Recent Sexual Abuse, Physical Abuse, and Suicide Attempts Among Male Veterans Seeking Psychiatric Treatment
Abstract
OBJECTIVES: This study examined the rates of sexual and physical abuse and suicide attempts among male and female patients and focused on the associations between sexual and physical abuse and recent suicide attempts among men. METHODS: Data were examined for a cohort of patients aged 19 years and older who were seeking treatment for substance use disorders, other psychiatric disorders, or both from the Department of Veterans Affairs (VA) between July 1997 and September 1997. Almost all the patients in the sample (more than 99 percent) had a substance use disorder. Patients were interviewed with the Addiction Severity Index about lifetime and recent (past 30 days) sexual and physical abuse and recent suicide attempts. Because of the low prevalence of suicide attempts in the past 30 days and limited representation of female patients in this sample, the data for female patients were used only to conduct descriptive analyses to compare the prevalence of sexual and physical abuse and suicide attempts between genders. RESULTS: The sample comprised 34,245 patients (33,236 males and 1,009 females). Compared with male patients, female patients were ten times as likely to have been sexually abused in the past 30 days and four times as likely to have been physically abused. Among male patients, bivariate analyses showed that those who had been recently sexually or physically abused were more likely than those who had not experienced such abuse to have attempted suicide recently (odds ratios of 4.8 and 3.0, respectively). After controlling for demographic and diagnostic factors, multivariate logistic regression analyses indicated that recent sexual abuse, recent physical abuse, and lifetime sexual abuse were significantly associated with a higher likelihood of a recent suicide attempt among male patients. CONCLUSIONS: Female patients were more likely than their male counterparts to experience sexual and physical abuse. Recent and lifetime history of sexual abuse and recent physical abuse were independent risk factors for recent suicide attempts among men who were seeking treatment. The results suggest that clinicians who identify suicide attempts and suicidal tendencies among male patients should routinely assess for sexual or physical abuse.
Although an association between sexual and physical abuse and attempted suicide has been established, our understanding of this association is limited. Previous research has four main limitations. First, no study has examined the association between recent (for example, in the past 30 days) sexual or physical abuse and recent suicide attempts among adults. Instead, most studies have focused on sexual or physical abuse among children and adolescents (1,2,3) or have relied on adults' retrospective reports of sexual or physical abuse in the remote past (4,5,6,7,8). Furthermore, many studies have examined suicide attempts over the lifetime (6,7). Therefore, it is difficult to discern whether incidents of abuse and suicide attempts were closely related in time. Second, little is known about these associations among men, because most studies' findings are based on relatively small samples and few incidents of sexual or physical abuse and suicide attempts among men (2,6). Consequently, multivariate analyses either have not been possible (9) or could include only a limited number of independent variables (6). Third, previous studies have identified associations between suicide attempts and psychotic disorders (10), affective disorders (10,11,12), posttraumatic stress disorder (10), anxiety disorders (10,11,12,13), substance use disorders (10,11), personality disorders (10), and demographic variables (10). However, no study has controlled for the impact of all these variables when examining the associations between sexual or physical abuse and suicide attempts. Finally, recent and remote abuse has not been differentiated in previous studies.
Accordingly, after presenting data that compare the rates of sexual and physical abuse and suicide attempts among male and female patients, we focus on the more numerous male patients in our sample and address three questions: Is there an association between lifetime and, particularly, recent sexual abuse and suicide attempts? Is there an association between lifetime or recent physical abuse and suicide attempts? Do experiences of sexual and physical abuse contribute independently to suicide attempts? We examined these associations after controlling for demographic factors and psychiatric disorders, using cross-sectional data from interviews of patients who were seeking treatment for substance use disorders, other psychiatric disorders, or both.
