each historically had a large number of inpatient clients who were homeless or at risk of homelessness and local medical center managers expressed interest in and support for the project. Also, VA desired to implement programs in different regions of the country. Institutional review board (IRB) approval was obtained at the authors' parent institution and at each of the medical centers in the study.
Before the first phase, a CTI case manager was hired at each site. All case managers were master's-level social workers. Each project site had only one staff member, and IRB agreements precluded the use of random assignment to treatment groups; therefore, implementation of the project then proceeded in two sequential phases. In the first phase, a cohort was recruited from inpatient psychiatric units and provided written informed consent to participate in a follow-up study. These veterans received usual discharge planning services from inpatient unit staff and standard referral to available outpatient services. Recruitment criteria included a diagnosis of a serious mental disorder (schizophrenia or other psychotic disorder, mood disorder, or posttraumatic stress disorder, as determined from inpatient chart review), recent homelessness or imminent risk of homelessness (based on client self-report), intention to remain in the geographic area for at least a year, and agreement to participate in the follow-up interviews.
CTI case managers regularly visited inpatient units to screen potential clients; they determined satisfaction of these criteria through a brief interview with the client as well as consultation with inpatient unit staff. CTI case managers had minimal clinical contact with phase 1 participants, making an initial referral to outpatient services but providing no further direct services. Rather, the case managers' activity was directed to the implementation of the evaluation, recruiting participants, obtaining informed consent from potential participants, and conducting structured baseline and quarterly follow-up interviews for one year. These activities were monitored and supported by monthly conference calls with central project administrators. Thus phase 1 involved no specific training or clinical intervention other than linkage with standard VA outpatient services.
Before the second phase, case managers were trained in the CTI model by clinical staff from the Department of Psychiatry, College of Physicians and Surgeons, and the Department of Epidemiology of the Mailman School of Public Health, both of Columbia University, which originated CTI. Orientation took place during a two-day meeting and included discussions with CTI case managers from the Columbia project and visits to community supportive housing sites in New York City.
Ongoing supervision from Columbia staff was carried out through biweekly conference calls, during which current cases from each project site were reviewed. The purpose of the clinical supervision was to ensure fidelity to the CTI model and to deepen the understanding of the case manager-client relationship. For example, discussions included how problems in the relationship might impede progress and how to address those problems through various motivational, interpretive, and cognitive-behavioral techniques. Although this ongoing supervision supported fidelity to the CTI model, no quantitative measure of fidelity was undertaken. Monthly administrative conference calls continued to support program implementation and evaluation efforts. Case managers recruited veterans for phase 2 using the same procedures and criteria as phase 1. Case managers continued to interview phase 1 participants while implementing phase 2, but managers were instructed to provide no clinical services to the phase 1 clients.
Study sample
Recruitment was conducted from February 1, 2001, to August 31, 2004. A total of 278 participants were recruited during phase 1, and an additional 206 participants were recruited in phase 2, for a total of 484 participants. Efforts were made to collect quarterly follow-up data for one year on all veterans regardless of clinical program status.
Measures
Baseline and follow-up client interviews. Baseline interviews were conducted shortly after recruitment and averaged 1.0–1.5 hours. Case managers conducted the interviews in both phases. Case managers were instructed on interview techniques, with emphasis on the need for neutral presentation of items and recording of client responses. All clients gave written informed consent and were paid $10 for each interview.
Background characteristics. Demographic characteristics included age, race, marital status, education, and military service history.
Housing and income. Housing status was measured by items concerning the number of days in the past 90 that clients were homeless (living in shelters or on the streets), living in an institution (hospital, residential treatment facility, or jail), or housed (living in their own home or with others).
Substance use and mental health. Recent alcohol use, drug use, and occurrence of psychiatric symptoms were assessed with complete scales from the Addiction Severity Index (ASI) ( 8 ).
