The Pathway to Meeting Need for Mental Health Services in Sweden
Abstract
OBJECTIVE: Mental health problems are often underrecognized and undertreated. Knowledge of the characteristics associated with the pathway to having a need for mental health care by appropriate treatment (met need) can help to correct this deficit. This study used data from a population-based study to determine the characteristics of persons whose needs were meetable, who were aware of the need for mental health care, who requested care, and whose needs were met. METHODS: A total of 10,443 randomly selected persons in Stockholm, Sweden, aged 20 to 64 years answered a survey that included questions about mental health problems. A subsample of 1,093 persons was then interviewed by psychiatrists, who determined whether the respondents had a psychiatric disorder according to DSM-IV criteria. The interview also assessed need for care, service use, and whether an evidence-based treatment was available for the mental health problem. RESULTS: Among the 1,093 persons interviewed 462 were found to have a mental health problem for which psychiatric treatment was available (meetable need for care). Among the 462 persons with a meetable need for care, 70 percent fulfilled the DSM-IV diagnostic criteria for having a psychiatric disorder; the rest had various symptoms, mostly depressive. Among the persons with a meetable need for care, 84 percent were aware of this need, 37 percent had requested care, and 17 percent had their needs met by evidence-based treatment. Persons whose needs were met tended to be female, have more education, and have good social support. Also, they were less likely to report that feelings of shame would prevent them from requesting psychiatric care. CONCLUSIONS: The characteristics associated with unmet need suggest that strategies that focus on specific groups (for example, males and persons with less education) could increase the percentage of persons whose needs are met.
Mental health problems are one of the leading causes of illness and disability worldwide (1). Although effective solutions for mental disorders are available, only 20 to 30 percent of the people identified in epidemiologic surveys as having a mental disorder had their needs for care met (2,3,4,5,6). Most of these studies defined need as being present if a person fulfilled the criteria for having a psychiatric disorder (ICD-10 or DSM-IV) and defined the need as being met if the person had seen a health professional.
To increase the proportion of persons whose needs are met is important, because untreated psychiatric disorders often have poor outcomes. Resources are sparse, and knowledge is needed in order to direct resources efficiently. One way to increase this knowledge is to analyze the pathway to met need to see which characteristics correspond with unmet need. Knowing which characteristics are involved could help to determine at which level interventions should be made. For example, an association between financial difficulties and unmet need would indicate that the general health insurance system in Sweden needs to be improved. And an association between co-occurring somatic disorders and unmet need would indicate the need for medical personnel to increase the awareness of mental health problems. Another way to reach people is with public awareness campaigns—for example, the Defeat Depression Campaign run by the Royal College of Psychiatrists and the Royal College of General Practitioners from 1992 to 1996 in the United Kingdom (7,8). Knowing which groups of persons have unmet need would be important when designing such campaigns—for example, whether to focus on educational level, type of psychiatric disorder, country of origin, or attitudes toward mental illness.
Some studies have stated that having a psychiatric disorder does not necessarily mean that mental health care is needed—the overall course of symptom development and the level of functioning are important in determining need (4,9,10,11). Additionally, having seen a mental health professional is not always the same as having needs met (12,13). One way to overcome this discrepancy is to use a structured interview to assess the need for care and met needs. The pathway to met need is a complex process, in which the individual first must identify the need for care (14). The ability to identify whether care is needed may be influenced by negative attitudes linked to psychiatric problems (15,16,17). If a person identifies a need for help, the next step is to decide what type of help he or she would like and where to turn. Some obstacles could prevent a person from receiving care, such as preferring care that is unavailable or available only at a cost that is too high. Additionally, professionals and people needing care may disagree about which type of care is suitable.
This study examined data from a population-based study to determine which characteristics were associated with having needs met for mental health care. Needs were said to have been met if the person received evidence-based treatment. This study analyzed the pathway to met need according to a model based on the work of Goldberg and Huxley (18). The first step in the model is awareness of need; the second, request for care; and the third, having needs met. This study then defined the characteristics associated with each step in order to provide information that could be used to create intervention strategies at each step.
