Medical Advance Care Planning for Persons With Serious Mental Illness
Abstract
OBJECTIVE: This study examined preferences regarding medical advance care planning among persons with serious mental illness, specifically, experience, beliefs, values, and concerns about health care proxies and end-of-life issues. METHODS: A structured interview, the Health Care Preferences Questionnaire, was administered to a convenience sample of 150 adults with serious mental illness who were receiving community-based services from the Massachusetts Department of Mental Health. Clinical information and demographic data were also collected. RESULTS: A total of 142 participants completed the questionnaire. Although more than one-quarter had thought about their medical treatment preferences in the event that they became seriously medically ill, very few had discussed these preferences. A majority of respondents (72 percent) believed that someone should be designated to make medical health care decisions for a person who is too sick to make or communicate these decisions him- or herself. Common end-of-life concerns included financial and emotional burdens on family, pain and suffering, interpersonal issues such as saying "goodbye," spiritual issues, and funeral arrangements. Participants were most uneasy about the prolonging or stopping of life support by proxy decision makers. A total of 104 respondents (69 percent) expressed interest in formally selecting a health care proxy. CONCLUSIONS: Although persons with serious and persistent mental illness have little experience with medical advance care planning, they show substantial interest in it. Furthermore, they are able to consider and communicate their preferences. This study supports the feasibility, acceptability, and utility of a standardized approach to medical advance care planning with this population.
End-of-life care planning through written advance directives and designation of a proxy promotes individual health care preferences after decision-making capacity is lost (1). Extensive research describes end-of-life care planning and preferences in the general medical population (2,3,4,5), but little is known about this topic for persons with serious mental illness.
Approximately 50 percent of psychiatric patients have known medical conditions, and 35 percent have undetected medical conditions (6). The life expectancy of individuals with schizophrenia is nine or ten years shorter than that expected for the general population (6,7,8,9). Furthermore, medical comorbidity is associated with more serious psychiatric symptoms, worse health status, and worsened health care outcomes (6,10,11,12,13,14,15,16). Despite poor health outcomes, individuals with serious mental illness have limited opportunities to engage in advance care planning discussions (17). Many who have thought disorders, cognitive deficits, and emotional dysregulation are assumed to have impaired capacities to formulate and communicate health care choices (18,19,20,21), and persons with guardianships are automatically excluded from advance care planning (22).
Capacity to make treatment decisions often fluctuates over the course of mental illness. For example, understanding treatment options can be impeded by psychiatric symptoms or cognitive disorganization (23). Similarly, individuals with schizophrenia may have acute psychotic symptoms or long-standing thought disorders that can impair their ability to make informed decisions (24). Tailored educational interventions can improve understanding to a level that falls within the range of informed decision-making capacity (24). Thus several states have created statutes that reflect "fluctuating capacity" of persons with serious mental illness, allowing for documentation of treatment preferences during an individual's stable and competent phases (25). Although the Patient Self-Determination Act (PSDA) (26) requires federally funded health care facilities to inform competent patients of their right to make medical care decisions, including accepting or refusing treatment and completing advance directives, application of the act to persons with serious mental illness has focused on psychiatric advance directives (22,27,28). Legal, medical, and ethics scholars argue that the PSDA grants individuals who have serious mental illness the right to document preferences for psychiatric treatments in the event that they become incompetent to participate in decision making as a result of their mental illness (22,29,30,31,32).
In contrast to psychiatric advance directives, medical advance care planning has been neglected for persons with serious mental illness (33,34). However, it has been extensively studied in the general population. Advance care planning studies have increased steadily over the past decade (35), and a vast and culturally diverse literature of research domains, toolkits, organizational principles, and policies now exists (36,37). However, it is not known whether these innovations apply to persons with serious mental illness, because this group has been specifically excluded from the research (38). The purpose of this article is to provide descriptive information about mental health consumers' attitudes, concerns, preferences, and experiences with medical advance directives and end-of-life issues.
Methods
Participants
The study participants were clients of the Massachusetts Department of Mental Health who were receiving services from one of five contracted community mental health agencies. Two agencies were located in suburban settings and three in urban environments. All participants met state criteria for a serious and persistent mental illness, consisting of a DSM-IV chart diagnosis of an axis I or axis II disorder with directly related functional disability as measured by the Current Evaluation of Risk and Functioning-Revised (CERF-R), an 18-item scale assessing client functioning and risk (39,40). Participants were 18 years of age or older, were able to communicate in English, and provided written informed consent. If a potential participant was legally incompetent—that is, under guardianship—and willing to participate, written informed consent was obtained from both the participant and the guardian. Two institutional review boards approved the study protocol and the document that was used for obtaining informed consent.