Methods
Participants
To evaluate the process and outcome of care for patients with substance use disorders, the Department of Veterans Affairs (VA) mandated that clinicians, as part of ongoing clinical practice, use the Addiction Severity Index (ASI) (14) to assess all such patients upon entry to treatment. This project was designed to monitor and improve the quality of care and treatment, for which separate informed consent was not required. We report here on findings for a 12-month cohort (July 1997 to September 1997) of patients who were seeking treatment for substance use disorders, other psychiatric disorders, or both in one of 150 VA facilities across the United States. Almost all the patients in the sample (more than 99 percent) had a substance use disorder.
Because of the low prevalence of attempted suicide in the past 30 days and limited representation of female patients in this sample, the data for the female patients were used only to conduct descriptive analyses to compare the prevalence of abuse and suicide attempts between genders. The main findings are based on data for male patients.
Procedure
The Addiction Severity Index (ASI) was selected as the assessment instrument for outcomes monitoring because it has established reliability and validity (15,16,17), clinicians in many VA programs had already used it as part of their standard intake assessment battery, and it had been widely used in a number of substance use disorder treatment systems. To ensure consistency and reliability the VA organized a nationwide program to train clinical staff who routinely provided treatment to patients with substance use disorders to conduct ASI interviews (18). The VA Employee Education System coordinated a series of eight two-day training sessions that were conducted by expert ASI interviewers in three locations nationwide. Each training session included information about the rationale and purpose of the ASI, a review of the ASI interview procedures, videotaped presentations of ASI interviews, and work with the VA computer system and ASI data entry procedures (19). Patients were interviewed with the ASI after entering treatment for a substance use disorder.
Measures
Suicide attempt. Clinical staff assessed suicide attempts in the past 30 days and lifetime suicide attempts before the past 30 days as part of the psychiatric module of the ASI (14). Self-harming behaviors in which the person did not have the intent to die were not regarded as suicide attempts.
Sexual and physical abuse. The ASI uses nine items to assess problems with the mother, father, brothers and sisters, sexual partner or spouse, children, other significant family members, close friends, neighbors, and coworkers. Interviewers then ask, "Did any of these people abuse you sexually (force sexual advances or sexual acts) or physically (cause you physical harm)" in your lifetime or in the past 30 days? Interviewers were trained to assess and code abuses in the past 30 days and abuses in the lifetime before the past 30 days. Najavits and colleagues (20) reported good interrater agreement and concurrent validity between the ASI items that assessed lifetime abuse and another measure of abuse (the Trauma History Questionnaire).
Psychiatric diagnoses. We obtained information from nationwide VA databases about patients' psychiatric and substance use diagnoses in the index episode of care. We focused on whether the following current diagnoses were present (code of 1) or absent (code of 0): psychotic disorders, depressive disorders, posttraumatic stress disorder, other anxiety disorders, alcohol abuse or dependence, drug abuse or dependence, and personality disorders (antisocial and borderline). Diagnoses were made by experienced clinicians during regular clinical intake interviews in the usual process of care.
Demographic factors. Demographic information was also available from the ASI. Age and education were analyzed as continuous variables in number of years. Race was categorized as white (1) or other (0), and marital status was coded as married (1) or not married (0).
Analysis
Bivariate analyses (chi square analysis and logistic regression) were conducted to examine differences in rates of sexual or physical abuse and suicide attempts among male and female patients, as well as the associations between abuse and suicide attempts and the association of suicide attempts with psychiatric and substance use disorders and demographic factors. To examine the predictive relationships of sexual and physical abuse, multivariate logistic regression analyses were conducted, with a suicide attempt in the past 30 days regressed on lifetime and recent sexual and physical abuse and all covariates that were significantly associated with suicide attempts in the bivariate analyses. Bonferroni-corrected alpha levels were used to reduce the chance of a type I error. The data were analyzed with SPSS 11.5 for Windows (21).