CTI case management reports
CTI services were documented by monthly reports submitted by CTI case managers during the first six months of each client's involvement and by quarterly reports thereafter. These reports documented case management status (including reasons for ending CTI case management if applicable), number and duration of contacts, and types of direct services provided. The case management report form was structured so that case managers chose from a fixed number of categories (for example, reasons for the client's ending case management); however, choice within these categories was based on each case manager's clinical judgment.
VA administrative databases
Documentation of outpatient mental health care services received by phase 1 clients ("usual services") came from VA administrative databases. These data record visits to psychiatric or substance abuse treatment clinics but do not specify treatment modality.
Data analysis plan
Participants in phase 1 and phase 2 were compared on baseline characteristics with chi square tests and t tests. Mixed-regression models were then used to compare outcomes between phases over the one-year follow-up period. The analyses controlled for baseline differences and project site with the MIXED procedure of SAS ( 9 ) and α =.05. All completed interviews were included in longitudinal analyses whether or not clients were actively participating in CTI case management.
Results
Recruitment and follow-up rates
A total of 484 clients were recruited into the project: 278 into phase 1 and 206 into phase 2. (Two project sites failed to implement the program because of difficulties in hiring and retaining case managers coupled with an inability to recruit clients who met inclusion criteria). Overall follow-up rates across all time periods in phase 1 averaged 56% (625 of 1,112 possible interviews) and in phase 2 averaged 56% (459 of 824 possible interviews). There was no significant phase difference in the percentage of follow-up interviews completed. Being married at baseline was the only client characteristic that was associated with the number of follow-up interviews completed (p=.006).
Baseline client characteristics
Client characteristics at baseline are summarized in Table 1 . Clients in the two phases were recruited according to the same criteria and were similar on many salient dimensions, including demographic characteristics, lifetime homelessness, recent residential status, and recent alcohol use. The few significant group differences at baseline showed that fewer phase 2 clients were usually employed full-time at baseline and more had disabilities or were retired at baseline. In addition, phase 2 clients used drugs for fewer days, spent less money on drugs in the 30 days preceding baseline, and had lower ASI drug scale scores. Measures on which significant group differences were observed at baseline were included as covariates in outcomes analyses.
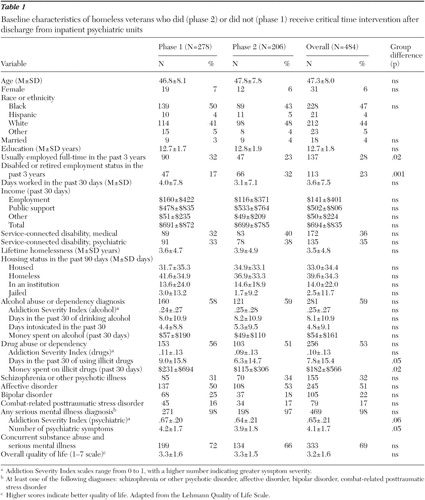 |
CTI case management
Duration and reasons for ending case management. The planned length of CTI services for phase 2 clients was six months, with exceptions at the case manager's discretion. (The planned duration of CTI services in the current project was somewhat shorter than the nine months recommended by the originators of the model. The intention was to increase the number of clients seen by the lone case manager at each project site). The average duration of CTI services was approximately seven months (212 days), with 53% involved for 180 days or less. During phase 2, typical caseload size per case manager was ten clients; caseload very rarely exceeded 15 per case manager at any of the project sites.
Successful accomplishment of significant clinical goals was the most common reason for ending case management (39%), followed by completion of limited improvement (22%). Less successful reasons for ending case management included clients' inability to tolerate CTI (19%), moving out of the area (15%), and returning to active substance abuse (13%). These categories are not mutually exclusive, and responses were based on the clinical judgment of the case manager.
Case management contacts and services.Table 2 shows the average number of CTI case management contacts at baseline and each of the follow-ups (in-person visits). These data reflect relatively intensive case management, with an average of five contacts during the first month. The number of contacts per month was fewer at each subsequent follow-up interval and averaged two at nine and at 12 months.
