Age-Related Modifiers of Clinical Presentation and Health Service Use Among Veterans With Bipolar Disorder
Abstract
OBJECTIVE: This retrospective analysis of a large Department of Veterans Affairs (VA) database evaluated differences in clinical presentation, health service use, and use of psychotropic medications between older and younger adults with bipolar disorder. METHODS: The results presented in this article focus on veterans with bipolar disorder who were active in the VA's National Psychosis Registry in federal fiscal year 2001 (FY01). RESULTS: The registry listed 65,556 individuals as having bipolar disorder in FY01. In FY01, nearly 25 percent of veterans with bipolar disorder (more than 16,000 individuals) were aged 60 years or older, and more than 10 percent were aged 70 years or older. Elderly persons were hospitalized at similar or slightly lower rates than middle-aged persons but tended to have longer hospital stays. Use of outpatient services was also higher in older populations. Patterns of use of psychotropic medications indicated that valproate is the most commonly used mood-stabilizing agent in the VA, in use by 72.9 percent of patients who receive a mood stabilizer. Use of lithium is substantial as well, with more than 40 percent of patients taking this agent. In addition, just over 40 percent of all veterans with bipolar disorder receive antipsychotic medication. CONCLUSIONS: Bipolar disorder affects large numbers of veterans across the entire life span, and use of VA resources by this population becomes greater with advancing age. Data from this study provide new information about the unique treatment requirements and clinical presentations of older patients with bipolar disorder.
Bipolar disorder is a serious, chronic, and debilitating mental illness that has been reported to affect approximately .4 to 1.6 percent of the U.S. population—an estimated 1 million to 3.5 million persons (1,2,3). Fortunately, our ability to treat bipolar disorder has grown dramatically in the past decade as a result of enhanced awareness of the disorder by the medical community, better identification of individuals with bipolar disorder, and rapid proliferation of effective drug treatments (4,5). A number of treatment guidelines for bipolar disorder currently exist (4,5,6,7). Such guidelines have been designed to provide clinicians with information about best treatments with respect to a variety of illness modifiers, including severity of illness, illness polarity, and treatment setting.
Despite the comprehensiveness of current guidelines, there remains a scarcity of evidence-based recommendations that clearly and specifically address treatment requirements and unique clinical presentations seen among older adults with bipolar illness (5,8). This circumstance is likely due to a variety of factors, including the dearth of treatment data for late-life bipolar illness and lack of large-scale and longitudinal assessments of bipolar illness across the life span (9,10).
This deficit in knowledge has become increasingly problematic given the aging of our population and the extensive service needs of older adults with serious mental illness. In patients over the age of 65 years, prevalence rates of bipolar disorder range from .1 to .4 percent, and 5 to 12 percent of geriatric psychiatry admissions involve persons with bipolar disorder (11). Mania and depression appear to be equally common among geriatric patients hospitalized with acute bipolar relapse (12). Providers who deliver care to older adults with bipolar disorder are not well supported with respect to literature-based consensus on optimal treatments, treatment settings, and service use expectations for older adults with bipolar disorder (8,13,14,15). There is a critical need for a better understanding of how health care needs of persons with bipolar disorder may change across the life span and how presentation of the illness may differ in elderly compared with younger populations (16).
This retrospective analysis of a large Department of Veterans Affairs (VA) database evaluated selected differences in clinical presentation, use of health care services, and use of psychotropic medications between older and younger adults with bipolar disorder. We hypothesized that older adults with bipolar disorder would constitute a substantial number of all individuals in the database and that these patients would frequently present with both bipolar mania and bipolar depression complicated by substantial comorbidity. We hypothesized that, compared with younger persons, older adults would have more frequent hospital admissions and longer hospital stays and would use more nonpsychiatric outpatient services.
Methods
The database from which the study results are derived was developed by the Serious Mental Illness Treatment Research and Evaluation Center (SMITREC) at the recommendation of the VA committee on care of severely chronically mentally ill veterans in 1998. This database—the National Psychosis Registry—is an ongoing registry of all veterans with a diagnosis of serious mental illness, including those with psychosis (schizophrenia, schizoaffective disorder, and other nonorganic psychosis) as well as bipolar disorder who have received VA services from 1988 to the present. Thus the registry consists of records for all patients who received a diagnosis of psychosis or bipolar disorder during inpatient stays for federal fiscal year 1988 (FY88) to fiscal year 2002 (FY02) and during outpatient visits for FY97 to FY02.
