Use of Alcohol Treatment and Mental Health Services Among Adolescents With Alcohol Use Disorders
Abstract
OBJECTIVE: This study examined the use of and perceived need for alcohol treatment services among adolescents (aged 12 to 17 years) who received mental health services in the previous year compared with same-aged adolescents who did not receive such services. METHODS: Study data were drawn from the 2000 and 2001 National Household Surveys on Drug Abuse. The authors conducted logistic regression analyses to identify the characteristics associated with the receipt of and perceived need for alcohol services among adolescents with alcohol use disorders. RESULTS: Adolescents who received mental health services were much more likely than those who did not to meet criteria for alcohol use disorders in the previous year (10 percent compared with 4 percent). Among adolescents with alcohol use disorders, 15 percent of those who received mental health services used any alcohol services, compared with only 6 percent of those who did not receive mental health services. Of adolescents with alcohol use disorders who did not receive any alcohol services, only 3 percent reported a need for alcohol treatment. Among adolescents with alcohol use disorders who received mental health services, Hispanics were significantly less likely than whites to receive any alcohol services. CONCLUSIONS: These findings from a nationally representative sample of adolescents reveal a largely unrecognized and underserved population at risk. Factors related to the underutilization of alcohol services by adolescents with alcohol use disorders deserve greater research attention.
Alcohol is the most common substance used by adolescents (1), and alcohol use disorders are the most prevalent psychiatric disorders among adolescents (2). The National Comorbidity Survey (NCS) estimated that 10 percent of adolescents aged 15 to 18 years met criteria for a lifetime alcohol use disorder (3). Alcohol use disorders are highly associated with other psychiatric disorders (4). Rohde and colleagues (5) found that 82 percent of adolescents aged 14 to 18 years who had an alcohol use disorder also met criteria for at least one of several other psychiatric disorders.
Studies among adults have shown that a majority of persons with alcohol use disorders do not utilize substance abuse services (6). Although the co-occurrence of alcohol use disorders with other psychiatric disorders is associated with an increased odds of service use (6,7), the prevalence of any use of mental health or substance abuse services among adults with comorbid alcohol and other psychiatric disorders is low (6). Similarly, adolescents who participate in treatment for mental health problems have a high prevalence of substance use disorders; however, many of these substance use problems are not initially detected by clinicians (8).
Current knowledge about the use of alcohol treatment services and the perceived need for alcohol treatment is based mainly on adult samples. Research among adolescents has typically failed to discriminate between their use of substance abuse services and their use of mental health services (3,7). Adolescents with substance use disorders are less likely than those with non-addiction-related psychiatric disorders to receive substance abuse care or mental health care (7). Compared with adults, adolescents may face additional barriers to alcohol treatment. Many adolescents do not consider their substance use to be problematic (9,10). Even when adolescent substance users perceive a need for help, they may not be sure where or to whom to turn (9,11).
These studies suggest that adolescents who abuse or are dependent on alcohol are very likely to be underserved (3,6,7,8,9,10,11). Given that alcohol abuse and dependence are the most prevalent disorders among adolescents (2) and that they tend to be co-occur with other psychiatric disorders (4,5), we examined the relationship between adolescents' use of mental health services and of alcohol abuse services. Specifically, we investigated the prevalence and correlates of the use of alcohol treatment services and of perceived need for such services among adolescents with alcohol use disorders who received mental health services and compared these youths with those who did not receive such services.
Methods
Data sources
We performed statistical analyses on data from the public use files of the 2000 and 2001 National Household Surveys on Drug Abuse (NHSDA) (12,13). The NHSDA, renamed the National Survey on Drug Use and Health in 2002, is an annual survey of the use of licit and illicit substances by noninstitutionalized Americans aged 12 years or older. To generate national estimates of substance use, the survey uses multistage area probability sampling methods to select survey respondents, including residents of noninstitutional group quarters (shelters, rooming houses, dormitories, and group homes), residents of all 50 states, and civilians residing on military bases.
Respondents were interviewed at their place of residence for about an hour. For adolescents aged 12 to 17 years, the field interviewer first obtained oral consent from a parent or guardian. Once parental permission was granted, the interviewer approached the adolescent and introduced the study by using the script to obtain the youth's agreement to participate. Parents were then asked to leave the interview setting to ensure the confidentiality of the youth's responses.