Methods
Data were from a longitudinal population-based study on mental health, the PART study (Psykisk hälsa, Arbete och RelaTioner, or Mental Health, Work, and Relations). A description of the study is available on the Internet (19). From 1998 to 2000, a total of 19,744 persons aged 20 to 64 years who were registered in the county of Stockholm, Sweden, were randomly selected to receive the survey by mail. A total of 10,443 persons answered the survey (53 percent). Informed consent was obtained from participants, and the study was approved by the ethical committee at Karolinska Institutet in Stockholm.
The survey was extensive. The first part included questions about the country of origin, family conditions during childhood, education, financial situation, occupation, coping strategies, social support, life events, drug use, and somatic disorders. The second part was composed of scales on psychological well-being and psychiatric symptoms.
According to study criteria, respondents were said to have anxiety disorder if they had at least six symptoms of anxiety or panic attacks and if they were afraid that the anxiety or panic attacks would return (Sheehan Patient-Rated [Panic] Anxiety Scale) (20), if they had at least one avoidance of agoraphobic or social phobic situations caused by fear or anxiety (instrument developed by Marks and Matthews) (21), or if they experienced at least one obsessive-compulsive symptom and suffered as a result (Yale-Brown Obsessive-Compulsive Scale) (22). Respondents were said to have depression if they had at least five symptoms of depression for more than two weeks and disability that resulted from the depression (Major Depression Inventory) (23). Persons were said to have a substance use disorder if they scored at least 11 on the Alcohol Use Disorders Identification Test (24) or if they had used illicit drugs in the past month. Persons were also said to have a mental health problem if they had at least one symptom of eating disturbance (scale developed by Beglin and Fairburn) (25) or at least one symptom of social disability caused by psychological problems (World Health Organization [WHO] Short Disability Assessment Schedule) (26). The survey did not include questions about psychotic symptoms. Among persons who responded to the questionnaire, 3,521 persons (34 percent) were found to have a mental health problem, according to the survey criteria.
Respondents versus nonrespondents
Lundberg and colleagues (27) performed an extensive analysis using available official registers to compare persons who responded to the survey (N=10,443) and those who did not (N=9,301). Persons were more likely to respond if they were female, were older, had a higher income and education, were born in a Nordic country, and had no psychiatric diagnosis in the hospital discharge register or in the early retirement register. The associations between age, gender, income, country of origin, and inpatient hospital care as a result of mental problems were calculated for respondents and nonrespondents separately. Odds ratios were calculated and no significant differences were found between respondents and nonrespondents (27).
Interviews
Among the respondents, random samples of persons with and persons without mental problems were invited to the psychiatric interview. Altogether 1,093 participants were interviewed: 884 who screened positive (25 percent of all respondents who screened positive, 60 percent of whom were women) and 209 who screened negative (3 percent of all respondents who screened negative, 49 percent of whom were women). The same data from official registers that were used for the attrition analysis for response to the questionnaire were used in an analysis for participation in the psychiatric interview (27). No statistically significant differences were found between respondents who were interviewed and those who were not.
The professional interviewers used the Schedules for Clinical Assessment in Neuropsychiatry (28) and a slightly modified version of the MRC Needs for Care Assessment (29,30). The MRC Needs for Care Assessment included questions on utilization (number and type of contacts with the health care system, when these contacts occurred, and the type of treatment received) and awareness of need (judgment concerning need of care). The assessment also determined whether meetable need for care was met. Needs were said to be meetable if a psychiatric treatment was available. Needs were said to have been met if the person received evidence-based treatment; other types of treatment were not included in our analysis. Evidence-based treatment was defined according to recommendations by Sweden's National Board of Health and Welfare. An open-ended question concerning what might prevent a person from requesting care was administered. The interviewers had a one-week introductory course by one of the WHO designated trainers on how to administer the Schedules for Clinical Assessment in Neuropsychiatry interview and the Short Disability Assessment Schedule. The training consisted of videotaped interviews that were rated by the interviewers and discussions after the rating. During the interviews this procedure was repeated once every other week by using videotapes of performed interviews. The interviewers were blind to the participants' answers to the questionnaire. At the interview, psychiatric diagnoses were made according to DSM-IV criteria (31).
