The Clinical Profile and Service Needs of Hospitalized Adults With Mental Retardation and a Psychiatric Diagnosis
Abstract
OBJECTIVE: This study compared patients with both mental retardation and a psychiatric diagnosis with patients who did not have co-occurring mental retardation who were served in Ontario's tertiary mental health care system in terms of demographic characteristics, symptom profile, strengths and resources, and clinical service needs. METHODS: A secondary analysis of data from the Colorado Client Assessment Record (CCAR) that were collected between 1999 and 2003 from all tertiary psychiatric hospitals in Ontario, Canada, was completed for a random sample of 3,927 cases, representing 12,470 patients receiving psychiatric services. RESULTS: Patients with both mental retardation and a psychiatric diagnosis differed from those who did not have mental retardation in terms of demographic characteristics, diagnostic and symptom profile, resources, and recommended level of care. More specifically, patients with both mental retardation and a psychiatric diagnosis had significantly worse ratings across nearly all CCAR functional domains and were assessed as requiring more than the recommended levels of care compared with other patients. CONCLUSIONS: Patients who have both mental retardation and a psychiatric diagnosis constitute a sizeable subgroup of an already underserved psychiatric hospital population. Greater attention is required to meet the unique clinical and service needs of this challenging group.
In Canada and other parts of the world, psychiatric services for persons with mental retardation, as defined in DSM-IV-TR, were once provided through institutions. In the 1970s, plans to downsize and close these institutions were initiated, and, since then, persons with mental retardation have been directed to the generic mental health system for their psychiatric needs (1). Little information is available about how patients with both mental retardation and a psychiatric disorder differ from those who do not have intellectual impairments in terms of their demographic characteristics, symptom profile, and clinical needs. Such information is critical to delivering effective mental health services to these patients (2).
A small number of studies have compared persons with and without co-occurring mental retardation who are receiving psychiatric services (3,4,5,6,7,8). These studies have shown that the patients with mental retardation are typically younger, are more likely to live in dependent living settings (with family or in group homes), and are less likely to be married or have children. With regard to symptom profile, they tend to have higher rates of comorbid medical conditions, more problems with aggression, and lower rates of substance abuse compared with other patients. In terms of aggression, patients with mental retardation have been reported to display more assaultive behavior and to receive more chemical and physical seclusion and restraint than other patients (4,6,9,10).
Lohrer and associates (6) and Saeed and colleagues (4) reported a longer stay for inpatients who had both mental retardation and a psychiatric diagnosis than for patients who did not have mental retardation. Several researchers have commented on the intensive clinical needs of this patient group and the high level of care required if they are to be supported outside the hospital (4,11,12,13,14,15). However, no studies have directly compared the level of services required by patients who have mental retardation and a comorbid psychiatric illness with the levels required by other groups of patients.
The study reported here compared the clinical profile and service needs of patients with both mental retardation and a psychiatric diagnosis with those of other patients receiving tertiary-level mental health care in Ontario. The goals of the study were to determine the prevalence of co-occurring mental retardation within the tertiary care psychiatric hospital system, to examine the patient characteristics and symptom profile of the group with both mental retardation and a psychiatric diagnosis compared with those of other patients receiving tertiary mental health care, and to calculate and compare the recommended level of care for those with and without mental retardation.
Methods
Sample and data collection
Patients were drawn from all nine provincial psychiatric hospitals responsible for providing tertiary inpatient and outpatient mental health services to urban, semiurban, and rural communities in Ontario, Canada, between 1999 and 2003. Tertiary inpatient programs provide mental health beds for persons with complex or chronic conditions for the purpose of specialized assessment and treatment. Such programs provide the highest level of care in the mental health service continuum in Ontario. Tertiary outpatient programs also target patients who have more complex conditions and represent the middle ground between specialized inpatient and community-based mental health care. All programs included in this study serve persons aged 16 years or older with severe and persistent mental illness.
For each hospital facility, all individuals receiving inpatient services on a specified census day were assessed. It was believed that this approach would yield a stable estimate of which patients received inpatient services, because these patients tend to be admitted for chronic conditions. In fact, patients' average length of stay was 3.65 years, and only 13 percent of inpatients were in the hospital for less than one month at the time of the survey. For the outpatient population, the sampling frame included all individuals who were using outpatient services during a three-month period.