Measures
A data collection form was used to gather information about sociodemographic characteristics, psychiatric diagnoses, medications, medical conditions, frequency of medical specialty visits or hospitalizations, and CERF-R scores. Participants' health status, exposure to advance care planning, values, beliefs, and end-of-life concerns were obtained with use of the Health Care Preferences Questionnaire (HCPQ). (The HCPQ is available at www.promotingexcellence.org/mentalillness.)
The HCPQ documents participants' attitudes and preferences for scenario-specific choices (38,41) and assesses basic health care values (42,43,44). HCPQ components include health status, assessed with the Short-Form-12 (SF-12) (45,46); advance care planning; scenario-based treatment preferences; beliefs, values, and concerns about end of life; interview feedback and follow-up; and an interviewer's addendum.
Procedures
Agency staff were trained on the study objectives, the function of advance care planning, the purpose of a health care proxy, and appropriate procedures for obtaining informed consent. Twenty-seven interviewers were trained to administer the HCPQ by using practice sessions and a manual that included instructions for each item. Instructions reminded interviewers what to emphasize when reading the item, what items to skip on the basis of subjects' responses (skip patterns), and how to address questions or concerns from respondents. All interviewers completed a written test of their knowledge about advance care planning and demonstrated proficiency in administration of the HCPQ.
Recruitment of participants began in November 2000 and ended in July 2001. Posters and contact information were displayed in agencies' residential group homes and supported-housing complexes. As potential participants expressed interest, study coordinators responded with a cued script that explained the study and emphasized its voluntary nature. Participating agencies provided residential or supported housing services to approximately 450 psychiatric clients, of which the first 150 eligible volunteers were included in the study.
Analyses
Frequency distributions were computed for participants' demographic, diagnostic, and medical treatment characteristics; responses to HCPQ questions; and the interviewers' addendum. Narrative responses were analyzed by using a coding system developed by the authors that categorized response themes. Independent-sample t tests were used to compare CERF-R scores between the study sample and a community sample of consumers, and SF-12 physical and mental component scores between the study sample and the general population and selected subpopulations. Possible scores on the CERF-R domains range from 1 to 6, with higher scores indicating greater disability or greater risk. Scoring of the SF-12 physical component score and mental component score are norm based, with a mean±SD of 50±10; higher scores indicate better health functioning. Finally, chi square analyses and independent-sample t tests were used to identify relationships between attitudes toward advance directives and demographic and clinical characteristics. The medical scenario-based treatment preferences are discussed in our accompanying article in this issue of Psychiatric Services (47).
Results
Sample characteristics
The participants' demographic characteristics are summarized in Table 1. The participants were middle-aged (42±10 years) and predominantly Caucasian (137 respondents, or 91 percent). Most had never been married (129 respondents, or 86 percent), and more than half were men (83 respondents, or 55 percent). Psychiatric diagnoses included schizophrenia spectrum disorders (99 respondents, or 66 percent), affective disorders (42 respondents, or 28 percent), and personality disorders or posttraumatic stress disorder (nine respondents, or 6 percent). Most participants received a second- or first-generation antipsychotic (128 respondents, or 87 percent), approximately half received an antidepressant (69 respondents, or 47 percent) or an anticonvulsant or mood stabilizer (80 respondents, or 56 percent), and less than a third received an anxiolytic medication (43 respondents, or 29 percent). Sixty percent of the sample (90 respondents) had at least one medical diagnosis. The most common medical conditions included cardiovascular disease (33 respondents, or 22 percent), endocrine disease (19 respondents, or 13 percent), and respiratory illnesses (16 respondents, or 11 percent). More than half the respondents (78 respondents, or 52 percent) had had one to four medical appointments in the previous three months, and 7 percent (ten respondents) had had five or more appointments. Eleven clients (8 percent) had been hospitalized for a medical condition during the previous three months.
The participants had similar demographic, clinical, and functional characteristics to those of the larger Massachusetts Department of Mental Health population. However, minor differences were found with respect to four of the 18 CERF-R functional status domains. Compared with the larger population (N=4,631), the study participants were more likely to hold jobs (mean score of 3.8±1.7 compared with 4.3±1.7; t=3.24, df=4,733, p<.001), had lower service needs (2.4±1.0 compared with 2.7±1.2; t= 2.77, df=119.9, p=.007), had a lower risk of sexual offenses (1.1±.3 compared with 1.2±.6; t=3.70, df=135.8, p<.001), and had a lower risk of leaving services (1.7±1.1 compared with 1.9±1.2; t=2.13, df=4,738, p=.033).