Characteristics analyzed in the model
The model examined demographic characteristics (age, gender, and whether the person was born in Sweden or another country) and social characteristics (whether the persons lived with someone and whether the person had high or low social support, according to a scale developed by Undén and Orth-Gomer) (32). Financial status was described by using occupational status (employed or unemployed), the number of years of education (nine years or less and ten years or more), and the presence of financial difficulties (whether the person was unable to attain 14,000 Swedish Kronor [$1,800 U.S.] within a week, if necessary). Psychiatric diagnoses were categorized as depressive disorders, anxiety disorders, alcohol use disorders, multiple diagnoses, and other diagnoses according to DSM-IV criteria. Additionally, there was a group that did not fulfill DSM-IV criteria for a diagnosis but still had a meetable need for care. Somatic disorders were considered to be present if the disorder required treatment by a physician or hospital care.
The most common answer for not seeking care was feelings of shame. Therefore, reasons for not seeking care were categorized into three groups: feelings of shame, other reasons, and no reasons. Other reasons included financial difficulties, negative perception of psychiatric care, and the view that all persons ought to resolve the problem themselves. Selecting "no reasons" indicated that the persons would ask for care without hesitating, if they felt that they needed it.
Statistical analyses
Statistical analyses were carried out with SPSS version 10.0 for Mac OSX (33). In order to study differences between persons who reached different stages in the pathway to care, chi square tests and t tests were used with a significance level set at .05. Persons who reached the previous step in the pathway to met need made up the reference group, and persons with met need were also compared with all persons with meetable need. Because characteristics might have been interrelated, hierarchical logistic regression analyses were performed by using persons who reached the previous step in the pathway to met need as the reference group. A separate analysis was performed that compared persons whose needs were met with all persons with meetable need.
Results
Study population
Among the 1,093 persons interviewed, 462 (42 percent) were identified as having a meetable need for care and were included in our study sample. All 462 were considered to have a mental health problem because they scored positive on at least one of the screening scales in the questionnaire. Their mental health problems needed treatment according to the MRC Needs for Care Assessment, and a practical treatment was available for these problems. Table 1 compares the characteristics of interviewees who were identified as having a meetable need for care (N=462) and the rest of the sample that responded to the survey (N=9,981). Compared with the rest of the sample that responded to the survey, persons who were interviewed and identified as having a meetable need for care tended to be unemployed, have less education, be single, have financial difficulties more often, and have low social support. Among the interviewees who were identified as having meetable need, 322 (70 percent) fulfilled the DSM-IV diagnostic criteria for having a psychiatric disorder, most commonly a depressive disorder. The remaining 140 did not meet DSM-IV criteria, although most had depressive symptoms.
Among the 462 persons with a meetable need for care, 388 (84 percent) had awareness of this need. Persons who were aware of their need for care tended to be female, to have been born in Sweden, and to not have an alcohol use disorder (Table 2). Multivariate analyses showed that alcohol use disorder was negatively associated with being aware of the need for care (odds ratio [OR]=.3, 95 percent confidence interval [CI]=.1 to .6), whereas female gender was positively associated (OR=2.1, CI=1.2 to 3.6).
Among the 388 respondents with a meetable need for care and awareness of need, 172 (44 percent) had requested care for a mental health problem. Among those who requested care, 98 (57 percent) had gone to some sort of specialist (psychiatrist or psychologist), and 74 (43 percent) had received another type of care, mostly from a general practitioner. As shown in Table 3, persons who requested care tended to be female, older, unemployed, more educated, and born in a country other than Sweden. They also tended to have multiple psychiatric diagnoses and less feelings of shame about mental health problems. Multivariate analyses showed that being born in another country (OR=3.1, CI=1.4 to 6.7), being female (OR=2.2, CI=1.4 to 3.5), having more education (OR=2.4, CI=1.4 to 3.9), and having multiple diagnoses (OR=2.1, CI=1.1 to 4.0) were all positively correlated with requesting care. Other diagnoses (OR=.2, CI=0 to .8) and feelings of shame (OR=.6, CI=.4 to .9) were negatively correlated.
Among the 172 persons who had requested care, 80 (47 percent) were considered to have had their needs met. Among the 98 persons who had gone to a specialist, 59 (60 percent) had their needs met. Among the 74 who had received another type of care, 20 persons (27 percent) had their needs met (χ2=19.5, df=1, p<.001). Persons whose needs were met tended to have good social support and had somatic disorders less often (Table 4). Both associations remained after multivariate analysis was performed (OR=3.4, CI=1.2 to 9.8) and (OR=.4, CI=.2 to .9), respectively.