The sample was drawn by using random selection, stratifying by clinical program. Sampling rates varied between 10 percent and 100 percent, with the aim of obtaining a minimum sample of 30 patients per program. For the purpose of generating population estimates, individual cases were then assigned weights based on the sampling rate per program. For example, if ten patients were assessed out of a total of 40, each patient would be given a weight of 4. Given that all inpatients were assessed, each inpatient case was given a weight of 1. The final study database comprised 3,927 cases, weighted to represent 2,218 inpatients and 10,323 outpatients, for a total of 12,541 patients (16). Institutional review board approval for conducting secondary analyses to compare patients with and without co-occurring mental retardation was obtained.
For all selected cases, standardized assessments were completed by trained staff who were familiar with the patients who were being rated (17). An interview was not required. For each patient, staff indicated the presence or absence of a developmental disability. (In Ontario, the term "developmental disability" is equivalent to the term "mental retardation" in DSM-IV-TR). Staff also reported any psychiatric diagnoses, including mental retardation. A patient was identified as having co-occurring mental retardation if he or she was recorded as having a developmental disability or a mental retardation diagnosis in addition to a psychiatric diagnosis (18). Using these criteria, we excluded a small number of cases (N=71, weighted) for which there was a designation of developmental disability or a diagnosis of mental retardation, but a precise psychiatric diagnosis was unknown or unavailable. This approach resulted in a final weighted total of 12,470 patients for analysis.
Measure
The assessment included completion of the Colorado Client Assessment Record (CCAR). The CCAR is a standardized tool for conducting a comprehensive assessment of patient functioning (19,20). Staff record basic patient information, such as current diagnosis and history of illness; legal, marital, employment, and educational status; and residential stability. Also, on the basis of his or her knowledge of the patient, input from other staff, and program records and charts, staff assess patient impairments and strengths across 25 domains and two global ratings. Each domain is rated on a 9-point scale from 1 (high functioning, no special problem) to 9 (low functioning, extreme problem of difficulty). Information from the CCAR is used to calculate a "recommended level of care" for each patient. The CCAR has been found to be both reliable and valid in the United States and in Ontario (17,21,22).
Level-of-care assessment
A level-of-care template was developed to provide a systematic approach for matching an individual to a particular level of care on the basis of need. The template is intended to support needs-based service planning for various patient groups.
An individual's recommended level of care is calculated through use of an algorithm based on ratings from six CCAR domains: security or management risk, overall problem severity, self-care and basic needs, overall lack of resources, danger to self, and danger to others. Patients were assigned to one of five recommended levels of care (Table 1) ranging from self-management (level 1) to specialized inpatient care (level 5) on the basis of their ratings on each of these six domains. Validity testing has supported the ability of the template to map patients who have more complex conditions into a higher recommended level of care (17).
Analyses
For patients with and without co-occurring mental retardation, frequencies of demographic characteristics, diagnoses, and recommended level of care were compared by using the chi square statistic and odds ratios. Symptom and resource ratings organized under three headings—adaptive behavior and cognition, challenging behavior, and lack of resources—were contrasted with analyses of variance (ANOVAs) for weighted data. To achieve an overall alpha level of .05, Bonferroni corrections were applied, which lowered the significance level for individual tests to .0016 (based on 31 comparisons in total). Analyses were performed with SPSS version 11 (23) and STATA (24) software (ANOVAs for weighted data).
Results
Prevalence of comorbid mental retardation
Of the final weighted sample of 12,470, which included 2,196 inpatients and 10,274 outpatients, 1,665 patients (13.4 percent)—394 inpatients, or 17.9 percent, and 1,271 outpatients, or 12.4 percent—were classified as having co-occurring mental retardation. Inpatients were significantly more likely to have both mental retardation and a psychiatric diagnosis than outpatients (χ2=48.05, p<.001). Initial analyses indicated that the pattern of differences between patients with and without co-occurring mental retardation was virtually identical across the inpatient and outpatient samples. Accordingly, we present findings for the combined group of inpatients and outpatients.
Patient characteristics and symptom profile
Patients with and without co-occurring mental retardation were compared in terms of their characteristics and psychiatric diagnoses (Table 2). Although patients with co-occurring mental retardation were slightly younger (mean age of 46 compared with 49 years), this age difference was not statistically significant once the Bonferroni correction for multiple comparisons was applied (F=7.06, df=1, 3824, p=.008). Inpatients with co-occurring mental retardation had significantly longer admissions than did those who did not have mental retardation (an average of 6.6 years compared with 3.0 years, F=85.95, df=1, 2123, p<.001). As indicated in Table 2, patients with both diagnoses were more likely to be unmarried, to be unemployed, and to have more comorbid medical conditions than those who did not have co-occurring mental retardation. Regarding psychiatric diagnoses, patients who had co-occurring mental retardation were less likely to have a mood, anxiety, or substance use disorder than those without mental retardation but were equally likely to receive a diagnosis of a psychotic, personality, or organic disorder.