Registry patients were identified by using data obtained from the VA Patient Treatment File, census data files, and Outpatient Care Files located at the Austin Automation Center in Texas. Patients were included in the study if they had at least one qualifying diagnosis listed in the FY01 inpatient or outpatient data. A full report of the Psychosis Registry can be found on the SMITREC Web site (www.va.gov/annarbor-hsrd).
The results presented here focus on veterans with bipolar disorder who were active in the registry in FY01. First, all veterans with bipolar disorder were evaluated as a group. Then three age cohorts were identified: veterans younger than 30 years, veterans between the ages of 30 and 59 years, and veterans aged 60 years or older. The three age groups were compared on selected indexes of illness presentation (bipolar disorder type I versus type II and atypical), illness polarity at hospitalization, service use (hospitalizations, outpatient care, and substance use treatment), and psychotropic use. Bipolar I diagnoses were categorized as DSM-IV codes 296.0 (bipolar manic, single episode), 296.1 (manic disorder, recurrent episode), 296.4 (bipolar manic or hypomanic), 296.5 (bipolar I depressed), 296.6 (bipolar I mixed), or 296.7 (bipolar I unspecified). Bipolar II and not-otherwise-specified diagnoses were categorized as a DSM-IV code of 296.8. Illness polarity at hospitalization for mania includes DSM codes 296.0, 296.1 (manic disorder, recurrent episode), 296.4, and 296.6 and for depression includes DSM code 296.5.
Statistical significance for differences across the three age cohorts for the measures presented in this study was tested by using chi square analysis and one-way analysis of variance for unbalanced designs. Simultaneous comparisons of means for the three age cohorts were carried out post hoc by using Tukey's honestly significant differences (HSD) test at 5 percent significance level.
Results
All patients with bipolar disorder
In FY01, a total of 196,675 veterans were identified in the Psychosis Registry. Of these, 65,556 (33.3 percent) were identified as having bipolar disorder. Longitudinal comparisons of all patients with a diagnosis of bipolar disorder in FY99, FY00, and FY01 are shown in Table 1. Given the increasing number of veterans with bipolar disorder, the possibility of this observed trend's being due to case-mix changes was evaluated. Separate analysis indicated that there was general consistency by psychosis diagnosis category with the aggregate trends among all patients with psychoses or bipolar disorder.
Findings of particular interest in this sample include the relatively high rates of individuals in the "never married" and "divorced or separated" categories, the relatively high proportion of female veterans with bipolar disorder, and the relatively low proportion of African Americans. In FY01, 7 percent of all patients in the registry were women; however, women were overrepresented among veterans with bipolar disorder, 11.3 percent of whom were women. In FY01, 20.3 percent of all patients in the registry were African American; however, only 11 percent of veterans in the registry with bipolar disorder were African American.
Age distribution and demographic characteristics
A majority of veterans with bipolar disorder were between the ages of 40 and 59 years, with 29 percent (N=18,980) between the ages of 40 and 49 years and 33.1 percent (N=21,680) between the ages of 50 and 59 years. As shown in Table 2, the mean±SD age of veterans with bipolar disorder in FY01 was 52.7±12.7 years (range, 19 to 102 years). For the purposes of this study, patients were grouped into three categories: youngest cohort, below age 30 (N=1,613, or 2.5 percent); middle cohort, age 30 to 59 (N=47,613, or 72.6 percent); and oldest cohort, age 60 or older (N=16,330, or 24.9 percent). More than 10 percent of the patients with bipolar disorder (more than 8,000 patients) were aged 70 years or older. The number of veterans with bipolar disorder in the Psychosis Registry increased from 59,938 in FY99 to 65,556 in FY01—a 9.4 percent increase.