We also compared the group whose needs were met (N=80) with the group with meetable need (N=462). Persons whose needs were met tended to be female (χ2=6.5, df=1, p<.01), have more education (χ2=7.0, df=1, p<.008), have good social support (χ2=5.2, df=1, p<.02), and have fewer feelings of shame (χ2=4.3, df=1, p<.03). These associations were also found after logistic regression analysis—female (OR=2.1, CI=1.2 to 3.7), more education (OR=2.5, CI=1.4 to 4.6), good social support (OR=3.3, CI=1.3 to 8.4), and fewer feelings of shame (OR=.5, CI=.3 to .9).
Discussion
Less than a quarter of the persons who were identified as having meetable need for care as a result of mental health problems had their needs met. This finding is in agreement with previous studies reporting that a majority of people with mental health problems have unmet need (2,3,4,5,6). One-third of the persons with meetable need did not fulfill the criteria for having a psychiatric disorder according to DSM-IV criteria. This finding has been reported in previous studies and supports the idea that other criteria are needed to study meetable need (4,9,10,11). Additionally, having seen a health professional was not an adequate measure for met need—which has also been seen in studies that examined primary care populations (12,13)—because less than half the persons in our study who requested care had their needs met.
Most participants (84 percent) who had a meetable need for care were aware of this need. One important exception was persons with an alcohol use disorder, indicating that this group tended to deny having a problem. Despite the high rate of awareness of need, only 37 percent of those who had a meetable need requested care. Persons tended to request care if they were female, were unemployed, and had more education. These correlations have also been reported in previous studies (34). One explanation is that many persons lack knowledge about recent advances in available treatments. Generally, females tend to discuss problems with their social network and as a result are more likely to be well informed about available therapies. Also, persons with higher education are experienced in seeking information.
Persons who had not requested care tended to report that feelings of shame stopped them from seeking care. In the group that had requested care, persons with low social support and a somatic disorder had their needs met less often. Coexistence of a somatic disorder may have made treatment more complicated but also increased the possibility that the psychiatric symptoms might have been seen as a part of the somatic disorder. Unmet need was less common in the group that had seen a specialist than in the group that received another type of treatment, indicating that primary care providers need training so they can provide the appropriate service for persons with mental health problems. Not only is diagnostic knowledge important, but the overall course of symptom development and the level of functioning are also important factors. The MRC Needs for Care Assessment is a step in this direction and can be further developed for primary care use.
The nonresponse rate in this study was high, which may have affected the results. Nonresponse was higher among persons who were born in other countries, were younger, were male, had lower income, and were previously hospitalized for psychiatric disorders. However, the associations between age, gender, income, country of origin, sick leave, and inpatient hospital care as a result of psychiatric diagnosis were similar among respondents and nonrespondents (27). This finding indicates that our sample corresponds to the general population in Sweden, despite the high nonresponse rate. The strength of the study is that data were taken from a population and clinically experienced psychiatrists performed the interviews.
Conclusions
To increase the proportion of persons whose needs for mental health care are met, strategies are required at different levels. Information to the public ought to be focused on groups that tend to have unmet needs, such as males, persons with an alcohol use disorder, and those with less education. At the health service level there is a need for education on co-occurring somatic and psychiatric problems. Also, persons with low social support need extra attention.
Acknowledgments
This study was supported with grants from the Swedish Medical Research Council and the Stockholm Community Council.
Dr. Forsell is affiliated with the department of social medicine at the Institute of Public Health, Karolinska Institutet, Norrbacka, Karolinska Hospital, Stockholm, S-17176, Sweden (e-mail, [email protected]).