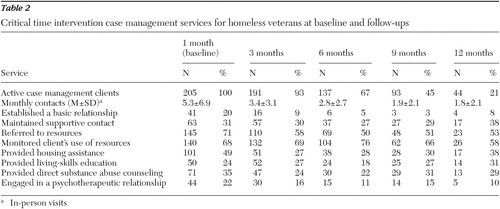 |
Also shown in Table 2 , the three most prevalent activities at the one-month report were making referrals to other agencies for resources such as financial benefits and treatment services (71%), monitoring clients' use of those resources (68%), and providing housing assistance (49%). Direct service activities, such as living-skills education (24%), direct substance abuse counseling (35%), and psychotherapy (22%), were less frequent but occurred in a substantial number of cases at the one-month report.
In summary, these process data suggest that the CTI program provided relatively intensive but time-limited case management and that most clients ended case management successfully in the view of their case manager.
VA outpatient mental health services
In order to document the treatment of phase 1 clients, we summarized VA outpatient mental health services from administrative data. Over the course of the one-year follow-up, approximately 68% of phase 1 clients used VA outpatient mental health services (which includes any psychiatric or substance abuse treatment; these data record clinic visits rather than specific treatment procedures). Among users of these services, the mean±SD number of visits was 68.7±87.6. A comparable summary for phase 2 clients showed that approximately 75% used VA mental health outpatient services during the one-year follow-up. The number of visits among users was 72.8±85.7. These data show that standard VA discharge planning and referral services were successful in connecting most phase 1 participants to VA outpatient mental health services; their utilization was only slightly lower than that observed for phase 2 clients.
Client outcomes
Regression statistics for all client outcomes are summarized in Table 3 .
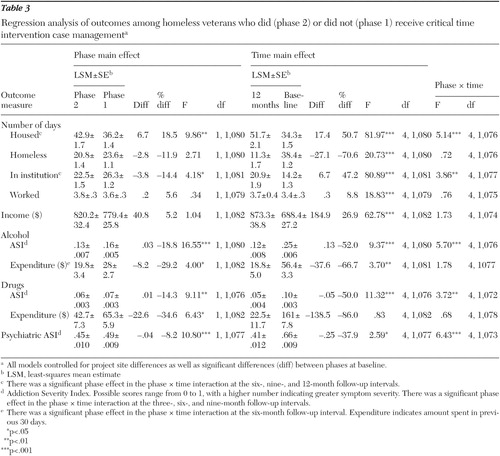 |
Housing. On average, phase 2 clients reported 6.7 (19%) more days housed in the previous 90 than those in phase 1 (p=.002). Both groups significantly increased the number of days housed over the one-year follow-up (p<.001). However, phase 2 clients had significantly more days housed at the six-, nine-, and 12-month follow-up intervals (p=.02, p=.001, and p=.001, respectively).
There was no overall effect of treatment cohort on number of days of homelessness. However, both groups significantly decreased the number of days spent homeless over the course of follow-up (p<.001).
Phase 2 clients on average reported significantly fewer days in institutions during the previous 90 than phase 1 clients (p=.041). As would be expected for clients recruited from hospitals, the number of days in institutions first increased, then decreased over the course of follow-up. Phase 2 clients spent significantly fewer days in institutional settings at the six-, nine-, and 12-month follow-up intervals (p=.01, p=.001, and p=.001, respectively).
Employment and income. There was no difference between phases in the number of days worked in the 30 days before the interview or in total monthly income. There was a small but statistically significant increase in the number of days worked over the course of the follow-up interval (p<.001). Change in the number of days worked over the course of follow-up was not different for the two groups. Similarly, there was a significant increase in total income over the course of the follow-up interval (p<.001). However, change in total monthly income over the course of follow-up was not different for the two groups.