Table 3 compares patients with and without co-occurring mental retardation on several CCAR domains, summarized under three relevant headings: adaptive behavior and cognition, challenging behavior, and lack of resources. Patients with co-occurring mental retardation were given a higher severity rating on almost every domain under these three headings compared with patients who did not have mental retardation. This pattern was also reflected in higher global ratings on problem severity and lack of strengths for those with both mental retardation and a psychiatric diagnosis than for other patients.
Recommended level of care
As can be seen from Table 4, a larger proportion of individuals with co-occurring mental retardation were recommended for level 3 care (42.8 percent compared with 31.9 percent) or level 4 care (27.3 percent compared with 15.1 percent), and significantly fewer were rated as being able to manage with less intensive supports (25.8 percent compared with 50.8 percent for levels 1 and 2 combined). Patients who had both mental retardation and a psychiatric diagnosis had a different distribution of levels of care than those without mental retardation (χ2=385.3, df=4, p<.001). However, the percentage of patients with recommended level-of-care ratings of 5 (tertiary inpatient care) was very low for both groups (4.0 percent and 2.2 percent). Thus patients with both diagnoses were not determined to be in greater need of tertiary-level inpatient care but were in greater need of more intensive outpatient supports than other patients.
Discussion
This study was conducted to determine the patient characteristics and clinical needs of persons with both mental retardation and a psychiatric diagnosis who were currently being served by the tertiary care psychiatric hospital system in Ontario. The results of the study provide important information for those planning services for this population. As many as one in eight individuals (13.4 percent) served by the tertiary mental health care system in Ontario have co-occurring mental retardation. Patients with both diagnoses differed from patients who did not have mental retardation with regard to demographic characteristics and tended to have a more severe diagnostic and symptom profile, a greater lack of resources, and a higher recommended level of care. Despite their more severe profiles, only a small percentage of patients with co-occurring mental retardation were rated as requiring long-term inpatient care (level 5). A majority were rated as requiring either intensive outpatient support (level 3) or residential treatment (level 4).
In terms of patient profiles, patients who had both mental retardation and a psychiatric diagnosis were more likely to be single, to be unemployed, to have comorbid medical conditions, and to have a longer stay than patients who did not have mental retardation. This presentation matches the profile reported by Saeed and associates (4), Hurley and colleagues (5), and Lohrer and colleagues (6) in their studies of patients in acute care settings. The patients with both diagnoses had lower rates of substance abuse, which has been reported elsewhere (6,8) and may be partly explained by the fact that persons with mental retardation have limited access to substances because of their supervised lifestyle (25).
The patients with co-occurring mental retardation who were included in the study reported here were found to have lower rates of mood and anxiety disorders than other patients. This finding is inconsistent with the general finding that persons with mental retardation have an increased risk of affective disorders (26). One explanation for our finding is that clinicians who do not have specialized training can underdiagnose or misdiagnose mood and anxiety disorders among persons with mental retardation (5,27). The lower rates may also reflect the fact that individuals with mental retardation and mood or anxiety disorders do not tend to receive the attention of tertiary-level services. Rather, it is those who have challenging behaviors, such as aggression, who receive such services (28,29).
In terms of patient profiles, the results of this study suggest that persons who have both mental retardation and a psychiatric diagnosis are disadvantaged as a result of adaptive behavior and cognitive limitations, challenging or aggressive behavior, and lack of resources. Adaptive limitations (poor attention and cognitive dysfunction) make it more difficult for patients who have co-occurring mental retardation to participate in treatments that have been developed for the "typical" patient (30,31). Compounding these functional limitations are problems with aggression to self and to others, referred to in the literature as "challenging behavior." Often, it is this challenging behavior rather than psychiatric symptoms that receives clinical attention (29,32) and jeopardizes community placements (13). Finally, persons with co-occurring mental retardation lack internal and external resources, which makes it difficult for them to obtain appropriate services, to maintain gains made in therapy, and to avoid regressing without extensive professional supports.