Results
The 34,245 patients had a mean±SD age of 46.6±9.4 years and had a mean of 12.5±2.1 years of education. Among the patients, 18,710 (55 percent) were white, 12,429 (37 percent) were black, 2,072 (6 percent) were Hispanic or Latino, and 706 (2 percent) were from another racial groups. Only 7,478 (22 percent) were currently married, 18,271 (54 percent) were separated or divorced, 1,187 (3 percent) were widowed, and 7,008 (21 percent) had never been married. A total of 33,236 patients were male (97 percent), and 1,009 were female (3 percent). For a more detailed description of the sample, see the study by Moos and colleagues (22).
Table 1 shows 30-day and lifetime prevalence of suicide attempts, sexual abuse, and physical abuse among male and female VA patients who were seeking treatment for substance use disorders, other psychiatric disorders, or both. Lifetime prevalence including and excluding occurrences in the past 30 days are labeled "lifetime ever" and "lifetime before the past 30 days," respectively. In the past 30 days, 3.4 percent of the male patients had attempted suicide, .5 percent had been sexually abused, and 2.7 percent had been physically abused. Over the entire lifetime, 26.7 percent of the male patients had attempted suicide, 8.4 percent had been sexually abused, and 25.5 percent had been physically abused.
Compared with male patients, female patients were ten times as likely (odds ratio [OR]=9.97) to have been abused sexually in the past 30 days (4.9 percent compared with .5 percent) and four times as likely (OR=4.05) to have been abused physically in the past 30 days (10.1 percent compared with 2.7 percent). Female patients were also twice as likely (OR=2.10) to have attempted suicide (43.3 percent), 12 times as likely (OR=11.62) to have been abused sexually (51.5 percent), and five times as likely (OR=5.01) to have been abused physically (63.1 percent) over the entire lifetime.
Sexual abuse and suicide attempts
Table 2 shows that male patients who had been sexually abused in the past 30 days were more than four times as likely as male patients who had not experienced such abuse (OR=4.8) to have attempted suicide in the past 30 days. Among male patients who were sexually abused in the past 30 days, 14.2 percent had attempted suicide in the same period, compared with 3.3 percent of male patients who had not experienced such abuse. Male patients who had been sexually abused at any point in their lifetimes were more likely to have attempted suicide in the past 30 days (6.6 percent compared with 3.1 percent; OR=2.3).
Relationship between physical abuse and suicide attempts
Male patients who had been physically abused in the past 30 days were three times as likely as those who had not experienced such abuse to have attempted suicide in the past 30 days (9.2 percent compared with 3.2 percent) (Table 2). Male patients who had been physically abused at any point over the lifetime were also more likely than male patients who had not experienced such abuse to have recently attempted suicide (4.9 percent compared with 2.8 percent; OR=1.8).
Psychiatric disorders, demographic factors, and suicide attempts
As shown in Table 3, there was a statistically significant increase of the odds of a suicide attempt in the past 30 days among patients who had been given a diagnosis of one of the following disorders during the index treatment episode: psychotic disorder (OR=2.2), any depressive disorder (OR=3.3), posttraumatic stress disorder (OR=2.0), other anxiety disorder (OR=2.5), alcohol abuse or dependence (OR=1.3), drug abuse or dependence (OR=1.5), and personality disorder (OR=3.0). The odds of a suicide attempt in the past 30 days were lower among patients who were married (OR=.80) and older (OR=.97 for each additional year).