To increase their willingness to report substance use behaviors honestly, the survey used a combination of computer-assisted personal interviewing and audio computer-assisted self-interviewing methods. The latter method was used for sensitive survey items, for which respondents either read the questions silently on a computer screen or listened to the questions read aloud by the computer through headphones and then entered their responses directly into the computer.
In 2000-2001, approximately 70,000 persons aged 12 years or older participated in each of the annual surveys. Weighted interview response rates were 73 to 74 percent and were consistently higher among adolescents (aged 12 to 17 years) than among adults (14). To ensure that each independent cross-sectional NHSDA sample was representative of the U.S. general population aged 12 or older, analysis weights were developed to adjust for variation in household selection, nonresponse, and poststratification of the selected sample to census. The NHSDA designs are reported in detail elsewhere (12,13). The survey was approved by the institutional review board of Research Triangle Institute.
Study sample
This study focused on adolescents aged 12 to 17 years. We found little yearly differences in the distribution of age, gender, race or ethnicity, or family income across the two survey years. In this combined sample (N=36,859), 49 percent were female, 35 percent were members of nonwhite minority groups, and 43 percent reported an annual family income of $40,000 or less.
Study variables
Use of mental health services included the receipt of any treatment or counseling at any service location in the previous year for emotional or behavioral problems that were not related to alcohol or drug use (15). Treatment service locations included hospitals, private physicians' offices, mental health clinics or programs, general medical settings, and schools.
Our dependent variable was any use of treatment services for alcohol-related problems at any location in the previous year (16). A specialty setting referred to the receipt of inpatient alcohol treatment at hospitals or of any alcohol services at a residential alcohol or drug rehabilitation or mental health facility. The subsample of respondents who reported that they did not receive services for their alcohol use in the previous year were then asked whether they thought they needed alcohol-related treatment or counseling during that period. A positive response to this question indicated the perceived need for alcohol treatment services (16).
Past-year alcohol and drug use disorders were assessed by using DSM-IV criteria (15,16,17,18). Any drug abuse included abuse of any of the following drugs in the previous year: cocaine or crack, marijuana or hashish, heroin, hallucinogens, inhalants, sedatives, tranquilizers, pain relievers, and stimulants. Similarly, any drug dependence referred to drug dependence on any of these drugs in the previous year. The number of drug use disorders in the previous year was summed and grouped into four categories (none, one, two, and three or more classes of drugs).
We examined the following demographic characteristics of respondents: age, gender, race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian or Pacific Islander, American Indian or Alaska Native, and more than one race), total family income, and population density of the area in which the respondent lived (15,16,17).
Data analysis
Because of the use of multistage probability sampling methods, data were weighted to adjust for variations in household selection and nonresponse and to reflect the representativeness of the NHSDA sample. We used SUDAAN software (19), which applies a Taylor series linearization method to account for the effects of the complex multistage NHSDA design features. All percentages reported in this article are weighted estimates, and sample sizes are unweighted.
We first examined the prevalence of mental health service use in relation to alcohol use disorders. In the subsample of adolescents who met the criteria for alcohol use disorders, we then compared the prevalence of their alcohol service use and of their perceived need for such services by their use of mental health services. Finally, we conducted logistic regression procedures to identify the characteristics associated with alcohol service use and with the perceived need for such services.
Results
Mental health service use
Among all adolescents aged 12 to 17 years in the two survey years (N=36,859), 16 percent (N=6,111) used mental health services for emotional or behavioral problems not related to substance use in the previous year. Of these mental health service users, 12 percent received inpatient mental health services and 61 percent received outpatient mental health services. The remaining users received mental health services at school. Reasons for receiving mental health services included depression (38 percent), acting out (17 percent), suicidal ideation or suicide attempt (14 percent), anxiety (11 percent), eating problems (6 percent), and other emotional or behavioral problems. Table 1 shows that girls, American Indians and Alaska Natives, adolescents who reported more than one race, adolescents who reported the lowest level of family income, and adolescents who were living in large metropolitan areas were slightly more likely to receive mental health services than boys, Asians or Pacific Islanders, Hispanics, those reporting a higher level of income, and those residing in nonmetropolitan areas. Use of mental health services also was highly associated with alcohol and drug use disorders.