The oldest cohort of veterans were nearly exclusively male (95.5 percent, compared with 86.5 percent of male veterans with bipolar disorder aged 30 to 59 years and 71.85 percent of male veterans with bipolar disorder aged less than 30). This finding likely reflects the growing numbers of women in the active armed services. The oldest cohort also included the largest proportion of Caucasians (76 percent) and individuals who were widowed (6.2 percent). The mean age of this oldest cohort was 70.14±7.05 years (range, 60 to 102 years), compared with a mean age of 47.66±7.17 (range, 30 to 59 years) in the middle-aged cohort and a mean age of 26.13±2.53 years (range, 19 to 29 years) in the youngest cohort (Table 2).
Illness presentation across the life span
In FY01, among all patients with bipolar disorder, 55,125 (84.1 percent) had type I bipolar disorder and 10,431 (15.9 percent) had type II bipolar disorder or bipolar disorder not otherwise specified. The proportion of patients with type I versus type II or not otherwise specified illness remained fairly similar across the age cohorts, with 86 percent of the oldest cohort having type I bipolar disorder, 83.5 percent of the middle cohort having type I bipolar disorder, and 82 percent of the youngest cohort having type I bipolar disorder (Table 2).
Substance use disorder appears to be common in this VA population: 32.5 percent of all veterans with bipolar disorder who received care during FY01 had a diagnosis of substance use disorder. Analysis of substance use disorder treatment across the age spectrum suggested that veterans aged 30 to 59 years had the highest use of substance abuse treatment (a mean of 14.79±52.16 visits between FY98 and FY00, compared with 3.34±24.67 visits among veterans aged 60 years or older and 4.19±27.4 visits among veterans younger than 30 years; F=352.14, df=2, 59,533, p<.001; Tukey's HSD p<.05).
In contrast to a reduced use of services for substance use disorders with aging, the oldest cohort had the highest use of nonpsychiatric outpatient services (mean of 72.02±46.71 visits between FY98 and FY00, compared with 23.66±30.17 visits in the youngest cohort and 58.25±67.61 visits in the cohort of veterans aged 30 to 59 years; F=372.70, df=2, 59,533, p<.001; Tukey's HSD p<.05).
Use of health care services
Hospitalization.Table 3 illustrates illness polarity at hospital admission and use of hospital resources by veterans with bipolar disorder in the period FY98 to FY00. A majority of persons with bipolar disorder (38,357, or 58.1 percent) were hospitalized at some point during that period. With respect to illness polarity at time of hospital admission, no significant differences were found in the number of hospitalizations for mania or depression between the different age groups. Veterans with bipolar disorder were hospitalized slightly more often for mania than for depression (F=19.33, df=1, 10,630, p<.001), and this finding was consistent across age groups. The mean duration of hospitalization was 40.8±98 days for mania and 29±57.5 days for depression. The oldest group had significantly longer hospital stays for both mania and depression than the youngest group (mania: F=98.90, df=2, 6,316, p<.001; Tukey's HSD p<.05; depression: F=41.53, df=2, 4,179, p<.001; Tukey's HSD p<.05).
The middle and oldest cohorts had significantly more inpatient stays than the youngest cohort (F=38.6, df=2, 27,196, p<.001; Tukey's HSD p<.05). Although the middle-aged cohort had slightly more hospitalizations than the oldest cohort, the oldest cohort, once hospitalized, had significantly longer hospital stays than younger patients—nearly three times as long, on average, as patients under the age of 30 (F=202.21, df=2, 27,196, p<.001; Tukey's HSD p<.05).
Use of outpatient services. In addition to hospital use, veterans with bipolar disorder were substantial consumers of VA outpatient health care services. Table 3 illustrates use of outpatient clinic services by age cohort during the period FY98 to FY00. Veterans in the middle-aged and older cohorts had more than twice the number of outpatient visits as those in the youngest cohort, with the oldest cohort having slightly fewer visits than the middle cohort. Services included nonpsychiatric clinic visits (including medical care), psychiatric clinic visits, VA homeless services, outpatient services for treatment of posttraumatic stress disorder, substance abuse clinic services, psychiatric day treatment, and psychiatric vocational clinic visits. Although the oldest cohort had a similar number of outpatient visits to the middle-aged cohort, the older cohort had more visits for nonpsychiatric outpatient care and fewer visits for substance abuse treatment (F=352.14, df=2, 59,533, p<.001; Tukey's HSD p<.05).