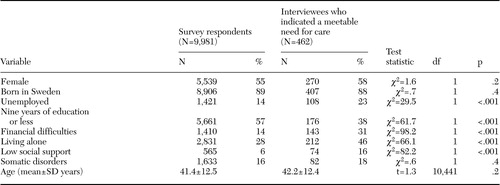 |
Table 1. Characteristics of persons who were interviewed and who indicated that they had a meetable need for mental health care and of the rest of the sample that responded to a survey in Sweden
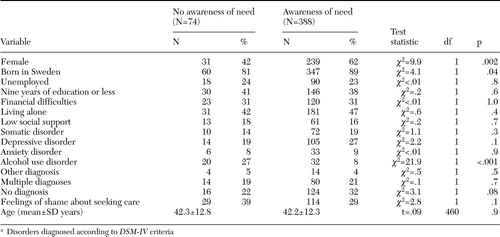 |
Table 2. Characteristics of persons who had a meetable need for mental health care (N=462), by their awareness of needa
a Disorders diagnosed according to DSM-IV criteria
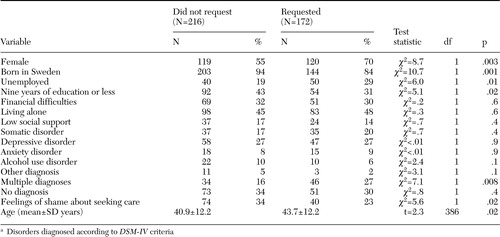 |
Table 3. Characteristics of persons who were aware of their need for mental health care (N=388), by whether they requested carea
a Disorders diagnosed according to DSM-IV criteria
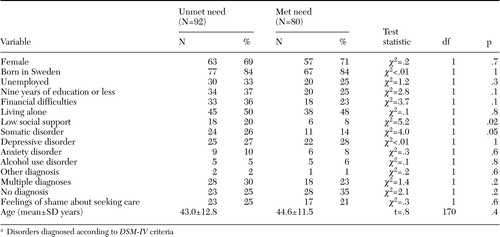 |
Table 4. Characteristics of persons who requested mental health care (N=172), by whether their needs were meta
a Disorders diagnosed according to DSM-IV criteria
1. The World Health Report 2001: Mental Health, New Understanding, New Hope. Geneva, World Health Organization, 2001Google Scholar
2. Henderson JG Jr, Pollard CA, Jacobi KA, et al: Help-seeking patterns of community residents with depressive symptoms. Journal of Affective Disorders 26:157–162,1992Crossref, Medline, Google Scholar
3. Bebbington PE, Marsden L, Brewin CR: The treatment of psychiatric disorder in the community: reports from the Camberwell needs for care survey. Psychological Medicine 27:821–834,1996Crossref, Google Scholar
4. Bebbington PE, Marsden L, Brewin CR: The need for psychiatric treatment in the general population: the Camberwell needs for care survey. Psychological Medicine 26:229–236,1997Crossref, Google Scholar
5. Kessler RC, Frank RG, Edlund M, et al: Differences in the use of psychiatric services between the United States and Ontario. New England Journal of Medicine 336:551–557,1997Crossref, Medline, Google Scholar
6. Bijl RV, Ravelli A: Psychiatric morbidity, service uses, and need for care in the general population: results from the Netherlands mental health survey and incidence study. American Journal of Public Health 90:602–607,2000Crossref, Medline, Google Scholar
7. Paykel ES, Tylee A, Wright A, et al: The Defeat Depression Campaign: psychiatry in the public arena. American Journal of Psychiatry 154:59–65,1997Link, Google Scholar
8. Paton J, Jenkins R, Scott J: Collective approaches for the control of depression in England. Social Psychiatry and Psychiatric Epidemiology 36:423–428,2000Crossref, Google Scholar
9. McConnell P, Bebbington P, McClelland R, et al: Prevalence of psychiatric disorder and the need for psychiatric care in Northern Ireland. British Journal of Psychiatry 181:224–219,2002Google Scholar
10. Kessler RC, McConagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the US: results from the national comorbidity survey. Archives of General Psychiatry 51:8–19,1994Crossref, Medline, Google Scholar
11. Lefebre J, Cyr M, Lesage A, et al: Unmet need in the community: can existing services meet them? Acta Psychiatrica Scandinavica 102:65–70,2000Google Scholar
12. Borowsky SJ, Rubenstein LV, Meredith LS, et al: Who is at risk for nondetection of mental health problems in primary care? Journal of General Internal Medicine 15:882–388,2000Google Scholar
13. Marshall M, Hogg LI, Gath DH, et al: The cardinal needs for care schedule: a modified version of the MRC Needs for Care Schedule. Psychological Medicine 25:605–617,1995Crossref, Medline, Google Scholar
14. Wells JE, Robins LN, Bushnell JA, et al: Perceived barriers to care in St Louis (USA) and Christchurch (NZ): reasons for not seeking professional help for psychological distress. Social Psychiatry and Psychiatric Epidemiology 29:155–164,1994Medline, Google Scholar