The physical and mental health status of study participants was compared with published norms for the general population and with data for subgroups with chronic medical illness (45,46). Overall, the study participants had worse physical and mental health functioning compared with the general population and had similar physical functioning to individuals with diabetes and hypertension. Physical and mental component scores of the SF-12 were significantly lower for the study population (46.7±10.2 and 45.5±10.8, respectively) than for the general population (50.1±9.5 and 50.0±9.6, respectively; t=-4.25, df=2,475, p<.001 and t=-5.46, df=2,475, p<.001). However, physical component scores of the study sample were similar to those of persons with hypertension (46.5±7.0) and diabetes (44.8±15.9). As expected, mental component scores indicated greater impairment for study participants than for persons with hypertension (53.0±7.0; t=-8.86, df=456, p<.001) or diabetes (52.5±14.1; t=-5.31, df=456, p<.001) (45).
Advance care planning
Participants reported little experience with advance care planning. More than one-quarter (41 respondents, or 27 percent) indicated that they had existing preferences for medical treatment if they were to become seriously ill, but only 20 percent of these (eight respondents, or 5 percent of the entire sample) had spoken with their doctor about their preferences. Only three participants (2 percent) had documented their health care preferences. Participants with undocumented preferences explained that they had "never thought about writing them down before" (24 participants, or 57 percent), were "too young" or "felt it was too soon" (seven participants, or 17 percent), and had not "gotten around to it" (five participants, or 13 percent).
Beliefs, values, and end-of-life concerns
Most participants (108 participants, or 72 percent) believed that someone should be designated to make health care decisions for a person who is too sick to do so. Nearly two-thirds (93 respondents, or 62 percent) specified at least one individual who could act as their health care proxy, including a family member (61 respondents, or 66 percent); a physician, psychiatrist, or mental health care worker (22 respondents, or 23 percent); or a friend (seven respondents, or 7 percent). However, less than one-fifth (25 respondents, or 18 percent) had selected a person to act as their health care proxy.
Ninety-five percent of the sample (142 respondents) identified concerns about proxy decision making and end-of-life care issues. Leading concerns about proxy decision making (165 concerns identified) were those related to life support in the context of a coma or brain damage, including decisions to "pull the plug" and fears of remaining "a vegetable" (62 respondents, or 44 percent), the places in which the person would live and receive care (17 respondents, or 12 percent), medication or medical errors (12 respondents, or 9 percent), and issues related to a funeral, burial, cremation, or the person's will (12 respondents, or 9 percent). Nine participants (6 percent) indicated no concerns and believed that their family would take care of everything. Specific concerns about end-of-life care are shown in Table 2. The most common concerns were financial (33 percent) and emotional (30 percent) burden to family or loved ones, pain and suffering (30 percent), interpersonal issues (22 percent), funeral and disposition of the individual's body (21 percent), and spiritual concerns (16 percent).
Comfort, distress, and understanding of the questionnaire
The average time to complete the entire HCPQ was 43.6±16.1 minutes, with a range of 14 to 118 minutes. Ninety-six percent of participants (144 participants) completed the questionnaire, and 4 percent (six participants) terminated the process before completion. Among participants who completed the interview, most (84 participants, or 58 percent) were comfortable with the interview and "with talking about the end of life." Two-thirds of participants (98 participants, or 68 percent) reported minimal interview-related stress, 26 percent (38 participants) reported some stress to moderate stress, and 4 percent (six participants) reported a great amount of stress. Most (111 participants, or 77 percent) were willing to participate in a follow-up interview, and 103 (72 percent) expressed interest in receiving more information about completing a formal health care proxy designation.
The interviewers rated understanding and comfort with the questionnaire for 134 of 150 participants. Most participants (94 participants, or 70 percent) were described as not at all or not very uncomfortable. Only one participant was rated as extremely uncomfortable. Most participants (90 participants, or 71 percent) understood the questions without additional explanation, 35 participants (26 percent) required clarifications, and nine participants (7 percent) were rated as possibly having misunderstood some questions. Twenty-nine participants (22 percent) reacted negatively to at least one question; however, no untoward effects of such reactions were observed during or after the interview.