Use of psychotropic medications. Information was available on use of lithium and anticonvulsant drugs as well as conventional and atypical antipsychotic drugs. Use of depot formulations of antipsychotics, ziprasodone, aripiprazole and lamotrigine is not included here. The only anticonvulsants included here are valproate and carbamazepine. Table 4 illustrates use of lithium and anticonvulsant medications among veterans with bipolar disorder in the VA system, including overall use patterns for each agent as well as identification of use of multiple agents. Psychotropic use patterns in the registry demonstrate that mood-stabilizing medications (lithium, carbamazepine, and valproate) are prescribed for 61.8 percent of veterans with bipolar disorder, with valproate being the most commonly used mood stabilizer (24,700 individuals, or 61 percent of all patients taking mood stabilizers). By comparison, lithium was used by 16,404 individuals (40.5 percent of patients taking mood stabilizers), and carbamazepine was used by 4,911 individuals (12.1 percent of patients taking mood stabilizers). Lithium was used by 44.1 percent of veterans aged 60 or older, and valproate was used by 55.9 percent of veterans aged 60 or older. More than one mood-stabilizing medication was prescribed for more than 13 percent of patients.
Table 5 illustrates use of antipsychotic medications among veterans with bipolar disorder in the VA system, including percentages of patients taking any oral antipsychotic medication, percentages of patients taking only conventional antipsychotic medications, any use of atypical antipsychotics, and concurrent use of two or more antipsychotics for all three age cohorts. The atypical antipsychotic category comprised clozapine, olanzapine, quetiapine, and risperidone. Among all veterans with bipolar disorder, more than 40 percent had antipsychotic medications prescribed in FY01; the great majority of veterans for whom antipsychotics were prescribed received atypical antipsychotics (85.5 percent).
Olanzapine was the most commonly used of all the atypical agents: nearly half of veterans with bipolar disorder who received any antipsychotic (12,996, or 48.6 percent) received olanzapine. Although olanzapine was used slightly more often in the youngest cohort, 48.9 percent of middle-aged veterans and 47.1 percent of veterans aged 60 and over for whom any type of antipsychotic was prescribed were receiving olanzapine (χ2=11.5, df=2, p=.0052). Risperidone was the second most utilized antipsychotic for bipolar disorder (approximately 33.6 percent of veterans for whom any antipsychotic was prescribed), whereas quetiapine was used by 17.3 percent of veterans on any antipsychotic and clozapine was rarely used (less than 1 percent of veterans).
Discussion
Analysis of this large VA patient database suggests that bipolar disorder affects large numbers of veterans across the entire life span and that use of VA resources by these individuals increases with advancing age. In addition, a growing number of persons with bipolar disorder are included in the VA Psychosis Registry. In FY01 a total of 65,556 individuals with bipolar disorder were identified by the registry, an increase of 9.4 percent from FY99. This increase presents a tremendous institutional responsibility and challenge, reflected in the $3,082,525,805 spent by the VA for psychiatric care for patients with psychosis or bipolar disorder in FY01 (17).
In FY01, nearly 25 percent of veterans with bipolar disorder (more than 16,000 individuals) were aged 60 years or older, and more than 10 percent were aged 70 years or older. The largest group of veterans with bipolar disorder comprised individuals between the ages of 50 and 59. Thus a projection of care needs for this population might be determined over the next decade on the basis of patterns seen in somewhat older age cohorts. In the general population, there is also a growing proportion of older adults as a result of increased longevity and lower birth rates (18). Thus findings from this VA population may be useful in better understanding illness presentation and care needs associated with aging among persons with bipolar disorder.
With respect to illness presentation, it appears that bipolar type remains fairly constant across the life span. By definition, once an individual receives a diagnosis of type I bipolar disorder, he or she will not "convert" to a type II diagnosis even if the person is no longer experiencing full- blown mania. However, approximately 14 percent of persons aged 60 years or older will have the type II variant of bipolar disorder with hypomanic episodes alternating with depressive episodes or bipolar disorder not otherwise specified. It must be noted that the diagnoses in this data set were clinical claims data rather than diagnoses established via rigorous research interviews or research criteria.
