Psychopathy and Violent Behavior Among Patients With Schizophrenia or Schizoaffective Disorder
Abstract
OBJECTIVE: Although a strong association between violence and psychopathy has been demonstrated in nonpsychotic forensic populations, the relationship between psychopathy and violence among patients with schizophrenia has not been thoroughly explored. Patients with and without a history of persistent violent behavior were compared for comorbidity of psychopathy and schizophrenia or schizoaffective disorder. METHODS: Violent and nonviolent patients were identified through reviews of hospital charts and records of arrests and convictions. The Psychopathy Checklist: Screening Version was administered to 51 patients, 26 violent patients and 25 matched nonviolent patients. Analysis of variance was used as the principal statistical method for comparing violent and nonviolent groups. RESULTS: Mean psychopathy scores were higher for violent patients than nonviolent patients. Five of the violent patients (19 percent) had scores exceeding the cutoff for psychopathy, and 13 (50 percent) scored in the possible psychopathic range. All of the nonviolent patients scored below the cutoff for possible psychopathy. Higher psychopathy scores were associated with earlier age of onset of illness and more arrests for both violent and nonviolent offenses. CONCLUSIONS: The comorbidity of schizophrenia and psychopathy was found to be higher among violent patients than among nonviolent patients. Violent patients with schizophrenia who score high on measures of psychopathy may have a personality disorder that precedes the emergence of psychotic symptoms, or they may constitute a previously unclassified subtype of schizophrenia, characterized by early symptoms of conduct disorder symptoms and persistent violent behavior.
Many persons held in correctional and forensic psychiatric facilities are psychopaths (1). Psychopathy is associated with criminality (2,3,4) and specifically with violent crime. Compared with nonpsychopathic offenders, psychopaths have more criminal charges per year spent unincarcerated and more convictions for violent crimes; they are also responsible for more violence in prisons (5). The association between violence and psychopathy has been well documented in nonpsychotic forensic populations (5,6,7,8,9).
The relative merits of the diagnosis of psychopathy (10) versus antisocial personality disorder, as it is referred to in DSM-IV, are a matter of continuing debate (11). Antisocial personality disorder is defined primarily in terms of behavior—that is, persistent violations of social norms— whereas psychopathy refers to characteristic affective and interpersonal traits as well as behaviors. Although most psychopaths would also meet the criteria for antisocial personality disorder, it is not true that most individuals with antisocial personality disorder are psychopaths.
One advantage of using the diagnosis of psychopathy in violence research rather than the DSM-IV diagnosis of antisocial personality disorder is the availability of measures of psychopathy. Other advantages have been discussed elsewhere (12). Accordingly, psychopathy was the diagnosis used in this study.
Although most patients with schizophrenia are not violent and most of the violence in the community is not attributable to schizophrenia, schizophrenia is associated with an elevated risk for violence in the community (13,14). Violence committed by persons with schizophrenia is a heterogeneous phenomenon. Violent behavior may be related to specific psychotic symptoms, such as delusions of thought insertion, thought control, and persecution (15), or to command hallucinations (16), but the link between violence and psychotic symptoms can be minimal (17). Individuals with schizophrenia may commit premeditated violent crimes that are similar in their apparent motivation to those committed by persons without mental illness (9,18).
Thus psychotic symptoms do not fully account for violence in schizophrenia. Underlying personality features may be responsible for some of the violent behavior of patients with schizophrenia. However, the prevalence of comorbidity of schizophrenia and psychopathy is not clear. The observed comorbidity may depend on the population from which subjects are selected. In general forensic patient populations, the reported overlap between psychopathy and schizophrenia or psychotic disorders is no more than 4 percent (19,20,21). In contrast, in a study of comorbidity among mentally ill subjects who showed extreme dangerousness or violence, the comorbidity of schizophrenia and psychopathy was 17 percent (22).
The primary purpose of the study reported here was to compare the comorbidity of schizophrenia and psychopathy in violent and nonviolent patients.
Methods
Subjects
Data were collected for a study (23) intended to replicate a finding of an association between ratings of risk for dangerousness and an allelic variant of the gene controlling catechol-O-methyltransferase in patients with schizophrenia (24). Subjects included men and women, age 18 years or older, with a DSM-IV diagnosis of schizophrenia or schizoaffective disorder. Due to differing allelic frequencies of the gene of interest among blacks and whites, enrollment was limited to white subjects. Potential subjects were identified by chart review.