Alcohol use disorders
Adolescents who received mental health services were more likely than those who did not to meet the criteria for alcohol use disorders. Prevalence rates of alcohol use disorders among adolescents who used mental health services were 6 percent for abuse and 4 percent for dependence, respectively. The corresponding prevalence rates among those who did not use mental health services were 3 percent (χ2=57.51, df=1, p<.001) and 2 percent (χ2=57.01, df=1, p<.001), respectively. We then compared the co-occurrence of alcohol and drug use disorders. Users of mental health services were more likely than nonusers to meet criteria for both alcohol and drug use disorders. Of all adolescents with alcohol use disorders, 51 percent of mental health service users also had drug use disorders, compared with 33 percent of nonusers of mental health services (χ2=34.42, df=1, p<.001).
Alcohol service use
Past-year use of alcohol services by past-year use of mental health services is shown in Table 2. Among alcohol abusers, mental health service users were more likely than nonusers to receive any alcohol service (13 percent compared with 6 percent) but did not differ from nonusers in their use of specialty alcohol treatment. Among adolescents with alcohol dependence, mental health service users were more likely than nonusers to receive any alcohol service (20 percent compared with 7 percent) and to receive specialty alcohol treatment (12 percent compared with 4 percent).
Because of the high prevalence of comorbid alcohol and drug use disorders among these adolescents, we also explored their use of drug abuse services. The prevalence of past-year use of drug abuse services was very similar to our estimate of alcohol services. Among adolescents with an alcohol use disorder, 9 percent used any drug abuse services and 4 percent used such services at a specialty setting. Overall, only 13 percent of adolescents with alcohol use disorders reported any service use for their alcohol or drug problems. Approximately 64 percent of service users received services for both alcohol and drug problems, and the remaining users received services for either alcohol problems (20 percent) or drug problems (17 percent).
Perceived need for alcohol treatment
Of the subsample of adolescents with alcohol use disorders who reported no use of any alcohol services in the previous year, very few reported needing alcohol services (Table 2). Mental health service users were equally as unlikely as nonusers to report that they perceived any need for alcohol treatment (5 percent compared with 5 percent among those with alcohol dependence and 1 percent compared with 2 percent among those with alcohol abuse).
Logistic regression of any alcohol treatment services
The results of our logistic regression of any past-year use of alcohol services among adolescents with alcohol use disorders are shown in Table 3. We found little variation in the characteristics that discriminated between the use of alcohol services by adolescents with alcohol use disorders who did and who did not use mental health services. Among those who used mental health services, Hispanic adolescents were less likely than whites to receive any alcohol service (adjusted OR=.3, 95 percent confidence interval [CI]=.1 to .8).
Age group, gender, family income, population density, and alcohol use diagnosis (abuse versus dependence) were all unassociated with the receipt of any alcohol treatment service. Among nonusers of mental health services, family income was associated with the use of alcohol treatment services. Adolescents who reported a family income between $20,000 and $39,999 were slightly more likely than those who reported a family income of $75,000 or more to use any alcohol treatment services (adjusted OR=2.3, CI=1.1 to 4.8). Regardless of use of mental health services, having more than one drug use disorder was associated with an increased odds of using any alcohol service.
Logistic regression of specialty alcohol treatment services
We then determined whether the correlates of using specialty alcohol treatment among adolescents with alcohol use disorders differed by use of mental health services (Table 4). Logistic regression indicated no significant differences in the use of specialty treatment by age group, gender, race or ethnicity, family income, population density, and alcohol use diagnosis. Regardless of mental health service use, the receipt of specialty alcohol treatment was highly associated with comorbid drug use disorders. Compared with adolescents without comorbid drug use disorders, adolescents who abused or were dependent on alcohol and had two comorbid drug use disorders were five times as likely to receive specialty alcohol treatment if they also used mental health services and were ten times as likely to receive such treatment if they did no use mental health services.
Logistic regression of perceived need for treatment
We then examined the perceived need for alcohol treatment among adolescents with alcohol use disorders who did not use any alcohol service in the previous year (Table 5). We found that age group, population density, and severity of alcohol use were all associated with perceived need for alcohol treatment among mental health service users, but none of them was significant among nonusers of mental health services. Adolescents aged 12 or 13 years who had alcohol use disorders were six times as likely as older adolescents (aged 16 or 17 years) to report needing alcohol treatment. Adolescents who lived in metropolitan areas, compared with those in nonmetropolitan areas, and those who had alcohol dependence, compared with those who had alcohol abuse, were more likely to report needing alcohol treatment.