Multivariate association of suicide attempts
Table 4 shows the results of a multivariate logistic regression analysis with a suicide attempt in the past 30 days regressed on sexual abuse, physical abuse, and all covariates that were significantly associated with suicide attempts in the bivariate analyses in Table 3 (all factors except for race and years of education). The results indicated a significant increase in adjusted odds for a suicide attempt in the past 30 days among male patients who had experienced sexual abuse in the past 30 days (adjusted OR=2.1), physical abuse in the past 30 days (adjusted OR=2.4), and lifetime sexual abuse before the past 30 days (adjusted OR=1.3). Among the covariates, a suicide attempt in the past 30 days was associated with the presence of a psychotic disorder (adjusted OR=1.5), depressive disorder (adjusted OR=2.4), posttraumatic stress disorder (adjusted OR=1.4), other anxiety disorder (adjusted OR=1.5), and personality disorder (adjusted OR=1.7) and with being younger (adjusted OR=.97 for each additional year). Follow-up multivariate logistic regression analysis (not shown) indicated that there were no significant interaction effects at the Bonferroni-adjusted level of .004 (.05 of 13 independent variables) for sexual and physical abuse in the past 30 days and in the lifetime before the past 30 days (p=.02).
Discussion
This study is the first to examine recent sexual and physical abuse and recent suicide attempts among men. Unlike most previous studies of abuse and suicide attempts among men, this study had a sample that was large enough (N=33,236) to allow for the inclusion of several covariates simultaneously in multivariate statistical models that examined the relationships between sexual and physical abuse and suicide attempts. The associations between sexual and physical abuse and suicide attempts are robust. The results show more than a fourfold higher likelihood of a suicide attempt in the past 30 days among male patients who were sexually abused in the past 30 days and a threefold higher likelihood among patients who were physically abused in the past 30 days. Relationships of both recent sexual abuse and recent physical abuse to a recent suicide attempt were independent of each other and of lifetime history of sexual and physical abuse and psychiatric and substance use disorders that were associated with a recent suicide attempt.
This study was distinct from many previous studies that relied on lifetime abuse alone, because it was able to separate the associations between recent suicide attempts and recent and lifetime sexual and physical abuse. We found that lifetime sexual abuse and lifetime physical abuse were associated with a recent suicide attempt. Furthermore, the association between lifetime sexual abuse and a recent suicide attempt continued to be statistically significant when recent abuse, psychiatric and substance use disorders, and demographic factors were included in the model. However, in the multivariate model only recent physical abuse was associated with a recent suicide attempt. The effects of physical abuse in the remote past on recent suicide attempts may be mediated completely through psychiatric disorders that were captured in the multivariate model.
This study replicates previous findings (10,11,12,13) on the associations between psychiatric disorders and attempted suicide. Psychotic disorder, depressive disorder, posttraumatic stress disorder, other anxiety disorder, and personality disorder were each associated with suicide attempts, even when sexual and physical abuse, demographic factors, and the other psychiatric disorders were simultaneously included in the analyses.
This study shows that many male patients who were seeking treatment for substance use disorders, other psychiatric disorders, or both had been abused and that the rate of suicide attempts was higher among the patients who had been abused. Eight percent of the male patients had been sexually abused and 25.5 percent had been physically abused in their lifetimes. In the past 30 days, .5 percent of the male patients had been sexually abused, and 2.7 percent had been physically abused. This level of short-term prevalence is sufficiently high to suggest repeated abuse. About one in seven (14.2 percent) male patients who had been sexually abused and one in 11 (9.2 percent) male patients who had been physically abused in the past 30 days attempted suicide in the past 30 days.
Women veterans who were seeking treatment for substance use disorders, other psychiatric disorders, or both had even higher rates of sexual and physical abuse than their male counterparts. A majority of these women had been sexually abused (51.5 percent) and almost two-thirds (63.1 percent) had been physically abused in their lifetimes. These figures represent more than an 11-fold higher likelihood of sexual abuse and a fivefold higher likelihood of physical abuse, compared with male patients. In the past 30 days alone, 4.9 percent of female patients had been sexually abused and 10.1 percent had been physically abused. That is close to a tenfold higher likelihood of sexual abuse and a fourfold higher likelihood of physical abuse, compared with male patients. Again, such a high prevalence in the past 30 days suggests that many women were being repeatedly abused in their lifetimes.