An important finding of this study from a service delivery perspective is that the recommended level of care for patients with co-occurring mental retardation is higher than for other patients. However, only a few patients in this study who had co-occurring mental retardation were deemed to require the highest level of support—inpatient tertiary care (level 5). This finding implies that a large percentage of individuals who were receiving level 5 care at the time of the study were deemed to require a lower recommended level of care. In other words, level 3 and 4 supports would be more appropriate for many of these individuals. Level 4 supports (highly staffed community residences with a strong therapeutic component) and level 3 supports (intensive case management services, such as specialized assertive community treatment teams) have evidenced some benefit for persons with lower functioning (33,34,35). Perhaps the longer stay among patients with co-occurring mental retardation in this study is in part a reflection of the shortage of level 3 and level 4 supports and the reluctance of agencies that provide intensive outpatient services to accept these more challenging, higher-need individuals. This question has been discussed by others in Ontario (4), the United States (13), and the United Kingdom (15).
An important caveat should be kept in mind in the interpretation of this study's findings. In this study, the patients with co-occurring mental retardation were defined as those who had a clinical diagnosis of mental retardation and a psychiatric disorder. Accurate psychiatric assessment of low-functioning individuals requires assessment from a psychiatrist or a psychologist who is specifically trained in making this type of dual diagnosis. Unfortunately, such specialist diagnostic skills have historically been limited in tertiary mental health services. Thus it is likely that a portion of our sample may have appeared clinically to have mental retardation but without correctly meeting DSM-IV criteria for mental retardation (IQ below 70, adaptive behavior deficits, and onset before age 18) (11). Similarly, it is likely that a number of patients in the group of patients with both diagnoses had been given a misdiagnosis—for example, psychotic-like behaviors may have led to diagnosis of psychosis when in fact the behaviors were related to another underlying cause (27,36).
This study had several limitations, which should be taken into consideration in interpreting its findings. First, data reported here are based on secondary analyses of data developed for another purpose. Issues such as accuracy of diagnoses of mental retardation or developmental disability and psychiatric diagnoses cannot be addressed by using this database, only through further research. Also, numbers reported here are estimates based on inpatients who were sampled on a given census day; not every outpatient was surveyed. Second, findings are based on the subgroup of persons with co-occurring mental retardation who were being served by Ontario's tertiary-level psychiatric hospitals. The study did not address the needs of patients obtaining services outside the tertiary care system or not receiving any services. Third, the findings may be unique to Ontario and not generalizable to other jurisdictions. Only comparable research in other places will address this issue. Finally, the level-of-care algorithm has demonstrated good concurrent validity, yet it is still relatively new and would benefit from further testing, especially in psychiatric populations with complex conditions.
Conclusions
One in eight patients served by Ontario's tertiary care psychiatric system were identified as having both mental retardation and a psychiatric disorder. These patients differed from patients who did not have co-occurring mental retardation in terms of demographic characteristics and tended to have a more severe diagnostic and symptom profile, a greater lack of resources, and a higher recommended level of care. Therefore, intensive services that match the greater needs of these patients (for example, care levels 3 and 4) must be made available to them. In addition, staff in the tertiary mental health care system would benefit from further training to better provide such services. The unique needs of patients with co-occurring mental retardation must be taken into consideration as part of mental health reform.
Acknowledgment
This research was supported by an Ontario Mental Health Foundation New Investigator Award.
Dr. Lunsky, Dr. Durbin, Mr. Koegl, Ms. Canrinus, and Dr. Goering are affiliated with the dual disorders program of the Centre for Addiction and Mental Health, 1001 Queen Street West, Unit 4-4, Toronto, Ontario, Canada M6J 1H4 (e-mail, [email protected]). Dr. Lunsky, Dr. Durbin, and Dr. Goering are also with the department of psychiatry of the University of Toronto, with which Dr. Bradley is affiliated. Dr. Bradley is also with the biomedical services and research division of the Surrey Place Centre in Toronto.