In the VA system over the next decades, women and non-Caucasians will be increasingly represented among individuals with bipolar disorder. A limitation of this data set is the overwhelmingly male subsample, which may have implications in the generalizability of the data, particularly with respect to mood polarity and comorbid substance abuse. The relatively low numbers of African Americans with a diagnosis of bipolar disorder is consistent with the findings of other studies in which lower rates of mood disorder diagnoses and higher rates of psychotic disorder diagnoses were found among African Americans compared with whites (19,20). Racial differences in rates of mood disorders may be due to both provider factors, such as misdiagnosis (21), and patient factors, such as the selective use of mental health care services for different disorders between races (22).
The findings of this study suggest that bipolar disorder among older adults does not "burn out" over time and that use of health care resources continues to be substantial among older adults with bipolar disorder at and beyond the seventh decade of life. Although theoretically possible, it is unlikely that older veterans with bipolar disorder are being "dropped" from the registry as they age. Integration between medical and psychiatric systems in the VA is relatively good—as opposed to the common scenario in community settings, where medical and psychiatric care are often delivered within entirely separate care systems—and having a single payer and a single care provider facilitates inclusion of all patients regardless of where care is received within the VA network.
Overall, middle-aged and older veterans with bipolar disorder had more hospital admissions than persons under the age of 30. Across all age groups, patients were hospitalized slightly more often for mania than for depression (F=19.33, df=1, 10,630, p<.001). Although elderly persons may be hospitalized at similar or slightly lower rates than middle-aged individuals, it can be expected that they will have longer hospital stays, possibly because of increased rates of comorbid medical illness associated with late-life bipolar disorder. Use of outpatient services in the study reported here followed a similar pattern, with increased use in older populations, although outpatient service use by the elderly was similar or slightly lower than that of middle-aged patients.
Other investigators have also noted the continued high use of resources in late-life bipolar disorder. Bartels and colleagues (23) reported that elderly persons with bipolar disorder had greater severity of symptoms and impairment of community living skills, using almost four times the total amount of mental health services, and were four times as likely to be hospitalized as older adults with unipolar depression. This finding may be a product of greater medical comorbidity (3), comorbid dementia (24), less robust response to treatment (8) or more adverse effects associated with medication treatment (25), or aging-related psychosocial issues (8).
The proportion of veterans with bipolar disorder who had a substance use disorder in FY01 was more than 32 percent in the VA Psychosis Registry, although the fact that identification of substance use disorder in this study was retrospective and based on service use is likely to result in underreporting of substance abuse in this population. Veterans with bipolar disorder appear to use substance abuse treatment services fairly extensively. Absolute numbers of clinic visits for substance abuse treatment are highest for veterans aged 30 to 59 years, although, in the youngest cohort, substance abuse treatment visits made up approximately 10 percent of total outpatient visits. Thus it appears that propensity to abuse substances may be a more substantial problem for younger and middle-aged veterans with bipolar disorder and may lessen over time for elderly veterans with bipolar disorder. Alternatively, the data may reflect a generational cohort effect—the baby-boomer generation would be included primarily in this middle-aged group. It has been suggested that these baby boomers may have higher rates of substance use disorders than generations born earlier (26), and it is not clear how substance use patterns may evolve among these individuals over time.
As expected, nonpsychiatric outpatient visits, which include medical or primary care visits, increased with age among veterans with bipolar disorder, with elderly veterans using the greatest amount of outpatient nonpsychiatric services. This finding has extremely important clinical implications for provision of services to older adults with bipolar disorder in the VA system. Medical illness is likely to complicate outcome and generate a greater need for both inpatient and outpatient services and may affect the efficacy and tolerability of psychotropic medications. The findings from this analysis suggest that aging affects outcomes among patients with bipolar disorder. Although the database does not allow for assessment of clinical response to mental health or medical care among veterans in the registry, it is likely that older adults with bipolar disorder and medical illness respond less well and have more adverse effects associated with treatments that typically are effective and well tolerated in younger populations. Integration of medical and psychiatric care is important in optimizing outcomes for older patients, and this issue needs to be addressed in the near future in order to provide appropriate care for this aging population of veterans.