Previous studies have shown much lower rates of lifetime suicide attempts in other samples. For example, Dube and colleagues (7) conducted a study that examined 17,337 members of a health maintenance organization (HMO) and showed that the lifetime prevalence of having at least one suicide attempts was 3.8 percent and that the prevalence was higher for women than for men (5.4 percent compared with 1.9 percent). In the Netherlands, Langeland and colleagues (23) showed that among 155 alcoholics, 22.1 percent of the men and 33.3 percent of the women who were seeking treatment for substance use disorders, other psychiatric disorders, or both disorder reported at least one suicide attempts in their lifetime. The study reported here shows higher rates of lifetime suicide attempts among both men and women than in the Netherlands sample. This difference may result from more severe psychopathology of VA patients with a substance use disorder.
Similarly, women who were seeking treatment for substance use disorders, other psychiatric disorders, or both in the VA had a higher prevalence of sexual or physical abuse than women in other samples. For example, Dube and colleagues (7) reported that among female members of an HMO, 27 percent were physically abused and 24.7 percent were sexually abused in their lifetimes, compared with rates of 63.1 and 51.5 percent, respectively, in the study reported here. However, men who were seeking treatment for substance use disorders, other psychiatric disorders, or both in the VA had a comparable rate of physical abuse and a lower rate of sexual abuse than the men in the Netherlands sample. Also, Dube and colleagues reported that among male members of an HMO, 29.9 percent were physically abused and 16 percent were sexually abused in their lifetimes, compared with 25.5 and 8.4 percent, respectively, in the study reported here. Perhaps men who have served in the military are less likely to be sexually abused or less likely to admit sexual abuse.
This study has two major limitations. First, its cross-sectional nature did not enable us to provide information on whether abuse preceded or followed a suicide attempt in the past 30 days. However, it seems much more likely that a suicide attempt would follow sexual or physical abuse. Second, more than 80 percent of the patients in the sample had an alcohol use disorder and more than 80 percent had a drug use disorder. Therefore, our findings may underestimate the strength of the associations between substance use disorders and suicide attempts; the associations may be stronger in more heterogeneous samples with a lower prevalence of substance use disorders. Consequently, the lack of an independent association between alcohol and drug use disorders and suicide attempts should be interpreted with caution.
Conclusions
This study shows that both lifetime and recent physical and sexual abuse are associated with recent suicide attempts among men. Furthermore, recent physical abuse, lifetime sexual abuse, and recent sexual abuse continued to be associated with a recent suicide attempt after the analysis controlled for demographic factors and diagnoses. Recent physical and sexual abuse may be a precipitant of a suicide attempt and may heighten the risk of a subsequent attempt. This connection likely reflects the especially profound impact of physical or sexual abuse among men, caused by severe shame, guilt, loss of self-esteem, threat to masculinity, or homosexual fear.
Patients with substance use disorders who have a history of physical or sexual abuse have a higher risk of problematic treatment outcomes because of more severe psychiatric problems, deficits in social support, and interpersonal problems that lead to difficulties in establishing a treatment alliance. In this regard, more frequent treatment contacts may be especially beneficial for patients who have been physically or sexually abused (24,25). Accordingly, clinicians who identify suicide attempts or tendencies among male patients should routinely assess for abuse in order to tailor interventions to address these patients' problems and reduce the likelihood of subsequent suicidal ideation and behavior.
Acknowledgments
Preparation of this manuscript was supported in part by the Department of Veterans Affairs (VA) Health Services Research and Development Service, Program Evaluation, and Resource Center and the Center for Health Care Evaluation, VA Palo Alto Health Care System.
The authors are affiliated with the Center for Health Care Evaluation at the Department of Veterans Affairs (VA) Palo Alto Health Care System in Menlo Park, California, and the department of psychiatry and behavioral sciences at Stanford University School of Medicine in Stanford, California. Send correspondence to Dr. Tiet at VA Palo Alto Health Care System, Center for Health Care Evaluation, 795 Willow Road (MPD-152), Menlo Park, California 94025 (e-mail, [email protected]).