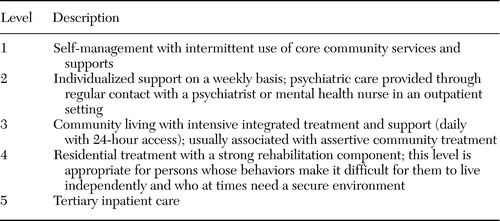 |
Table 1. Recommended level-of-care template for patients with both mental retardation and a psychiatric diagnosis
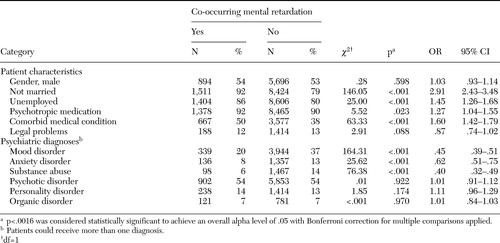 |
Table 2. Comparison of patient characteristics and psychiatric diagnoses among patients with both mental retardation and a psychiatric diagnosis and patients without co-occurring mental retardation
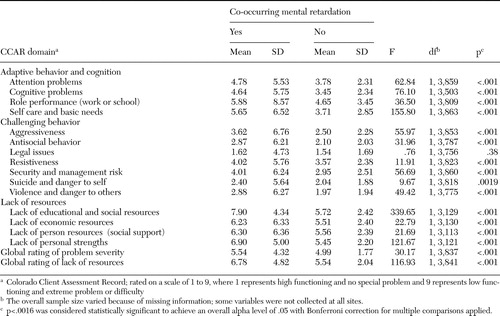 |
Table 3. Mean problem severity and resources among patients with both mental retardation and a psychiatric diagnosis and among patients without co-occurring mental retardation
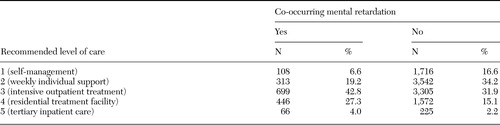 |
Table 4. Recommended level of care for patients with both mental retardation and a psychiatric diagnosis and for patients without cooccurring mental retardation
1. Zarfas DE: Mental health systems for people with mental retardation: a Canadian perspective. Australian and New Zealand Journal of Developmental Disabilities 14:3–7,1988Crossref, Google Scholar
2. Chaplin R: General psychiatric services for adults with intellectual disability and mental illness. Journal of Intellectual Disability Research 48:1–10,2004Crossref, Medline, Google Scholar
3. Glick M, Zigler E: Developmental differences in the symptomatology of psychiatric inpatients with and without mild mental retardation. American Journal of Mental Retardation 99:407–417,1995Medline, Google Scholar
4. Saeed H, Ouellette-Kuntz H, Stuart H, et al: Length of stay for psychiatric inpatient services: a comparison of admissions of people with and without developmental disabilities. Journal of Behavioral Health Services and Research 30:406–417,2003Crossref, Medline, Google Scholar
5. Hurley AD, Folstein M, Lam N: Patients with and without intellectual disability seeking outpatient psychiatric services: diagnoses and prescribing pattern. Journal of Intellectual Disability Research 47:39–50,2003Crossref, Medline, Google Scholar
6. Lohrer SP, Greene E, Browning CJ, et al: Dual diagnosis: examination of service use and length of stay during psychiatric hospitalization. Journal of Developmental and Physical Disabilities 14:143–158,2002Crossref, Google Scholar
7. Addington D, Addington JM, Ens I: Mentally retarded patients on general hospital psychiatric units. Canadian Journal of Psychiatry 38:134–136,1993Crossref, Medline, Google Scholar
8. Burge P, Ouellette-Kuntz H, Saeed H, et al: Acute psychiatric inpatient care for people with a dual diagnosis: patient profiles and lengths of stay. Canadian Journal of Psychiatry 47:243–249,2000Google Scholar
9. Tardiff K, Sweillam A: Assaultive behavior among chronic inpatients. American Journal of Psychiatry 139:212–215,1982Link, Google Scholar
10. Way BB, Banks SM: Use of seclusion and restraint in public psychiatric hospitals: patient characteristics and facility effects. Hospital and Community Psychiatry 41:75–81,1990Abstract, Google Scholar
11. Gustafsson C, Sonnander K: Occurrence of mental health problems in Swedish samples of adults with intellectual disabilities. Social Psychiatry and Psychiatric Epidemiology 39:448–456,2004Crossref, Medline, Google Scholar
12. Driessen G, DuMoulin M, Haverman MJ, et al: Persons with intellectual disability receiving psychiatric treatment. Journal of Intellectual Disability Research 41:512–518,1997Crossref, Medline, Google Scholar
13. Morgan CJ, Lowin A: A Study of Dually Diagnosed Psychiatric Inpatients: Adults With Developmental Disabilities Who Were Also Psychiatric Inpatients at State or Community Hospitals. Olympia, Wash, Washington State Department of Social and Health Services, 1989Google Scholar
14. Ballinger BB, Ballinger CB, Reid AH, et al: The psychiatric symptoms, diagnosis, and care needs of 100 mentally handicapped patients. British Journal of Psychiatry 158:251–254,1991Crossref, Medline, Google Scholar
15. Watts RV, Richold P, Berney TP: Delay in the discharge of psychiatric in-patients with learning disabilities. Psychiatric Bulletin 24:179–181,2000Crossref, Google Scholar