Alcohol use. On average, phase 2 clients used less alcohol than phase 1 clients did (p<.001). Both groups significantly decreased alcohol use over the one-year follow-up (p<.001). However, phase 2 clients had significantly lower alcohol use than phase 1 clients at the three-, six-, and nine-month follow-up intervals (p<.001, p<.001, and p=.001, respectively).
Phase 2 clients on average spent less on alcohol in the previous 90 days than phase 1 clients (p=.046). Both groups significantly decreased spending on alcohol over the course of the one-year follow-up (p=.003). The only between-group difference on this measure was at the six-month follow-up interval (p=.02).
Drug use. On average, phase 2 clients had lower illicit drug use than phase 1 clients (p=.004). Both groups significantly decreased drug use over the one-year follow-up (p<.001); however, phase 2 clients had significantly lower drug use at the three-, six-, and nine-month follow-up intervals (p<.001, p<.001, and p=.04, respectively).
Phase 2 clients on average spent less on illicit drugs in the previous 90 days than phase 1 clients spent (p=.011). There was no significant change in expenditure over the course of the one-year follow-up. The only between-group difference on this measure was at the six-month follow-up interval (p=.035).
Psychiatric problems. On average phase 2 clients reported fewer psychiatric problems than phase 1 clients (p=.001). Both groups reported significantly fewer psychiatric problems over the one-year follow-up (p=.035). However, phase 2 clients had significantly fewer psychiatric problems at the three-, six-, and nine-month follow-up intervals (p<.001, p<.001, and p=.005, respectively).
Discussion
The purpose of this study was to evaluate an effort to disseminate a program of CTI case management for homeless veterans with mental illness being discharged from VA psychiatric inpatient units. Clients who were offered CTI case management spent more days housed and fewer days in institutional settings than clients receiving usual VA services. CTI case management clients also reported lower alcohol use, drug use, and psychiatric problems. In contrast to the between-group differences in housing, which persisted through the end of the 12-month follow-up, between-group differences on clinical measures such as alcohol use, drug use, and psychiatric problems were seen only at the intermediate follow-up intervals (at three, six, and nine months). This finding was principally due to continued improvement of the phase 1 group, who received usual VA services that included access to outpatient mental health treatment and less intensive specialized services for homeless veterans but not CTI.
These generally positive results were the product of both educational and clinical interventions of relatively limited intensity. One case manager was hired at each project site, and the CTI model was implemented through modestly intensive but sustained training of these case managers. Training was characterized by limited in-person meetings and a heavy reliance on teleconference case review. This strategy was quite different from the original CTI program, which was located in New York City and involved regular face-to-face meetings of all CTI team members. The current long-distance implementation strategy had mixed results across project sites, with two sites essentially failing to implement the case management model in phase 2 because of an inability to hire and retain CTI case managers and to recruit clients who met inclusion criteria. Rosenheck and Mares ( 10 ) used a similar teleconference-based dissemination strategy in their study of supported employment in the VA, with successful implementation at most but not all sites.
The current results are generally consistent with the results of studies of the original CTI project. Susser and colleagues ( 4 ) found a reduced number of days homeless that persisted beyond the end of the case management intervention. Herman and colleagues ( 11 ) reported significantly greater improvement for CTI clients on measures of psychiatric symptoms.
A shortcoming of this evaluation is that clients were not randomly assigned to receive CTI or usual services. As a result, we cannot be certain that outcome results are entirely attributable to the program intervention, because differences in the groups at baseline also may have contributed to differences in study outcomes at follow-up. To minimize the influence of such selection biases, we used multiple regression analysis to adjust our assessment of outcomes for baseline differences.
Another limitation comes from the relatively low follow-up rates in the study, which could make the results from later time intervals less representative of the client group that started the study. However, dropout was similar across treatment cohorts and was not associated with more serious problems at baseline. Thus dropout most likely did not bias between-group comparisons. In addition, the current use of mixed-model regression analysis conserved as much statistical power as possible by keeping all observations in the model even if participants had not completed all interviews.
