Current Trends in Outpatient Pharmacy in VA Specialized Mental Health Treatment
Abstract
This report examines current trends in specialized mental health care in the U.S. Department of Veterans Affairs (VA). Over the period 1999 to 2002, inpatient bed-days declined steadily, and the number of outpatient visits increased. Outpatient pharmacy spending increased by nearly 19 percent per year, whereas spending for inpatient, residential, and outpatient nonpharmacy services increased by less than 1.5 percent per year. Total per capita spending declined from $3,262 to $3,061 as the number of patients served increased faster than did total spending. These trends most likely reflect VA policy changes and the impact of new psychiatric medications.
Heffler and colleagues (1) predict double-digit rates of growth in spending for all prescription drugs throughout this decade. Will mental health pharmacy follow the same trend? There is less consumer advertising for mental health medications than for physical conditions, such as arthritis and high cholesterol levels. In addition, because mental illnesses typically present earlier in life, the aging of the population does not tend to increase the prevalence of such illness. However, mental health pharmacy may expand if manufacturers release powerful new medications at the rate that was seen in the 1990s.
We assessed current mental health trends in the Department of Veterans Affairs (VA) health care system over the period 1999 to 2002. The VA system, which serves former military personnel and certain dependents, is ideal for the study of mental health care trends, because it has no limitations on mental health care and provides prescription drugs with at most a small copayment. Chen and colleagues (2) described broad trends in VA mental health treatment expenditures over the period 1995 to 2001. In this report we provide more recent data and break down outpatient pharmacy spending into major classes. We compare annual rates of change across drug classes and between drugs and other forms of mental health treatment.
Methods
Specialized mental health care provided by the VA is recorded in VA service use databases. We extracted all records pertaining to inpatient, outpatient, and residential care. Substance abuse care was excluded. Inpatient programs were defined as specialized mental health units in which patients received treatment of more than 24 hours' duration. Residential treatment refers to specialized domiciliary and residential rehabilitation programs. Residential programs have an inpatient component but are staffed less intensively than are standard inpatient wards.
Costs were derived primarily from the annual VA Cost Distribution Report (CDR), which attributes spending to individual clinics and departments on the basis of workload data. Pharmacy costs for residential and inpatient care are factored into the CDR cost figures and cannot be separated out. Because outpatient care costs in the CDR exclude costs for prescription drugs, we derived outpatient pharmacy spending by year and drug class from the PBM V3.0 database, which is a record of prescriptions filled by VA pharmacies. The data were limited to the most common classes of psychiatric drugs: antipsychotics, antidepressants, anxiolytics and sedatives-hypnotics, and lithium. Smaller drug classes, such as anticonvulsants and anticholinergics, were omitted because of their frequent use for nonpsychiatric illnesses.
We calculated total spending and spending growth rates separately for the three drug classes and for the three settings of care—inpatient, residential, and nonpharmacy outpatient. Service use rates were measured by counting individual patients served and the number of days (inpatient and residential) or on the basis of clinic codes (outpatient).
Results
The results of our analysis are summarized in Table 1. Over the period 1999 to 2002, the proportion of specialized mental health spending attributable to pharmacy increased from 13 percent to nearly 19 percent. We observed moderate growth in total expenditures over time, reflecting both double-digit growth in outpatient pharmacy spending and very slow growth in other services. Inpatient care declined steadily over the study period, whereas residential and outpatient services increased. Total spending per VA patient receiving specialized mental health care declined at a moderate pace.
Pharmacy payments increased sharply each year. Nearly all growth in the use of pharmaceuticals was due to newer antipsychotics and newer antidepressants, which had average annual growth rates of 18.7 percent and 15.7 percent, respectively. The VA has traditionally spent considerably more on antidepressants than on antipsychotics, but at current rates the newer antipsychotics are expected to become the largest single class of psychiatric medications in the VA in fiscal year 2003.
Significant changes were also observed in the use of nonpharmacy services. Inpatient days declined by 8 to 12 percent each year. The number of outpatient visits—the largest category—increased by an average of 1.8 percent per year. The much smaller category of residential care declined sharply in 2000 before rebounding in 2001 and 2002. These trends most likely reflect a VA management plan, dating to the late 1990s, intended to close many inpatient beds in favor of less intensive residential and outpatient services (3). Similar results have been found for VA substance abuse care (4).
Discussion
Inflation of the cost per dose does not appear to have driven the increases in expenditures on antidepressants or antipsychotics. Dobscha and associates (5) documented acquisition costs for selective serotonin reuptake inhibitors (SSRIs) paid by the Portland (Oregon) VA Medical Center at four points during the period January 1999 through November 2001. The per-pill cost of five SSRIs either declined or increased by less than 5 percent over that time. Prices at other VA facilities would have been very similar, given the existence of national purchasing contracts. We did a similar check for antipsychotic drug prices in the VA National Formulary. Of the five newer antipsychotics, three kept the same price or had a slight decrease over that of the previous year, and two had a cost increase of 2.5 percent or less. On this basis, we tentatively conclude that inflation was not responsible for the high growth rates we observed in outpatient pharmacy spending.