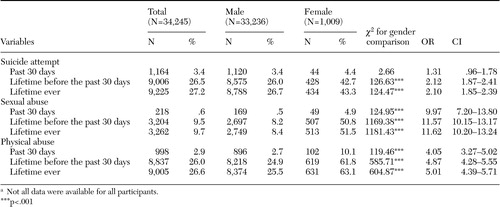 |
Table 1. Prevalence of suicide attempts, sexual abuse, and physical abuse among patients who were seeking treatment for substance use disorders, other psychiatric disorders, or both through the Department of Veterans Affairsa
a Not all data were available for all participants.
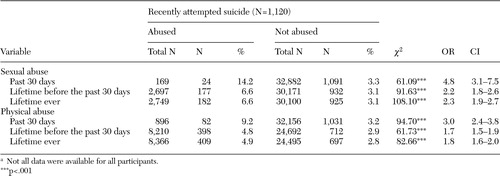 |
Table 2. Bivariate associations of sexual and physical abuse with a suicide attempt in the past 30 days among 33,236 males who were seeking treatment for substance use disorders, other psychiatric disorders, or both through the Department of Veterans Affairsa
a Not all data were available for all participants.
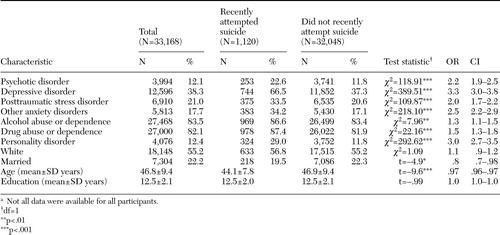 |
Table 3. Diagnostic and demographic characteristics and bivariate associations of suicide attempts in the past 30 days among males who were seeking treatment for substance use disorders, other psychiatric disorders, or both through the Department of Veterans Affairsa
a Not all data were available for all participants.
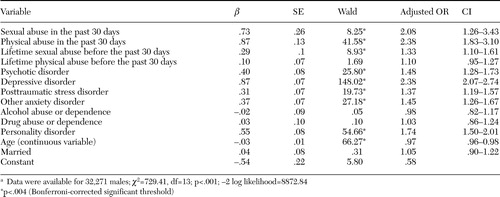 |
Table 4. Results of a multivariate logistic regression analysis of suicide attempts in the past 30 days among males who were seeking treatment for substance use disorders, other psychiatric disorders, or both through the Department of Veterans Affairsa
a Data were available for 32,271 males; χ2=729.41, df=13; p<.001; -2 log likelihood=8872.84
1. Hershberger SL, D'Augelli AR: The impact of victimization on the mental health and suicidality of lesbian, gay, and bisexual youths. Developmental Psychology 31:65–74,1995Crossref, Google Scholar
2. Lipschitz DS, Winegar RK, Nicolaou AL, et al: Perceived abuse and neglect as risk factors for suicidal behavior in adolescent inpatients. Journal of Nervous and Mental Disease 187:32–39,1999Crossref, Medline, Google Scholar
3. Sedney MA, Brooks B: Factors associated with a history of childhood sexual experience in a nonclinical female population. Journal of the American Academy of Child and Adolescent Psychiatry 23:215–218,1984Crossref, Google Scholar
4. Benda BB: Discriminators of suicide thoughts and attempts among homeless veterans who abuse substances. Suicide and Life Threatening Behavior 33:430–442,2003Crossref, Medline, Google Scholar
5. Briere J, Evans D, Runtz M, et al: Symptomatology in men who were molested as children: a comparison study. American Journal of Orthopsychiatry 58:457–461,1988Crossref, Medline, Google Scholar
6. Davidson JRT, Hughes DC, George LK, et al: The association of sexual assault and attempted suicide within the community. Archives of General Psychiatry 53:550–555,1996Crossref, Medline, Google Scholar
7. Dube SR, Anda RF, Felitti VJ, et al: Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 286:3089–3096,2001Crossref, Medline, Google Scholar
8. Kroll PD, Stock DF, James ME: The behavior of adult alcoholic men abused as children. Journal of Nervous and Mental Disease 173:689–693,1985Crossref, Medline, Google Scholar
9. Simon TR, Anderson M, Thompson MP, et al: Assault victimization and suicidal ideation or behavior within a national sample of US adults. Suicide and Life Threatening Behavior 32:42–50,2002Crossref, Medline, Google Scholar