In contrast, the co-occurrence of multiple drug use disorders was strongly associated with the perceived need for alcohol treatment, regardless of use of mental health services. Compared with adolescents who did not have comorbid drug use disorders, those with two comorbid drug use disorders were eight times as likely to use alcohol treatment services if they also used mental health services and ten times as likely to report needing alcohol treatment.
Discussion and conclusions
We found that 5 percent of adolescents aged 12 to 17 years met criteria for past-year alcohol use disorders. The National Survey of Adolescents also reported that 4 percent of adolescents aged 12 to 17 years met criteria for past-year alcohol use disorders (20). Consistent with the findings of other studies (8,21), we found that adolescents who received mental health services had a higher prevalence of substance use disorders than those who did not receive such services.
The most salient finding of this study is the very low prevalence of adolescents with alcohol use disorders who neither used alcohol services nor perceived a need for such services. Only 9 percent of adolescents with alcohol use disorders received any alcohol-related services, and only 5 percent received specialty alcohol services. Even when the use of drug abuse services was included, 13 percent of adolescents who abused or were dependent on alcohol received any alcohol or drug abuse services.
Of the adolescents who had alcohol use disorders and who did not receive any alcohol treatment service, only 2 percent of mental health service users and 3 percent of nonusers reported a need for alcohol treatment.
Our prevalence estimate of any use of alcohol services among adolescents who were dependent on alcohol (11 percent) is close to the estimate for adults who are dependent on alcohol (12 percent) (16). The National Longitudinal Alcohol Epidemiologic Survey also estimated that 10 percent of adults with alcohol use disorders received alcohol treatment services in the previous year (22). Yet our prevalence estimate of perceived needs for alcohol treatment among adolescents who were dependent on alcohol (5 percent) is much lower than the estimate for adults (8 to 10 percent) (16).
As with other studies (9), we found that adolescents who received mental health services were more likely than those who did not to use any alcohol treatment services and to receive such services in a specialty setting. Kramer and colleagues (8) found that, among adolescents who were seeking treatment for mental health problems, adolescents whose substance use problems were detected by clinicians at their initial assessments were much more likely than those whose substance use problems were undetected to receive specialty addiction care. Our findings and those of others highlight the importance of a thorough screening for comorbid substance abuse and mental health problems among adolescents seeking mental health services (8,9).
The low prevalence of use of alcohol treatment services appears to be related to the following factors. First, a majority of individuals with alcohol use disorders do not perceive the need for substance abuse services (23). They typically do not consider their drinking to be a problem, or they prefer to handle it on their own (10,24,25). There is generally a long lag time between the onset of an alcohol problem and contact with a health care provider (26), and many individuals who abuse or are dependent on alcohol do not seek treatment until their alcohol use generates substantial problems in their lives (27).
Second, adolescents with an alcohol use disorder may not be sure where to turn for help (9,11). Their access to and use of alcohol treatment services may depend in part on their parents' or other adults' recognition of alcohol problems and a need for treatment (28). In this study, a majority of service users received treatment or counseling for both alcohol and drug problems, which is consistent with our findings that the presence of more than one drug use disorder is the primary determinant of use of alcohol treatment services and the perceived need for such services (16,29). It seems likely that the illicit nature of drug abuse behaviors brings adolescents to the attention of the criminal justice system, which in turn precipitates their entry into substance abuse services (30). Adolescents with comorbid alcohol and drug use disorders also tend to run afoul of their schools, families, peers, and employers, which prompts others to identify them as needing help.
Third, adolescents with alcohol use disorders tend to have other psychiatric problems (5). Parents and other caregivers may interpret the adolescents' alcohol use as a psychological problem and seek services that address that issue. Adolescents with substance abuse who also have mental health problems may use mental health services that are not designed specifically for addressing substance use problems (9). Yet many adolescent substance abusers who are in mental health treatment are not identified early by clinicians as having substance use problems and do not receive appropriate substance abuse services (8). Finally, stigma, cost of treatment, lack of knowledge about treatment programs and options, costs related to time and transportation, and negative attitudes toward alcohol treatment are other potential barriers to adolescents' use of alcohol treatment services (24,25,31).