Diagnostic, demographic, and health status characteristics were examined to identify differences among participants' reactions to the interview. No differences were associated with patient-reported stress or comfort with the interview. In contrast, participants who were perceived by the interviewer as being uncomfortable with the interview had lower mental health functioning (mean mental component score of 42.4±10.6 compared with 47.5±10.5; t=2.55, df=130 p=.01), and participants who were perceived by the interviewer to have a negative reaction to any questions were younger (mean age of 38.7±10.1 years compared with 43.4±10.8 years; t=-2.10, df=132, p=.04).
Characteristics associated with end-of-life preferences
Few clinical or demographic differences were noted between participants with respect to end-of-life care preferences. As shown in Table 1, women were more likely than men to have preferences for medical treatment if they were to become seriously ill, to have selected a person to act as their health care proxy, and to want more information about selecting a proxy. Persons with worse physical health status were more likely to have selected a health care proxy, and individuals who had never been married were less likely to have selected a proxy. Caucasians were less likely than individuals from ethnic minority groups to have medical treatment preferences. Individuals who had made at least one medical visit in the past three months were more likely to be interested in obtaining more information about completing an advance directive than individuals who had made no visits. Finally, individuals who were older and had worse physical health status were more likely to believe that someone should make health care decisions for a seriously ill person, even in the absence of written instructions.
No other demographic characteristics were associated with interest in or preferences regarding advance care directives. Persons with preexisting end-of-life care preferences were more likely to have picked someone to be their health care proxy (14 participants, or 38 percent, compared with 11 participants, or 11 percent; χ2=13.04, df=1, p<.001). In addition, individuals who wanted additional information about completing an advance care directive were more likely to think that a person should be named to make health care decisions for a person who is too sick to do so (86 respondents, or 84 percent, compared with 22 respondents, or 47 percent; χ2=21.55, df=1, p<.001). Because of the presence of multiple comparisons, these findings should be interpreted with caution.
Discussion
Despite the small number of community-based persons with serious mental illness who reported experience with advance care planning in this study, nearly three-quarters (72 percent) believed that someone should be designated to make health care decisions for a person who is too sick to do so, and 69 percent expressed interest in obtaining more information about formally designating a health care proxy. This substantial level of interest is similar to that seen in studies of psychiatric advance directives (22,48). For example, a recent survey of persons with schizophrenia indicated that 7 percent had a psychiatric advance directive and that 67 percent would like assistance with completing a psychiatric advanced directive (23). Unfortunately, as in the general population, mental health consumers have little experience with advance directives.
Sixty-nine percent of our sample and 76 to 78 percent of the general population have expressed interest in designating a health care proxy (38). Persons with serious mental illness differ from the general population in their preferences for health care proxy designation; only 63 percent were likely to designate a family member as their proxy, compared with 85 to 90 percent in the general population (27,38). This finding may reflect the high prevalence of unmarried individuals with serious mental illness (86 percent in this sample) as well as the potential for estrangement from family members in this population (49,50). With regard to proxy decision making and end-of-life issues, HCPQ respondents and the general population are strikingly similar. Both groups are most concerned about a proxy's prolonging or terminating life support (51,52), and they both prioritize emotional and financial burden on family, pain and suffering, and saying "goodbye" to friends and family (28,52,53).
Few demographic or clinical characteristics were associated with interest in advance directives and end-of-life care preferences. Women were more likely than men to endorse end-of-life treatment preferences and interest in the designation of a health care proxy. In addition, individuals who had ever been married, who had made medical visits in the previous three months, or who had worse physical health were more likely to express interest in designating a health care proxy. As noted in the general population, older age and poor physical health status were associated with the belief that someone should make a health care decision for a seriously ill person (54). Of note, attitudes toward end-of-life care were not associated with psychiatric or medical problems, educational level, guardianship status, or religious beliefs. In general, these findings suggest that the most physically impaired psychiatric patients are likely to be the most receptive to an opportunity to talk about advance directives and end-of-life care preferences.
The results of this study suggest that persons with serious mental illness are emotionally capable of engaging in medical advance care planning. Most participants understood the questions, and mental status rarely appeared to affect responses. These findings underscore an important distinction between functional capability and legal competence in making health care decisions (55,56,57,58,59). When decision-making capacity is in question, it is critical to assess relevant decision-making tasks. Persons with serious mental illness were able to consider, comfortably tolerate, and articulate preferences about medical advance directives. In most instances they identified a person who might serve as their health care proxy.
Previous reports have postulated that individuals in this population may react negatively to end-of-life discussions (31,60). However, most participants were interested in medical advance care planning and were able to complete the questionnaire. Only one-fifth of participants expressed discomfort with questions, and less than one-tenth reported interview-related stress. Our findings suggest that a semistructured interview can be effective in engaging persons with serious mental illness in advance care planning. This approach has been promoted by the Agency for Healthcare Research and Quality (55).