It has been reported that anticonvulsant drugs, such as valproate, have surpassed lithium in popularity in some settings (13). Likewise, in the VA setting, valproate is the number-one mood stabilizer prescribed for bipolar disorder. Despite the fact that some reports suggest that lithium may be poorly tolerated by older adults (27), more than 44 percent of veterans aged 60 years or more for whom mood-stabilizing medications are prescribed were taking lithium. This finding is consistent with a proposal suggesting that lithium remains the first choice for bipolar disorder among geriatric patients (28). Unfortunately, the registry does not provide information about daily dosages or serum levels, and it is not clear whether dosage adjustments are generally made with lithium for older individuals or for individuals with more comorbid medical conditions. Eastham and associates (29) noted that lithium dosage is generally 25 to 50 percent lower for older adults than for younger persons and that effective serum lithium concentrations range from .53 to .7 mmol per liter.
It must be noted that the registry information presented here is for FY01 and thus may not reflect the most current utilization practices. This observation may be important given the growing popularity of additional novel anticonvulsants such as lamotrigine and oxcarbazepine in the management of bipolar disorder in many clinical settings. In addition, medication patterns in this data set are based on filled prescriptions, this might be affected by both adherence with clinic visits as well as compliance with pharmacy follow-up or calls to request medication refills.
Just over 40 percent of veterans with bipolar disorder (N=26,730) received some type of antipsychotic agent, largely atypical compounds. Olanzapine, which was the first atypical antipsychotic approved by the Food and Drug Administration (FDA) for the treatment of bipolar disorder, was the most prescribed atypical antipsychotic among persons with bipolar disorder, and clozapine was very rarely prescribed for bipolar disorder in the VA (less than 1 percent of patients). Patterns of use for each atypical antipsychotic were similar across the age spectrum. The agents that were most commonly prescribed for bipolar disorder in the VA Psychosis Registry in FY01 were lithium (25.9 percent of all veterans with bipolar disorder), olanzapine (19.8 percent), risperidone (13.7 percent), carbamazepine (7.5 percent), quetiapine (7.1 percent), and valproate (5.3 percent).
Atypical antipsychotics are a promising addition to the psychopharmacologic armamentarium for treatment of mood disorders. Olanzapine, risperidone, and quetiapine currently have FDA approval for the treatment of bipolar disorder. Olanzapine, risperidone, quetiapine, and aripiprazole have been found to be effective and safe for the treatment of bipolar disorder as monotherapy or adjunct therapy among adults in controlled double-blind studies (30). However, published, controlled studies of the use of atypical antipsychotics in geriatric mania and geriatric bipolar depression are still needed to establish the effectiveness of these agents among elderly patients with bipolar disorder (8).
Conclusions
Veterans with bipolar disorder constitute a large and growing proportion of adults with psychotic illnesses in the VA system. In order for the VA to provide appropriate services for these individuals, a good understanding of illness presentation and service needs for aging veterans with bipolar disorder is essential. The published literature on bipolar disorder among older persons has been limited, with gaps in knowledge in multiple areas, including illness presentation, outcome, and specific treatment needs. Patterns of illness manifestation and health service use from this large VA registry may assist in improving our understanding of how late-life bipolar disorder may present in both VA and non-VA populations.
Dr. Sajatovic is associate professor of psychiatry at Case Western Reserve University School of Medicine in Cleveland, Ohio. Dr. Blow is director of the Serious Mental Illness Treatment Research and Evaluation Center (SMITREC) of the Ann Arbor Department of Veterans Affairs Healthcare System and associate professor and research associate professor of psychiatry at the University of Michigan in Ann Arbor. Ms. Ignacio is senior research associate at SMITREC in Ann Arbor. Dr. Kales is assistant professor of psychiatry in the section of geriatric psychiatry at the University of Michigan in Ann Arbor and director of the geriatric psychiatry clinic of the Department of Veterans Affairs in Ann Arbor. Send correspondence to Dr. Sajatovic at the Department of Psychiatry, University Hospitals of Cleveland, 11100 Euclid Avenue, Cleveland, Ohio 44106 (e-mail, [email protected].)