The results of our study suggest the need to educate the public about the symptoms of alcohol use disorders, their consequences, and the availability of treatment services (16). For example, the use of media campaigns in educating the public about depression has generated significant positive changes in public attitudes toward depression and its treatment (32). Among adolescents who have alcohol use disorders, the receipt of mental health services is not associated with their perceived needs for alcohol treatment, which suggests that adolescents may consider alcohol and mental health problems as two different conditions and that alcohol-related problems tend to be viewed as transient phenomena.
These findings should be interpreted with some caution. First, the NHSDA uses a cross-sectional design and relies on respondents' self-reports. Although we focused on alcohol use problems and service use that occurred within the 12 months before the interview, our findings could have been influenced by both memory errors and underreporting biases (33). On the other hand, the NHSDA has incorporated computer-assisted interviewing techniques to improve the accuracy of self-reports of substance use behaviors (34). Second, the lack of data on the quality of service obtained limited the breadth of our analyses. Third, our distinction between alcohol services and drug abuse services was based on adolescent self-reports, which may be influenced by adolescents' perceptions of their substance use behaviors and could be different from the view of service providers. Nevertheless, we found that about 84 percent of adolescents who abused or were dependent on alcohol and who received alcohol or drug treatment services reported the receipt of services for alcohol problems (64 percent for both alcohol and drug problems and 20 percent for alcohol problems only) and that 17 percent reported the receipt of services for drug problems only.
It appears that only adolescents with the most severe alcohol problems come to the attention of adults, who then facilitate their entry into treatment (35). Overall, 91 percent of adolescents who had recent alcohol use disorders did not receive any alcohol services in the previous year and, of those who received no such services, 97 percent did not perceive the need for alcohol treatment. Underuse of alcohol services is widespread across all demographic groups. Hispanic youths and those without co-occurring drug use disorders may be less likely to be identified by others as having alcohol problems that require help. Untreated alcohol use disorders are highly costly to affected families and to society. More studies are recommended to specify the factors that impede the identification of alcohol problems and access to alcohol services.
Dr. Wu is affiliated with the department of psychiatry and behavioral sciences of the Duke University in Durham, North Carolina. Dr. Ringwalt is with the Chapel Hill Center of the Pacific Institute for Research and Evaluation in North Carolina. Send correspondence to Dr. Wu at Duke University Medical Center, Duke Clinical Research Institute, P.O. Box 17969, Durham, North Carolina 27715 (e-mail, [email protected]).
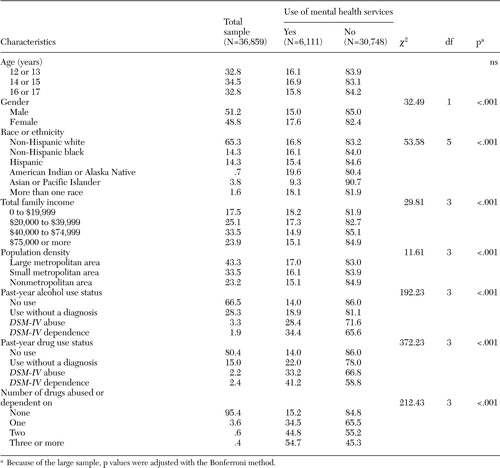 |
Table 1. Demographic and substance use characteristics of adolescents in a study of use of mental health and alcohol treatment services, expressed as weighted percentages
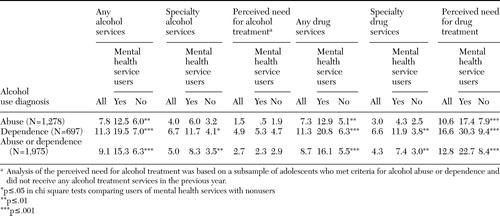 |
Table 2. Past-year prevalence of use of alcohol treatment services and of perceived need for such services among adolescents (aged 12 to 17), by past-year alcohol use diagnosis and use of mental health services, expressed as weighted percentages