15. Jorm AF, Korten AE, Jacomb PA, et al: Mental health literacy: a survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia 166:182–186,1997Crossref, Medline, Google Scholar
16. Jorm AF, Angermyer M, Katschnig H: Public knowledge of and attitudes to mental disorders: a limiting factor in the optimal use of treatment services, in Unmet Need in Psychiatry. Edited by Andrews G, Henderson S. United Kingdom, Cambridge University Press, 2000Google Scholar
17. Meltzer H, Bebbington P, Brugha T: The reluctance to seek treatment for neurotic disorders. Mental Health 9:335–343,2000Google Scholar
18. Goldberg DP, Huxley P: Mental illness in the community: the pathway to psychiatric care. Tavistock, London, 1980Google Scholar
19. Hällström T, Damström Thakker K, Forsell Y, et al: The PART Study: A Population Based Study of Mental Health in the Stockholm County: Study Design: Phase l (1998-2000). Available at www.folkhalsoguiden.se/templates/publication_565.aspxGoogle Scholar
20. Sheehan DV: The Anxiety Disease: New Hope for the Millions Who Suffer From Anxiety. New York, Scribner, 1983Google Scholar
21. Marks IM, Mathews AM: Brief standard self-rating for phobic patients. Behavioural Research Therapy 17:263–267,1979Crossref, Medline, Google Scholar
22. Goodman WK, Price LH, Rasmussen SA, et al: The Yale-Brown Obsessive-Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry 46:1006–1011,1989Crossref, Medline, Google Scholar
23. Bech P, Wermuth L: Applicability and validity of the Major Depression Inventory in patients with Parkinson's disease. Nordic Journal of Psychiatry 52:305–309,1998Crossref, Google Scholar
24. Saunders JB, Aasland OG, Babor H, et al: Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction 88:791–804,1993Crossref, Medline, Google Scholar
25. Beglin SJ, Fairburn CG: Evaluation of a new instrument for the detection of eating disorders in community samples. Psychiatric Research 44:191–201,1992Crossref, Medline, Google Scholar
26. Janca A, Kastrup M, Katschnig H, et al: The World Health Organization Short Disability Assessment Schedule (WHO DAS-S): a tool for the assessment of difficulties in selected areas of functioning of patients with mental disorders. Social Psychiatry and Psychiatric Epidemiology 31:349–354,1996Crossref, Medline, Google Scholar
27. Lundberg I, Damström Thakker K, Hallström T, et al: Determinants of non-participation, and the effects of non-participation on potential cause-effect relationships, in the PART study on mental disorders. Social Psychiatry and Psychiatric Epidemiology 40:475–483,2005Crossref, Medline, Google Scholar
28. Wing JK, Babor T, Brugha T, et al: SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Archives of General Psychiatry 47:589–593,1990Crossref, Medline, Google Scholar
29. Brewin CR, Wing JK, Mangen SP, et al: Principles and practice of measuring need in the long term mentally ill: the MRC Needs for Care Assessment. Psychological Medicine 17:971–991,1987Crossref, Medline, Google Scholar
30. Brewin CR, Wing JK, Mangen SP, et al: Need for care among the long-term mentally ill: a report from the Camberwell high contact survey. Psychological Medicine 18:457–468,1988Crossref, Medline, Google Scholar
31. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
32. Undén AL, Orth-Gomer K: Development of a social support instrument for use in population surveys. Social Science and Medicine 1387-1392, 1989Google Scholar
33. SPSS 10.0 for Macintosh: Brief Guide. Chicago, SPSS Inc, 2000Google Scholar
34. Algria M, Kessler RC, Bijl R, et al: Comparing data on mental health service use between countries, in Unmet Need in Psychiatry. Edited by Andrews G, Henderson S. Cambridge, University Press, 2000Google Scholar