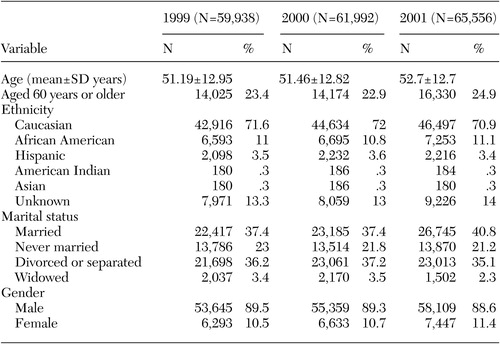 |
Table 1. Demographic characteristics of all veterans with bipolar disorder receiving services from the Department of Veterans Affairs, federal fiscal years 1999 through 2001
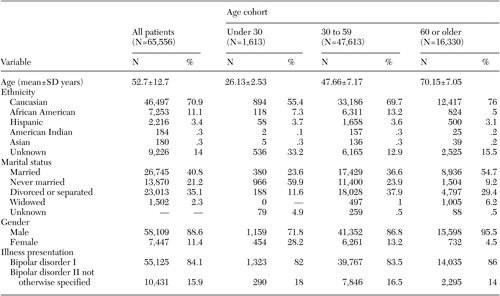 |
Table 2. Demographic and clinical characteristics of all veterans with bipolar disorder in federal fiscal year 2001, by age cohort
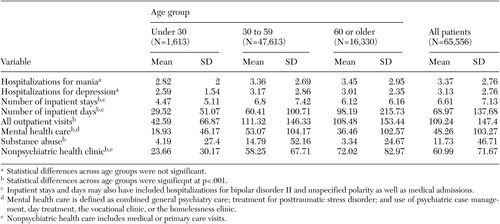 |
Table 3. Illness polarity at hospitalization and use of hospital and outpatient services during federal fiscal years 1998 through 2000 by veterans who had bipolar disorder in fiscal year 2001
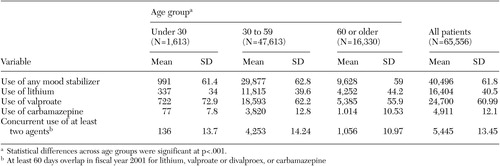 |
Table 4. Use of lithium and anticonvulsants among veterans who had bipolar disorder in federal fiscal year 2001
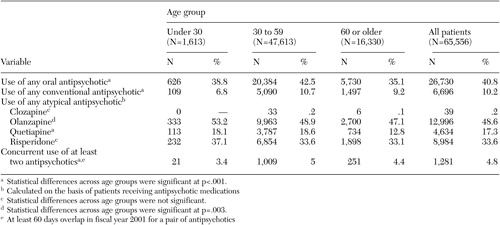 |
Table 5. Use of antipsychotic medications among veterans who had bipolar disorder in federal fiscal year 2001
1. Regier DA, Myers JK, Kramer M, et al: The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Archives of General Psychiatry 41:934–941, 1984Crossref, Medline, Google Scholar
2. Bourdon KH, Rae DS, Locke BZ, et al: Estimating the prevalence of mental disorders in US adults from the Epidemiologic Catchment Area Survey. Public Health Reports 107:663–668, 1992Medline, Google Scholar
3. Evans DL: Bipolar disorder: diagnostic challenges and treatment considerations. Journal of Clinical Psychiatry 61(suppl 13):26–31, 2000Google Scholar
4. American Psychiatric Association: Practice guideline for the treatment of patients with bipolar disorder (revision). American Journal of Psychiatry 159(suppl 4):1–50, 2002Google Scholar
5. Goodwin GM and the Consensus Group of the British Association for Psychopharmacology: Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology 17:149–173, 2003Crossref, Medline, Google Scholar
6. Bauer MS, Callahan AM, Jampala C, et al: Clinical practice guideline for bipolar disorder from the Department of Veterans Affairs. Journal of Clinical Psychiatry 60:9–21, 1999Crossref, Medline, Google Scholar
7. Sachs GS, Printz DJ, Kahn DA, et al: The Expert Consensus Guideline Series: medication treatment of bipolar disorder 2000. Postgraduate Medicine 1:1–104, 2000Google Scholar
8. Sajatovic M: Aging-related issues in bipolar disorder: a health services perspective. Journal of Geriatric Psychiatry and Neurology 15:128–133, 2002Crossref, Medline, Google Scholar
9. Colenda CC: Mania in late life. Geriatrics 57:50–54, 2002Medline, Google Scholar
10. Snowdon J: The relevance of guidelines for treatment of mania in old age. International Journal of Geriatric Psychiatry 15:779–783, 2000Crossref, Medline, Google Scholar
11. Van Gerpen MW, Johnson JE, Winstead DK: Mania in the geriatric patient population. American Journal of Geriatric Psychiatry 7:188–202, 1999Crossref, Medline, Google Scholar
12. Sajatovic M: Late-life bipolar disorder: early- vs late-onset illness. Presented at the annual meeting of the American Psychiatric Association, San Francisco, May 17–22, 2003Google Scholar
13. Shulman KI, Rochon P, Suykora K, et al: Changing prescription patterns for lithium and valproic acid in old age: shifting practice without evidence. British Medical Journal 326:960–961, 2003Crossref, Medline, Google Scholar