16. Koegl C, Durbin J, Goering P: Mental Health Services in Ontario: How Well is the Province Meeting the Needs of Persons With Serious Mental Illness? Toronto, Centre for Addiction and Mental Health, 2004Google Scholar
17. Durbin J, Cochrane J, Goering P, et al: Needs-based planning: an evaluation of a level-of-care planning model. Journal of Behavioral Health Services and Research 28:68–80,2001Crossref, Google Scholar
18. Lunsky Y, Bradley E, Durbin J, et al: Dual diagnosis in provincial psychiatric hospitals: a population based study. Toronto, Centre for Addiction and Mental Health, 2003Google Scholar
19. Ellis RJ, Wackwitz JH, Foster M: Uses of an empirically derived client typology based on level of functioning: twelve years of the CCAR. Journal of Mental Health Administration 18:88–100,1991Crossref, Medline, Google Scholar
20. Ellis R, Wilson N, Foster F. Statewide treatment outcome assessment in Colorado: the Colorado Client Assessment Record (CCAR). Community Mental Health Journal 20:72–89,1984Crossref, Medline, Google Scholar
21. Schwartz RC: Reliability and validity of the functional assessment rating scale. Psychological Reports 84:389–391,1999Crossref, Medline, Google Scholar
22. Coffman JM: Assessing the validity of the Colorado Client Assessment Record for measurement of mental health status and outcomes. Poster presented at the annual meeting of the American Public Health Association, Philadelphia, Nov 7-10, 2004Google Scholar
23. SPSS (Statistical Package for the Social Sciences). Release 11.0.1, 2001Google Scholar
24. STATA Statistics/Data Analysis. Release 6, 1999Google Scholar
25. Robertson J, Emerson E, Gregory N, et al: Lifestyle related risk factors for poor health in residential settings for people with intellectual disabilities. Research in Developmental Disabilities 21:469–486,2000Crossref, Medline, Google Scholar
26. Richards M, Maughan B, Hardy R, et al: Long-term affective disorder in people with mild learning disability. British Journal of Psychiatry 179:523–527,2001Crossref, Medline, Google Scholar
27. Jacobson JW: Do some mental disorders occur less frequently among persons with mental retardation. American Journal of Mental Retardation 94:596–602,1990Medline, Google Scholar
28. Davidson PW, Cain NN, Sloane-Reeves JE, et al: Characteristics of community-based individuals with mental retardation and aggressive behavioral disorders. American Journal on Mental Retardation 98:704–716,1994Medline, Google Scholar
29. Edelstein TM, Glenwick DS: Referral reasons for psychological services for adults with mental retardation. Research in Developmental Disabilities 18:45–59,1997Crossref, Medline, Google Scholar
30. Spence S, Stevens R, Parks R: Cognitive dysfunction in homeless adults: a systematic review. Journal of the Royal Society of Medicine 97:375–379,2004Crossref, Medline, Google Scholar
31. Bouras N, Martin G, Leese M, et al: Schizophrenia-spectrum psychoses in people with and without intellectual disability. Journal of Intellectual Disability Research 48:548–555,2004Crossref, Medline, Google Scholar
32. Moss S, Emerson E, Kiernan C, et al: Psychiatric symptoms in adults with learning disability and challenging behaviour. British Journal of Psychiatry 177:452–456,2000Crossref, Medline, Google Scholar
33. Thornicroft G, Tansella M: What Are the Arguments for Community-Based Mental Health Care? Europe: Health Evidence Network (HEN) Synthesis Report on Community Based Mental Health. Geneva, World Health Organization, 2003Google Scholar
34. Hassiotis A, Ukoumunne O, Tyrere P, et al: Prevalence and characteristics of patients with severe mental illness and borderline intellectual functioning. British Journal of Psychiatry 175:135–140,1999Crossref, Medline, Google Scholar
35. Meisler N, McKay C, Gold PB, et al: Using principles of ACT to integrate community care for people with mental retardation and mental illness. Journal of Psychiatric Practice 6:77–83,2000Crossref, Medline, Google Scholar
36. Bresch D: Problems and questions in the dual diagnosis of schizophrenia and intellectual disability. Mental Health Aspects of Developmental Disabilities 7:81–90,2004Google Scholar



