Risk Factors for Aggressive Behavior Among Psychiatric Inpatients
Abstract
The evaluation of a patient's potential for aggressive behavior is an important component of care on psychiatric units. In this study, the aggressive behavior of 111 new psychiatric inpatients in Taiwan was recorded by nursing staff using the Overt Aggression Scale (OAS) during the patients' hospitalization. Psychiatrists made diagnoses in accordance with DSM-IV criteria and collected information about psychosocial risk factors for aggression. On average, aggressive patients were hospitalized longer than nonaggressive patients. After duration of hospitalization was controlled for, it was found that patients with an earlier onset of illness were more likely to be aggressive than other patients.
The evaluation of a patient's potential for aggressive behavior is an important component of psychiatric care (1). Previous studies that have examined risk factors for aggression on psychiatric units have much relevance for Western populations but are of unproven relevance to Asian populations (2).
This study of risk factors for aggressive behavior was carried out prospectively with use of a standardized measure of aggressive behavior in a non-Western setting. Six risk factors commonly associated with inpatient violence were examined: psychiatric diagnosis, time of onset of psychiatric illness, number of hospitalizations, duration of hospitalizations, severity of psychopathology, and family history of psychiatric disorders.
Methods
The study was approved by the institutional review board of National Cheng-Kung University Hospital in Taiwan. All patients who were admitted to a locked psychiatric unit at the hospital during a seven-month period (January to July 1997) were invited to participate in the study. The refusal rate was relatively low (three patients, or 3 percent); the valid sample size was 111.
After informed consent was obtained, psychiatrists interviewed the patients and made psychiatric diagnoses based on DSM-IV criteria and Global Assessment Scale (GAS) (3) scores. In a pilot study, the interrater reliability of six psychiatrists who were involved in further data collection based on ten patients' scores on the GAS was 92 percent. Family history of psychiatric disorders was determined on the basis of the information collected by psychiatrists, social workers, and nurses. Nursing staff, who were not blinded to the study objectives, observed the study participants and filled out one Overt Aggression Scale (OAS) (4) form immediately after witnessing each aggressive behavior.
The OAS was translated into Chinese by using a two-stage procedure and was used in this study to measure three types of aggression: verbal aggression, aggression toward objects, and aggression toward other people. A pilot study was carried out beforehand to test the data collection procedure and to ensure the satisfactory reliability of all 16 nurses who would be involved in the study. On the basis of 18 aggressive episodes, the generalized kappa statistics were .66 for verbal aggression, .72 for aggression toward objects, and .61 for aggression toward other people. For the analysis reported here, we selected physical aggression toward others as the outcome variable, not only because of its importance and severity in acute psychiatric care but also because of the potential threat and actual harm to human safety.
First, chi square tests and t tests were used to compare the characteristics of patients who were physically aggressive toward others with those of patients who were not. Second, demographic variables and six risk factors were included in the multivariate logistic regression analyses to adjust for spuriousness in the prediction of physical aggression toward others. The regression results are presented as odds ratios (ORs) with 95 percent confidence intervals (CIs). A two-tailed significance level of .05 was used for statistical tests.
Results
The sample consisted of 111 patients with a mean±SD age of 38±13.8 years and a mean educational level of 9.5±3.7 years. Nearly half the patients (53 patients, or 48 percent) were women. All were Taiwan-born Chinese; 48 (43 percent) were currently married, and 50 (45 percent) had never married. A majority (82 patients, or 74 percent) had been employed for less than six months in the previous year. Fifty-three patients (48 percent) had a diagnosis of a schizophrenic disorder, and 38 (34 percent) had a diagnosis of bipolar disorder. During the current hospital stay, 46 patients (41 percent) exhibited 224 episodes of aggression toward others; 24 of these patients had just one or two episodes. The number of aggressive episodes per patient averaged 2±5.1 and ranged from zero to 37. In the first step of the analysis, patients who demonstrated physical aggression during hospitalization tended to be younger (t=−2.44, df=109, p=.02), to have a younger age at onset of their major psychiatric disorder (t=−3.21, df=109, p=.002), and to stay longer in the hospital (t=3.17, df=109, p=.002) (Table 1).
These potential risk factors for aggression, along with other demographic characteristics, were then examined by using multivariate analyses. A borderline risk or significantly elevated risk of aggression was significantly associated with a greater duration of hospitalization in days (OR=1.02, CI=1.01 to 1.04, p=.01) and an earlier onset of major psychiatric disorder (OR=.95, CI=.92 to .99, p<.01).
Discussion
We used the OAS as a measure of aggressive behavior among psychiatric inpatients to avoid some methodologic problems, such as an underestimation by chart reviewing (5). We were also able to demonstrate the cross-cultural usefulness of the OAS in Taiwan (6). However, the sample size was limited, because the intensive nature of data collection precluded enrollment of a larger sample. The selection of risk factors was based on review of the literature and consideration of feasibility—for example, we did not include patients with comorbid substance abuse or personality disorder, because these conditions were found to be uncommon among acute psychiatric inpatients in Taiwan (1,7). In addition, current adherence to psychopharmacologic treatment was excellent and did not vary among patients, likely because the primary treatment in acute psychiatric settings is medications covered by the national health care program. The nurses were responsible for the patients' medication taking around the clock, throughout the hospitalization. Thus we did not include adherence to medications as a risk factor.