14. McDonald WM: Epidemiology, etiology, and treatment of geriatric mania. Journal of Clinical Psychiatry 61(suppl 13):3–11, 2000Google Scholar
15. Young RD, Klerman GL: Mania in late life: focus on age of onset. American Journal of Psychiatry 49:867–876, 1992Google Scholar
16. Charney DS, Reynolds DF, Lebowitz BL, et al: Depression and bipolar support alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Archives of General Psychiatry 60:664–672, 2003Crossref, Medline, Google Scholar
17. Blow FC, Valenstein M, McCarthy J, et al: Care for Veterans with Psychosis in the VHA, FY01:3rd Annual National Psychosis Registry Report to the Department of Veterans Affairs. Washington, DC, 2002Google Scholar
18. Administration on Aging: A Profile of Older Americans:2001. Available at www.aoa.gov/prof/statistics/profile/profiles2002.aspGoogle Scholar
19. Minsky S, Vega W, Miskimen T, et al: Diagnostic patterns in Latino, African American, and European American psychiatric patients. Archives of General Psychiatry 60:637–644, 2003Crossref, Medline, Google Scholar
20. Kales HC, Blow FC, Bingham CR, et al: Race and inpatient psychiatric diagnoses among elderly veterans. Psychiatric Services 51:795–800, 2000Link, Google Scholar
21. Neighbors HW, Jackson JS: The use of informal and formal help: four patterns of illness behavior in the black community. American Journal of Community Psychology 12:629–644, 1984Crossref, Medline, Google Scholar
22. Neighbors HW, Trierweiler SJ, Ford BC, et al: Racial differences in DSM diagnosis using a semi-structured instrument: the importance of clinical judgment in the diagnosis of African Americans. Journal of Health and Social Behavior 44:237–256, 2003Crossref, Medline, Google Scholar
23. Bartels SJ, Forester B, Miles KM, et al: Mental health service use by elderly patients with bipolar disorder and unipolar major depression. American Journal of Geriatric Psychiatry 8:160–166, 2000Crossref, Medline, Google Scholar
24. Dhingra U, Rabins PV: Mania in the elderly: a five-to-seven year follow-up. Journal of the American Geriatrics Society 39:581–583, 1991Crossref, Medline, Google Scholar
25. Tueth MJ, Murphy TK, Evans KL: Special considerations: use of lithium in children, adolescents, and elderly populations. Journal of Clinical Psychiatry 5:29–33, 1993Crossref, Google Scholar
26. Patterson TL, Jeste DV: The potential impact of the baby-boom generation on substance abuse among elderly persons. Psychiatric Services 50:1184–1188, 1999Link, Google Scholar
27. Sproule BA, Hardy BG, Shulman KI: Differential pharmacokinetics of lithium in elderly patients. Drugs and Aging 16:165–177, 2000Crossref, Medline, Google Scholar
28. Oshima A, Higuchi T: Treatment guidelines for geriatric mood disorders. Psychiatry and Clinical Neuroscience 53(suppl):S55–59, 1999Google Scholar
29. Eastham JH, Jeste DV, Young RC: Assessment and treatment of bipolar disorder in the elderly. Drugs and Aging 12:205–224, 1998Crossref, Medline, Google Scholar
30. Hirschfeld RMA: The efficacy of atypical antipsychotics in bipolar disorders. Journal of Clinical Psychiatry 64(suppl 8):15–21, 2003Medline, Google Scholar