Substance abuse was assessed only by self-report in this study. Similarly, our only measure of psychiatric symptoms came from self-reports. This may be problematic because the client's case manager conducted the assessment interviews. There is some risk of reporting bias; however, there is little reason to think it would be substantially greater in one phase rather than the other. Veterans in phase 2 had more regular contact with CTI case managers than those in phase 1, which could have either improved the accuracy of self-reports or increased the motivation to provide socially desirable data.
Finally, although the results presented in this article suggest that CTI was effectively implemented and deserves further dissemination as an evidence-based intervention, we did not conduct a qualitative study of organizational factors that facilitated or impeded this effort. Data on site variations in leadership, support, and training could be helpful in guiding future efforts of this type.
Conclusions
This study provides evidence that a sustained training program principally based on teleconference clinical supervision can be used to implement the CTI case management model in mental health systems such as VA. It also showed that such dissemination efforts can yield improved housing and clinical outcomes in a particularly challenging clinical population.
Acknowledgments and disclosures
Gay Koerber, M.A., in VA Central Office provided overall leadership of this project. Alan Felix, M.D., and Daniel Herman, D.S.W., of Columbia College of Physicians and Surgeons provided CTI training; Dr. Felix provided ongoing clinical supervision to project clinicians. The authors thank the CTI case managers: Jessica Brian and Jim Fiedler (San Diego), Joann Edwards and Donna Fuchs (Lyons, N.J.), Mary Elizabeth Ellis (Richmond, Va.), Elizabeth Gallichio (Hines, Ill.), Karen Mannos (Chicago), Marla Moore and Erica Roy (Salem, Va.), Theresa Riha (Houston, Tex.), and Linda Spencer (Montrose, N.Y.).
The authors report no competing interests.
1. Koegel P, Burnam A, Baumohl J: The causes of homelessness, in Homelessness in America. Edited by Baumohl J. Phoenix, Ariz, Oryx, 1996Google Scholar
2. Valencia E, Susser E, McQuistion H: Critical time points in the clinical care of homeless mentally ill individuals, in Practicing Psychiatry in the Community: A Manual. Edited by Vacaro JV and Clarke GH Jr. Washington, DC, American Psychiatric Press, 1996Google Scholar
3. Morse GA: A review of case management for people who are homeless: implications for practice, policy and research. Presented at Department of Health and Human Services Workshop on Exemplary Practices Addressing Homeless and Health Care Issues, Washington, DC, Oct 29–30, 1998Google Scholar
4. Susser E, Valencia E, Conover S, et al: Preventing recurrent homelessness among mentally ill men: a critical time intervention after discharge from a shelter. American Journal of Public Health 87:256–262, 1997Google Scholar
5. Herman D, Conover S, Felix A, et al: Critical time intervention: an empirically supported model for preventing homelessness in high-risk groups. Journal of Primary Prevention, in pressGoogle Scholar
6. Drake RE, Becker DR, Goldman HH, et al: The Johnson & Johnson-Dartmouth community mental health program: disseminating evidence-based practice. Psychiatric Services 57:302–304, 2006Google Scholar
7. Rosenheck RA, Seibyl C: Costs of homelessness: health service use and cost. Medical Care 36:1256–1264, 1998Google Scholar
8. McLellan AT, Luborsky L, Woody GE, et al: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease 168:26–33, 1980Google Scholar
9. SAS STAT 9.1 Users Guide. Cary, NC, SAS Corp, 2003Google Scholar
10. Rosenheck RA, Mares AS: Implementation of supported employment for homeless veterans with psychiatric or addiction disorders: two-year outcomes. Psychiatric Services 58:325–333, 2007Google Scholar
11. Herman DS, Opler L, Felix A, et al: A critical time intervention with mentally ill homeless men: impact on psychiatric symptoms. Journal of Nervous and Mental Disease 188:135–140, 2000Google Scholar