Mental health providers are one of several logical community resources for conducting advance care planning discussions, given that persons with mental illness are likely to obtain general medical care through linkages with community mental health care providers (61). Results of studies conducted in the general population also stress the importance of providing advance care planning opportunities in the community before people develop serious medical illnesses (62). Hospitalization of individuals with serious mental illness is associated with an exacerbation of psychiatric symptoms, making advance care planning during hospitalization difficult (63). Finally, it is possible that engaging mental health care consumers in conversations about advance directives will support their recovery and affirm autonomy, choice, and self-determination.
This study had several limitations that suggest caution in considering generalizability of our results. The study sample was drawn from one urban-suburban area and was not culturally or racially diverse, and a purposive sampling method of self-selection of participants was used. Thus the end-of-life concerns of this study sample may not be representative of ethnic minorities, other cultures, or individuals in rural settings.
Although the study group consisted of volunteers, the lack of a random sampling method did not appear to affect the representativeness of the sample with respect to the target population of community-based persons with serious mental illness. The study participants had similar demographic characteristics and mental, physical, and functional status compared with the larger Massachusetts Department of Mental Health population. Furthermore, although the sample's SF-12 physical and mental component scores were significantly different from those of the general population, the study participants had physical impairment that was comparable to that of normative medical samples and to that of a sample in a large study of persons with serious mental illness (46). The participants also had similar rates of medical comorbidity to those reported in other studies of persons with serious mental illness (48,56,64).
Given the high level of physical impairment and prevalence of medical comorbidity (60 percent) among the study participants, the study sample represents a likely priority population for implementing advance directives, thereby underscoring the significance of our findings. We did not follow the participants who indicated that they were receptive to completing an advance directive (103 participants, or 72 percent) to determine the frequency with which receptivity converted into a completed advance care plan. This information would have important implications for the advance care planning utility of a semistructured interview such as the HCPQ. Finally, this study was based on data collected during 2000 to 2001. It is possible that public promotion of end-of-life care planning has increased the use of such planning by persons with serious mental illness, although we are unaware of any organized national or state efforts that would suggest significant differences from these results.
Conclusions
To our knowledge, this is the first study to explore preferences for medical advance directives among persons with serious mental illness. The results suggest feasibility and acceptability of a standardized approach to medical advance care planning in this population. Health care proxy designation and end-of-life care concerns can be ascertained through a semistructured interview conducted by mental health providers without adverse effects on participants.
Examination of medical advance directives among persons with serious mental illness is an important issue. However, knowledge in this area significantly lags behind that for the general population. Although this article presents initial findings, it is unclear whether preferences remain stable over time, which barriers impede advance care planning, or whether end-of-life treatment preferences will be implemented by health care proxies and physicians. These questions merit examination in well-designed research evaluations and will be useful in developing strategies for effectively implementing advance directives and targeting interventions that address concerns and barriers specific to this population.
Acknowledgments
This study was funded by a grant from the Robert Wood Johnson Foundation through the Promoting Excellence in End-of-Life Care Program (grant 035497). The authors thank Kristen Roy-Bujnowski, B.A., Meredith Hanrahan-Boshes, R.N., Stephen Carreras, Ph.D., Sally Neylan Okun, B.S.N., M.M.H.S., and Andrea Miller, Ed.M., M.S., for their invaluable contributions.
Dr. Foti and Dr. Fletcher are affiliated with the department of psychiatry at the University of Massachusetts Medical School. Dr. Foti is also State Medical Director of the Massachusetts Department of Mental Health in Boston. Dr. Bartels and Ms. Van Citters are with the New Hampshire-Dartmouth Psychiatric Research Center in Lebanon, New Hampshire. Dr. Bartels is also with the department of psychiatry of Dartmouth Medical School in Hanover, New Hampshire. Dr. Merriman is with the University of Miami School of Nursing and with Touchstone Consulting in Miami. Send correspondence to Dr. Foti at the Massachusetts Department of Mental Health, 25 Staniford Street, Boston, Massachusetts 02114-2503 (e-mail, [email protected]).