10. Kessler RC, Borges G, Walters EE: Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry 56:617–626,1999Crossref, Medline, Google Scholar
11. Fergusson DM, Lynskey MT: Suicide attempts and suicidal ideation in a birth cohort of 16-year-old New Zealanders. Journal of the American Academy of Child and Adolescent Psychiatry 34:1308–1317,1995Crossref, Medline, Google Scholar
12. Johnson J, Weissman MM, Klerman GL: Panic disorder, comorbidity, and suicide attempts. Archives of General Psychiatry 47:805–808,1990Crossref, Medline, Google Scholar
13. Weissman MM, Klerman GL, Markowitz JS, et al: Suicidal ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine 321:1209–1214,1989Crossref, Medline, Google Scholar
14. McLellan AT, Kushner H, Metzger D, et al: The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213,1992Crossref, Medline, Google Scholar
15. Argeriou M, McCarty D, Mulvey K, et al: Use of the Addiction Severity Index with homeless substance abusers. Journal of Substance Abuse Treatment 11:359–365,1994Crossref, Medline, Google Scholar
16. McLellan AT, Luborsky L, Cacciola J, et al: New data from the Addiction Severity Index: reliability and validity in three centers. Journal of Nervous and Mental Disease 173:412–23,1985Crossref, Medline, Google Scholar
17. Zanis DA, McLellan AT, Cnaan RA, et al: Reliability and validity of the Addiction Severity Index with a homeless sample. Journal of Substance Abuse Treatment 11:541–548,1994Crossref, Medline, Google Scholar
18. Moos RH, Finney JW, Canon D, et al: Outcomes Monitoring for Substance Abuse Patients: Patients' Characteristics and Treatment at Baseline. Washington, DC, Department of Veterans Affairs, 1998Google Scholar
19. Fureman B, Parikh G, Bragg A, et al: The Fifth Edition of the Addiction Severity Index Workbook. Philadelphia, University of Pennsylvania and Center for Studies of Addiction, Department of Veterans Affairs, 1990Google Scholar
20. Najavits LM, Weiss RD, Reif S, et al: The addiction severity index as a screen for trauma and posttraumatic stress disorder. Journal of Studies on Alcohol 59:56–62,1998Crossref, Medline, Google Scholar
21. SPSS 11.5 Syntax Reference Guide. Chicago, SPSS, 2002Google Scholar
22. Moos RH, Finney JW, Federman EB, et al: Specialty mental health care improves patients' outcomes: findings from a nationwide program to monitor the quality of care for patients with substance use disorders. Journal of Studies on Alcohol 61:704–713,2000Crossref, Medline, Google Scholar
23. Langeland W, Draijer N, van den Brink W: Psychiatric comorbidity in treatment-seeking alcoholics: the role of childhood trauma and perceived parental dysfunction. Alcoholism, Clinical, and Experimental Research 28:441–447,2004Crossref, Medline, Google Scholar
24. Rosen CS, Ouimette PC, Sheikh JI, et al: Physical and sexual abuse history and addiction treatment outcomes. Journal of Studies on Alcohol 63:683–687,2002Crossref, Medline, Google Scholar
25. Ouimette PC, Kimerling R, Shaw J, et al: Physical and sexual abuse among women and men with substance use disorders. Alcoholism Treatment Quarterly 18:7–17,2000Crossref, Google Scholar