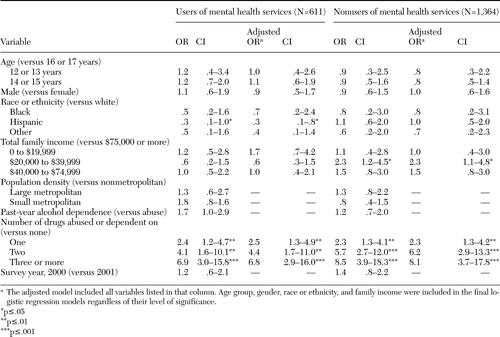 |
Table 3. Odds ratios, adjusted ORs, and 95 percent confidence intervals for any use of alcohol treatment services among adolescents who met criteria for alcohol abuse or dependence
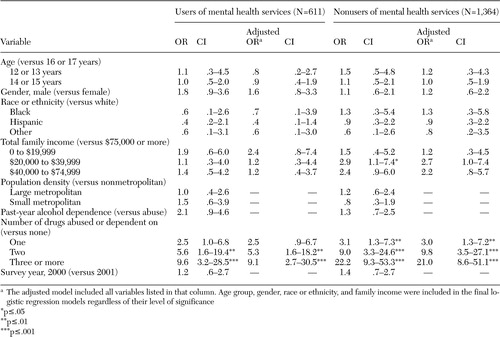 |
Table 4. Odds ratios and 95 percent confidence intervals for use of specialty alcohol treatment service among adolescents who met criteria for alcohol abuse or dependence
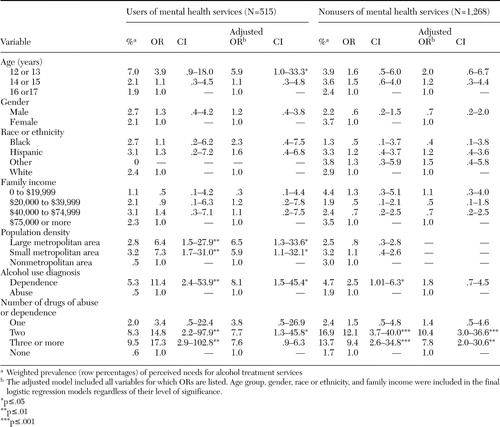 |
Table 5. Odds ratios and 95 percent confidence intervals for perceived need for alcohol treatment services among adolescents with alcohol abuse or dependence who did not receive any alcohol treatment service
1. Results From the 2002 National Survey on Drug Use and Health: National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2003Google Scholar
2. Reinherz HZ, Giaconia RM, Lefkowitz ES, et al: Prevalence of psychiatric disorders in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 32:369–377,1993Crossref, Medline, Google Scholar
3. Warner LA, Canino G, Colon HM: Prevalence and correlates of substance use disorders among older adolescents in Puerto Rico and the United States: a cross-cultural comparison. Drug and Alcohol Dependence 63:229–243,2001Crossref, Medline, Google Scholar
4. Kessler RC, Crum RM, Warner LA, et al: Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry 54:313–321,1997Crossref, Medline, Google Scholar
5. Rohde P, Lewinsohn PM, Seeley JR: Psychiatric comorbidity with problematic alcohol use in high school students. Journal of the American Academy of Child and Adolescent Psychiatry 35:101–109,1996Crossref, Medline, Google Scholar
6. Wu LT, Kouzis AC, Leaf PJ: Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. American Journal of Psychiatry 156:1230–1236,1999Abstract, Google Scholar
7. Garland AF, Aarons GA, Brown SA, et al: Diagnostic profiles associated with use of mental health and substance abuse services among high-risk youths. Psychiatric Services 54:562–564,2003Link, Google Scholar
8. Kramer TL, Robbins JM, Phillips SD, et al: Detection and outcomes of substance use disorders in adolescents seeking mental health treatment. Journal of the American Academy of Child and Adolescent Psychiatry 42:1318–1326,2003Crossref, Medline, Google Scholar
9. Johnson SD, Stiffman A, Hadley-Ives E, et al: An analysis of stressors and co-morbid mental health problems that contribute to youth's paths to substance-specific services. Journal of Behavioral Health Services and Research 28:412–426,2001Crossref, Medline, Google Scholar
10. McLennan JD, Shaw E, Shema SJ, et al: Adolescents' insight in heavy drinking. Journal of Adolescent Health 22:409–416,1998Crossref, Medline, Google Scholar
11. Klein JD, McNulty M, Flatau CN: Adolescents' access to care: teenagers' self-reported use of services and perceived access to confidential care. Archives of Pediatrics and Adolescent Medicine 152:676–682,1998Crossref, Medline, Google Scholar
12. Summary of Findings From the 2000 National Household Survey on Drug Abuse. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2001Google Scholar
13. Results From the 2001 National Household Survey on Drug Abuse: Vol I. Summary of National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2002Google Scholar
14. Results From the 2001 National Household Survey on Drug Abuse: Vol II Technical Appendices and Selected Data Tables. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2002Google Scholar
15. Wu LT, Pilowsky DJ, Schlenger WE: Inhalant abuse and dependence among adolescents in the United States. Journal of the American Academy of Child and Adolescent Psychiatry 43:1206–1214,2004Crossref, Medline, Google Scholar