The swift increase in VA spending on antipsychotics has prompted several reactions, including a study by the General Accounting Office (GAO), administrative reviews for selected antipsychotics, and an agencywide prescribing guideline (6). Analyzing the GAO data, Rosenheck and Leslie (6) found evidence that the nondirective administrative reviews affect prescribing practices, which may lead to moderate cost savings.
An important driver of antipsychotic spending is the trend toward polypharmacy, or the prescribing of multiple medications for a single condition (7,8). Even if the number of prescriptions per person had stayed constant over the study period, drug spending would have increased, because existing patients had their medications switched to more costly brand-name medications. Likewise, new patients are likely to start therapy with brand-name medications rather than generic drugs. This practice will lead to higher expenditures per person as long-term patients who are stabilized on less expensive older medications die and are replaced in the system by newer patients who use a more costly mix of medications. A third factor is advertising. Manufacturers are marketing antipsychotics for illnesses other than schizophrenia, such as bipolar disorder and senile dementia.
The results of this study should be interpreted in light of several limitations. Although the CDR reconciles with the VA general ledger, allocations in the CDR are sometimes missing or inaccurate (9). Second, some spending for inpatient and residential care pertains to physical rather than mental health conditions. Finally, we underestimated mental health pharmacy spending by omitting anticonvulsants and medications for treating the side effects of antipsychotics that are used for both mental and physical conditions.
Conclusions
The growth in specialized mental health spending attributable to pharmacy over the period 1999 to 2002 was driven by double-digit annual increases in spending for newer antidepressants and antipsychotics. Under current trends, the class of newer antipsychotics is expected to soon account for the greatest share of outpatient pharmacy spending for VA mental health services.
Although most drug expenditures are for treatment of physical conditions, the data presented here suggest that psychiatric drugs will follow a similar pattern of growth during this decade. However, we expect that, as the number of veterans served increases, the cost per person for mental health treatment will slowly decrease as a result of continuing reductions in inpatient spending.
Acknowledgments
The authors gratefully acknowledge the support of the VA Health Services Research and Development Service in Washington, D.C. (project SDR-ECN-99017).
The authors are affiliated with the Health Economics Resource Center of the Veterans Affairs Palo Alto Health Care System, 795 Willow Road (152 MPD), Menlo Park, California 94025 (e-mail, [email protected]).
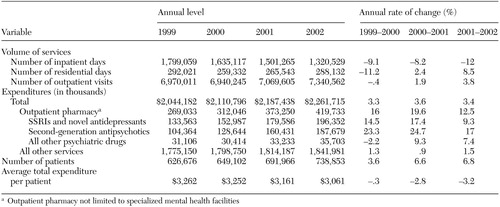 |
Table 1. Expenditures for and use of specialized mental health treatment in the Department of Veterans Affairs, 1999 to 2002
1. Heffler S, Smith S, Won G, et al: Health spending projections for 2001–2011: the latest outlook. Health Affairs 21(2):207–218, 2002Google Scholar
2. Chen S, Smith MW, Wagner TH, et al: Spending for Mental Health Treatment in the VA, 1997–2001. Health Affairs 22(6):256–263, 2003Google Scholar
3. Kizer K, Demakis J, Feussner J: Reinventing VA health care: systematizing quality improvement and quality innovation. Medical Care 38(6 suppl 1):I7-I16, 2000Google Scholar
4. Chen S, Wagner TH, Barnett PG: The effect of reforms on spending for veterans' substance abuse treatment, 1993–1999. Health Affairs 20(4):169–175, 2001Google Scholar
5. Dobscha SK, Anderson TA, Hoffman WF, et al: Strategies to decrease costs of prescribing selective serotonin reuptake inhibitors at a VA medical center. Psychiatric Services 54:195–200, 2003Link, Google Scholar
6. Rosenheck R, Leslie D: Administrative prescription review, procedures, and use of atypical antipsychotic medications in the Department of Veterans Affairs. Mental Health Services Research 5(3):149–153, 2003Google Scholar
7. Clark RE, Bartels SJ, Mellman TA, et al: Recent trends in antipsychotic combination therapy of schizophrenia and schizoaffective disorder: implications for state mental health policy. Schizophrenia Bulletin 28:75–84, 2002Crossref, Medline, Google Scholar
8. Weissman EM: Antipsychotic prescribing practices in the Veterans Healthcare Administration: New York metropolitan region. Schizophrenia Bulletin 28:31–42, 2002Crossref, Medline, Google Scholar
9. Swindle R, Beattie M, Barnett P: The quality of cost data: a caution from the VA experience. Medical Care 34 (3 suppl):MS83–90, 1996Google Scholar