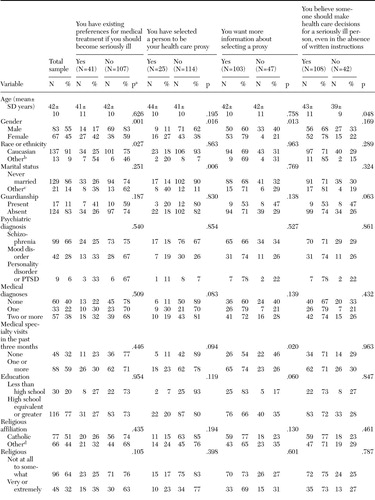 |
Table 1. Characteristics of a sample of 150 persons with severe mental illness who participated in a study of preferences regarding advance care directives
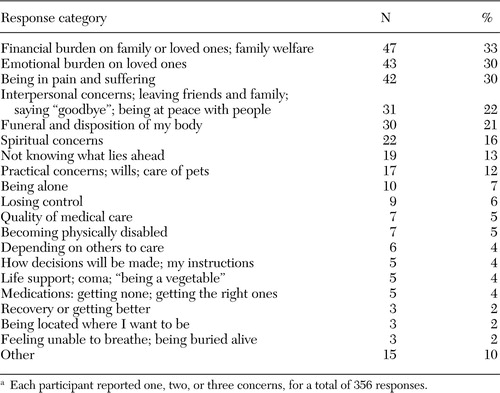 |
Table 2. End-of-life concerns reported by 142 persons with severe mental illness who completed the Health Care Preferences Questionnairea
a Each participant reported one, two, or three concerns, for a total of 356 responses.
1. Miles SH, Koepp R, Weber EP: Advance end-of-life treatment planning: a research review. Archives of Internal Medicine 156:1062–1068, 1996Crossref, Medline, Google Scholar
2. Aikman PJ, Thiel EC, Martin DK, et al: Proxy, health, and personal care preferences: implications for end-of-life care. Cambridge Quarterly of Healthcare Ethics 8:200–210, 1999Crossref, Medline, Google Scholar
3. Singer PA, Siegler M: Elective use of life-sustaining treatments in internal medicine. Advances in Internal Medicine 36:57–79, 1991Medline, Google Scholar
4. Singer PA, Martin DK, Kelner MJ: Quality end of life care: patients' perspectives. JAMA 281:163–168, 1999Crossref, Medline, Google Scholar
5. Singer PA, Martin DK, Lavery JV, et al: Reconceptualizing advance care planning from the patient's perspective. Archives of Internal Medicine 158:879–884, 1998Crossref, Medline, Google Scholar
6. Felker B, Yazel J, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356–1362, 1996Link, Google Scholar
7. Saku M, Tokudome S, Ikeda M, et al: Mortality in psychiatric patients, with a specific focus on cancer mortality associated with schizophrenia. International Journal of Epidemiology 24:366–372, 1995Crossref, Medline, Google Scholar
8. Baxter DN: The mortality experience of individuals on the Salford Psychiatric Case Register: I. all-cause mortality. British Journal of Psychiatry 168:772–779, 1996Crossref, Medline, Google Scholar
9. Mortensen PB, Juel K: Mortality and causes of death in first admitted schizophrenic patients. British Journal of Psychiatry 163:183–189, 1993Crossref, Medline, Google Scholar
10. Dixon L, Postrado L, Delahanty J, et al: The association of medical comorbidity in schizophrenia with poor physical and mental health. Journal of Nervous and Mental Disease 187:496–502, 1999Crossref, Medline, Google Scholar
11. Lambert TJ, Velakoulis D, Pantelis C: Medical comorbidity in schizophrenia. Medical Journal of Australia 178:S67-S70, 2003Google Scholar
12. Brown S, Inskip H, Barraclough B: Causes of the excess mortality of schizophrenia. British Journal of Psychiatry 177:212–217, 2000Crossref, Medline, Google Scholar
13. Osborn DP: The poor physical health of people with mental illness. Western Journal of Medicine 175:329–335, 2001Crossref, Medline, Google Scholar
14. Jeste DV, Gladsjo JA, Lindamer LA, et al: Medical comorbidity in schizophrenia. Schizophrenia Bulletin 22:413–430, 1996Crossref, Medline, Google Scholar
15. Holmberg SK, Kane C: Health and self-care practices of persons with schizophrenia. Psychiatric Services 50:827–829, 1999Link, Google Scholar
16. Druss BG, Bradford WD, Rosenheck RA, et al: Quality of medical care and excess mortality in older patients with mental disorders. Archives of General Psychiatry 58:565–572, 2001Crossref, Medline, Google Scholar
17. Lo B, McLeod GA, Saika G: Patient attitudes to discussing life-sustaining treatment. Archives of Internal Medicine 146:1613–1615, 1986Crossref, Medline, Google Scholar
18. Grisso T, Appelbaum PS: The MacArthur Treatment Competence Study: III. abilities of patients to consent to psychiatric and medical treatments. Law and Human Behavior 19:149–174, 1995Crossref, Medline, Google Scholar
19. Silberfeld M, Nash C, Singer PA: Capacity to complete an advance directive. Journal of the American Geriatrics Society 41:1141–1143, 1993Crossref, Medline, Google Scholar
20. Jones GH: Informed consent in chronic schizophrenia? British Journal of Psychiatry 167:565–568, 1995Google Scholar
21. Freedman M, Stuss DT, Gordon M: Assessment of competency: the role of neurobehavioral deficits. Annals of Internal Medicine 115:203–208, 1991Crossref, Medline, Google Scholar