16. Wu LT, Ringwalt CL: Alcohol dependence and treatment service utilization among community women. American Journal of Psychiatry 161:1790–1797,2004Link, Google Scholar
17. Wu LT, Pilowsky DJ, Schlenger WE: High prevalence of substance use disorders among adolescents who used marijuana and inhalants. Drug and Alcohol Dependence 78:23–32,2005Crossref, Medline, Google Scholar
18. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
19. SUDAAN User's Manual: Release 8.0. Research Triangle Park, NC, Research Triangle Institute, 2002Google Scholar
20. Kilpatrick DG, Acierno R, Saunders B, et al: Risk factors for adolescent substance abuse and dependence: data from a national sample. Journal of Consulting and Clinical Psychology 68:19–30,2000Crossref, Medline, Google Scholar
21. King RD, Gaines LS, Lambert EW, et al: The co-occurrence of psychiatric and substance use diagnoses in adolescents in different service systems: frequency, recognition, cost, and outcomes. Journal of Behavioral Health Services and Research 27:417–430,2000Crossref, Medline, Google Scholar
22. Grant BF: The influence of comorbid major depression and substance use disorders on alcohol and drug treatment: results of a national survey. NIDA Research Monograph 172:4–15,1997Medline, Google Scholar
23. Mojtabai R, Olfson M, Mechanic D: Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry 59:77–84,2002Crossref, Medline, Google Scholar
24. Cunningham JA, Sobell LC, Sobell MB, et al: Barriers to treatment: why alcohol and drug abusers delay or never seek treatment. Addictive Behaviors 18:347–353,1993Crossref, Medline, Google Scholar
25. Grant BF: Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. Journal of Studies on Alcohol 58:365–371,1997Crossref, Medline, Google Scholar
26. Kessler RC, Aguilar-Gaxiola S, Berglund PA, et al: Patterns and predictors of treatment seeking after onset of a substance use disorder. Archives of General Psychiatry 58:1065–1071,2001Crossref, Medline, Google Scholar
27. Bucholz KK, Homan SM, Helzer JE: When do alcoholics first discuss drinking problems? Journal of Studies on Alcohol 53:582–899,1992Google Scholar
28. Poduska JM: Parents' perceptions of their first graders' need for mental health and educational services. Journal of the American Academy of Child and Adolescent Psychiatry 39:584–591,2000Crossref, Medline, Google Scholar
29. Wu LT, Ringwalt CL, Williams CE: Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatric Services 54:363–369,2003Link, Google Scholar
30. Grella CE, Hser YI, Joshi V, et al: Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. Journal of Nervous and Mental Disease 189:384–392,2001Crossref, Medline, Google Scholar
31. Sturm R, Sherbourne CD: Are barriers to mental health and substance abuse care still rising? Journal of Behavioral Health Services and Research 28:81–88,2001Google Scholar
32. Paykel ES, Hart D, Priest RG: Changes in public attitudes to depression during the Defeat Depression Campaign. British Journal of Psychiatry 173:519–522,1998Crossref, Medline, Google Scholar
33. Colon HM, Robles RR, Sahai H: The validity of drug use self-reports among hard core drug users in a household survey in Puerto Rico: comparison of survey responses of cocaine and heroin use with hair tests. Drug and Alcohol Dependence 67:269–279,2002Crossref, Medline, Google Scholar
34. Wright DL, Aquilino WS, Supple AJ: A comparison of computer-assisted paper-and-pencil self-administered questionnaires in a survey on smoking, alcohol, and drug use. Public Opinion Quarterly 62:331–353,1998Crossref, Google Scholar
35. Grella CE, Joshi V: Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. American Journal of Drug and Alcohol Abuse 25:385–406,1999Crossref, Medline, Google Scholar