The younger age at onset of psychiatric illness and the longer period of hospitalization were shown to have an association with aggressive behavior. It is interesting that the violence dynamic is similar between Western and non-Western populations. In a Western study, younger age at onset of mental illness, especially among patients with schizophrenia, was associated with aggression on long-stay psychiatric units (8).
No causal relationship can be assumed for the association between length of stay and aggression. One possible explanation for the association is that the longer the patients were in the hospital, the more time they had to commit aggressive acts, which were then captured on the OAS by the nursing staff. A second explanation is that aggression toward others was one of the indications of severe psychopathology and thus was associated with longer hospitalization (9). Alternatively, it is possible that the hospital environment leads to social breakdown that affects the behavior of institutionalized persons (10).
Since 1994, the national health care program in Taiwan has allowed patients with severe psychiatric illness to obtain health care without a copayment. However, daily reimbursements decrease as the number of days of hospitalization increases, which discourages prolonged stay on acute units. Health care providers face cost pressure to discharge patients as soon as they show a low risk of self-harm or aggression. Thus the second explanation for the association between longer hospitalization and increased aggression is more likely. Our sample might have been different from those in Western societies, where health care can be very expensive.
Conclusions
The Overt Aggression Scale may be applied to routine clinical practice and in non-Western settings. Aggressive psychiatric inpatients who were assessed with the OAS tended to stay longer on the acute ward and had an earlier onset of mental illness. Our results are still limited. Some significant associations found in this study are likely to be epiphenomena, not directly related to aggressive behavior but indicators of other variables more directly predictive. Thus it is important that a more comprehensive analysis be undertaken to identify and assess the risk of aggression among various cultural and ethnic populations.
Acknowledgments
This research was funded by grant NCKUH86-076 from National Cheng Kung University Hospital in Taiwan. The authors thank Elaine Walsh of the University of Washington in Seattle for her excellent advice and help in the preparation of the manuscript.
Dr. Chang is affiliated with Ching-Kuo Institute of Management and Health in Keelung, Taiwan. Dr. Lee is with the department of psychiatry at Lotung Pohai Hospital and College of Medicine of Fu-Jen Catholic University in Taiwan. Send correspondence to Dr. Lee at 83 Nan-Chang Street, Department of Psychiatry, Lotung Pohai Hospital, Lotung, Ilan 265, Taiwan (e-mail, [email protected]).
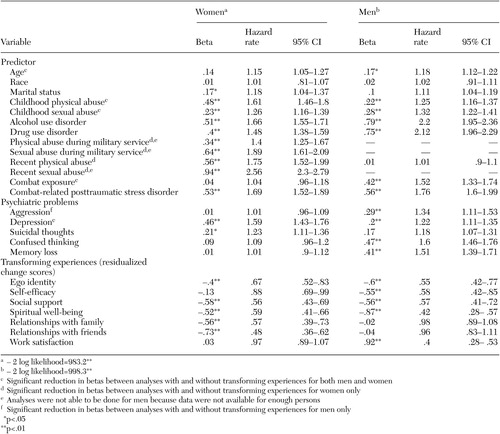 |
Table 1. Risk factors associated with aggression toward other people in a sample of 111 psychiatricinpatients
1. Lee CS, Chang CJ: Assessment of the potential for aggressive behavior in psychiatric inpatients. Taiwanese Journal of Psychiatry 13:14–22, 1999Google Scholar
2. Nijman HL, a Campo JM, Ravelli DP, et al: A tentative model of aggression on inpatient psychiatric wards. Psychiatric Services 50:832–834, 1999Link, Google Scholar
3. Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale. Archives of General Psychiatry 33:766–771, 1976Crossref, Medline, Google Scholar
4. Yudofsky SC, Silver JM, Jackson W, et al: The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry 143:35–39, 1986Link, Google Scholar
5. Apperson LJ, Mulvey EP, Lidz CW: Short-term clinical prediction of assaultive behavior: artifacts of research methods. American Journal of Psychiatry 150:1374–1379, 1993Link, Google Scholar
6. Chou KR, Lu RB, Chang M: Assaultive behavior by psychiatric in-patients and its related factors. Journal of Nursing Research 9:139–151, 2001Crossref, Google Scholar
7. Tsai SY: Outcome of bipolar disorder. Taiwanese Journal of Psychiatry 17:172–179, 2003Google Scholar
8. Rabinowitz J, Mark M: Risk factors for violence among long-stay psychiatric patients: national study. Acta Psychiatrica Scandinavica 99:341–347, 1999Crossref, Medline, Google Scholar
9. Nolan KA, Volavka J, Mohr P, et al: Psychopathy and violent behavior among patients with schizophrenia or schizoaffective disorder. Psychiatric Services 50:787–792, 1999Link, Google Scholar
10. Gruenberg EM, Kasius RV, Huxley M: Objective appraisal of deterioration in a group of long-stay hospital patients. Milbank Quarterly 40:90–100, 1962Crossref, Google Scholar