22. Geller JL: The use of advance directives by persons with serious mental illness for psychiatric treatment. Psychiatric Quarterly 71:1–13, 2000Crossref, Medline, Google Scholar
23. Swanson JW, Swartz MS, Hannon MJ, et al: Psychiatric advance directives: a survey of persons with schizophrenia, family members, and treatments providers. International Journal of Forensic Mental Health 2:73–86, 2003Crossref, Google Scholar
24. Carpenter WT Jr, Gold JM, Lahti AC, et al: Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry 57:533–538, 2000Crossref, Medline, Google Scholar
25. Schwartz HI, Blank K: Shifting competency during hospitalization: a model for informed consent decisions. Hospital and Community Psychiatry 37:1256–1260, 1986Abstract, Google Scholar
26. Patient Self-Determination Act. Federal Register 60(123):33262–33294, 1990Google Scholar
27. Srebnik DS, La Fond JQ: Advance directives for mental health treatment. Psychiatric Services 50:919–925, 1999Link, Google Scholar
28. Swanson JW, Tepper MC, Backlar P, et al: Psychiatric advance directives: an alternative to coercive treatment? Psychiatry 63:160–172, 2000Google Scholar
29. Fleischner RD: Advance directives for mental health care: an analysis of state statutes. Psychology, Public Policy, and the Law 4:788–804, 1998Crossref, Medline, Google Scholar
30. Gallagher EM: Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychology, Public Policy, and the Law 4:746–787, 1998Crossref, Medline, Google Scholar
31. Swisher KN: Implementing the PSDA for psychiatric patients: a common-sense approach. Journal of Clinical Ethics 2:199–205, 1991Medline, Google Scholar
32. Backlar P, McFarland BH, Swanson JW, et al: Consumer, provider, and informal caregiver opinions on psychiatric advance directives. Administration and Policy in Mental Health 28:427–441, 2001Crossref, Medline, Google Scholar
33. Peters C, Chiverton P: Use of a values history in approaching medical advance directives with psychiatric patients. Journal of Psychosocial Nursing and Mental Health Services 41:28–36, 2003Medline, Google Scholar
34. Foti ME: "Do It Your Way": a demonstration project on end-of-life care for persons with serious mental illness. Journal of Palliative Care 6:661–669, 2003Google Scholar
35. Kaplan KO, Peres JR: Means to a Better End: A Report on Dying in America Today. Washington, DC, Last Acts, 2002Google Scholar
36. Lynn J: Measuring quality of care at the end of life: a statement of principles. Journal of the American Geriatrics Society 45:526–527, 1997Crossref, Medline, Google Scholar
37. Field MJ, Cassel CK: Approaching Death: Improving Care at the End of Life. Washington, DC, Institute of Medicine, Committee of Care at the End of Life, 1997Google Scholar
38. Emanuel LL, Barry MJ, Stoeckle JD, et al: Advance directives for medical care: a case for greater use. New England Journal of Medicine 324:889–895, 1991Crossref, Medline, Google Scholar
39. Barry JR: Investigation of reliability and validity of the Current Evaluation of Risk and Functioning (CERF-R), an assessment tool for use with adults with serious and persistent mental illness. Ph.D. dissertation. Boston, department of psychology, Northeastern University, 2001Google Scholar
40. McCorkle BH: A new measure for clinical evaluation of risk and functioning in adults with serious and persistent mental illness. Dissertation Abstracts International 59:UMI 99–11910. Boston University, 1999Google Scholar
41. Emanuel LL, Emanuel EJ: The medical directive: a new comprehensive advance care document. JAMA 261:3288–3293, 1989Crossref, Medline, Google Scholar
42. Alpert HR, Hoijtink H, Fischer GS, et al: Psychometric analysis of an advance directive. Medical Care 34:1057–1065, 1996Crossref, Medline, Google Scholar
43. Lambert P, Gibson JM, Nathanson P: The values history: an innovation in surrogate medical decision-making. Law, Medicine, and Healthcare 18:202–212, 1990Crossref, Google Scholar
44. Tyler B, Perry M, Lofton T, et al: The Quest to Die With Dignity: An Analysis of Americans' Values, Opinions, and Attitudes Concerning End-of-Life Care. Appleton, Wisc, American Health Decisions, 1997Google Scholar
45. Ware JE, Kosinski M, Keller SD: The SF-12 Users Manual: How to Score the SF-12 Physical and Mental Health Summary Scales. Boston, Quality Metric Inc, 1998Google Scholar
46. Salyers MP, Bosworth HB, Swanson JW, et al: Reliability and validity of the SF-12 health survey among people with severe mental illness. Medical Care 38:1141–1150, 2000Crossref, Medline, Google Scholar
47. Foti ME, Bartels SJ, Van Citters A, et al: End-of-life treatment preferences of persons with serious mental illness. Psychiatric Services 56:585–591, 2005Link, Google Scholar
48. Dickey B, Normand ST, Weiss RD, et al: Medical morbidity, mental illness, and substance use disorders. Psychiatric Services 53:861–867, 2002Link, Google Scholar
49. Bopp J Jr, Coleson RE: A critique of family members as proxy decision makers without legal limits. Issues in Law and Medicine 12:133–165, 1996Medline, Google Scholar
50. Pollio DE, North CS, Osborne V, et al: The impact of psychiatric diagnosis and family system relationship on problems identified by families coping with a mentally ill member. Family Process 40:199–209, 2001Crossref, Medline, Google Scholar
51. Steinhauser KE, Christakis NA, Clipp EC, et al: Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482, 2000Crossref, Medline, Google Scholar
52. Steinhauser KE, Christakis NA, Clipp EC, et al: Preparing for the end of life: preferences of patients, families, physicians, and other care providers. Journal of Pain and Symptom Management 22:727–737, 2001Crossref, Medline, Google Scholar
53. Steinhauser KE, Clipp EC, McNeilly M, et al: In search of a good death: observations of patients, families, and providers. Annals of Internal Medicine 132:825–832, 2000Crossref, Medline, Google Scholar
54. Elpern EH, Yellen SB, Burton LA: A preliminary investigation of opinions and behaviors regarding advance directives for medical care. American Journal of Critical Care 2:161–167, 1993Medline, Google Scholar
55. Kass-Bartelmes BL, Hughes R, Rutherford MK: Advance Care Planning: Preferences for Care at the End of Life. AHRQ pub 03–0018. Rockville, Md, Agency for Healthcare Research and Quality, 2003Google Scholar
56. Swartz MS, Swanson JW, Hannon MJ, et al: Regular sources of medical care among persons with severe mental illness at risk of hepatitis C infection. Psychiatric Services 54:854–859, 2003Link, Google Scholar
57. Grisso T, Appelbaum PS, Mulvey ET, et al: The MacArthur Treatment Competence Study: II. measure of abilities related to consent to psychiatric and medical treatments. Law and Human Behavior 19:127–148, 1995Crossref, Medline, Google Scholar
58. Applebaum PS, Grisso T: The MacArthur treatment competence study: I. mental illness and competence to consent to treatment. Law and Human Behavior 19:105–126, 1995Crossref, Medline, Google Scholar
59. Sales GN: The health care proxy for mental illness: can it work and should we want it to? Bulletin of the American Academy of Psychiatry and the Law 21:161–179, 1993Google Scholar
60. Lee MA, Ganzini L, Heintz R: The PSDA and treatment refusal by a depressed older patient committed to the state mental hospital. HEC Forum 5:289–301, 1993Crossref, Medline, Google Scholar
61. Schwab B, Drake RE, Burghardt EM: Health care of the chronically mentally ill: the culture broker model. Community Mental Health Journal 24:174–184, 1988Crossref, Medline, Google Scholar
62. Pfeifer MP, Mitchell CK, Chamberlain L: The value of disease severity in predicting patient readiness to address end-of-life issues. Archives of Internal Medicine 163:609–612, 2003Crossref, Medline, Google Scholar
63. Loewy EH: Ethical considerations in executing and implementing advance directives. Archives of Internal Medicine 158:321–324, 1998Crossref, Medline, Google Scholar
64. Sokal J, Messias E, Dickerson FB, et al: Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Disease 192:421–427, 2004Crossref, Medline, Google Scholar