Two groups of subjects were selected: those with and without a history of violence. Information about subjects' history of violent behavior was extracted by reviewing all available material, including admission and discharge summaries of current and previous admissions, progress notes, treatment plans, and the chart notes transcribed from the official records of arrests and convictions (RAP sheets) provided by the New York State Bureau of the Criminal Justice Services.
The minimum criterion for inclusion in the violent group was at least two documented assaults on other people. Patients whose violent acts occurred exclusively during periods of acute psychosis (for example, around the time of admission to the hospital) were not included, nor were patients who had not been violent within the preceding year. In addition, violent subjects were selected for maximal number and severity of violent behaviors in their history. Consequently, the violent subjects each had a documented history of repeated serious assaults on others occurring over several years.
Among the 26 violent subjects in the study, 22 (85 percent) had five documented assaults. Of the four subjects with fewer than five documented assaults, two had been convicted of serious violent crimes (murder and rape). A typical violent subject had a history of behavior problems, including aggressive, threatening, and assaultive behavior, dating back to adolescence or earlier; the subject also had numerous, long-term psychiatric hospitalizations during which he or she was frequently in seclusion, under close observation, or held in secure care because of assaultive behavior.
The nonviolent subjects were matched as nearly as possible to the violent subjects in gender, ethnicity (white non-Hispanic and white Hispanic), and age. These individuals had no record of physically assaulting or threatening another person and had no history of violent crime. We are aware that some of individuals in the nonviolent group might have engaged in violent acts that went unrecorded. Calling this group the comparison group instead of the nonviolent group would have been more precise but less clear.
Because psychiatrists' ratings of risk for dangerousness appear to be strongly related not only to a history of violence but also to a history of substance abuse (24), we initially excluded subjects with a history of either violent behavior or a DSM-III-R or DSM-IV diagnosis of substance abuse or dependence from the nonviolent control group. However, we subsequently discovered that the high comorbidity of substance abuse and schizophrenia and schizoaffective disorder rendered this exclusion impracticable. Thus the sample includes 25 patients with substance use disorders, six in the nonviolent group and 19 in the violent group.
Ratings
The Psychopathy Checklist: Screening Version (PCL:SV) (25) is used to assess psychopathy among persons with mental disorders (26). Each of the 12 items in the PCL:SV is rated on a 3-point scale, depending on the extent to which it applies to the individual, with 0 indicating that it does not apply. Part 1 (items 1 through 6) measures the interpersonal and affective symptoms of psychopathy, and part 2 (items 7 through 12) the social deviance symptoms.
The psychometric properties of the PCL:SV were examined in 11 samples in four settings— among correctional offenders, forensic psychiatric patients, civil psychiatric patients, and university students (25). The mean interrater reliabilities were .84 for the total score, .77 for part 1, and .82 for part 2. The weighted mean interrater reliability of the 12 items ranged from .50 to .79. The mean interrater agreement (kappa) for PCL:SV diagnosis of psychopathy was .48.
For this study, the PCL:SV was completed by a single rater who interviewed the subjects and had access to all available collateral information, including all information in the hospital chart. The nature of the information required to use the PCL:SV precluded blinding the rater to violence status. The interviews were completed between April 1996 and June 1997.
The age of onset of psychiatric symptoms was determined by chart review. In some cases the chart did not contain sufficient information to determine the age of onset. The Hollingshead Index of Social Position (27) was determined from information about educational and occupational history. The Hollingshead index has a reversed scale, so that higher scores indicate lower socioeconomic status. Full-scale IQ was estimated from scores on four subtests of the Wechsler Adult Intelligence Scale— Revised (WAIS-R) (28) according to Kaufman's algorithm (29).
Statistical analyses
To confirm the acceptability of pooling data from subjects diagnosed with schizophrenia and schizoaffective disorder, two-way analyses of variance (ANOVAs) (diagnosis by violence history) were applied to demographic variables and PCL:SV scores. In each case, no significant main effect of diagnosis or any significant interactions with diagnosis were found. The main effects of violence history were consistent with those of the pooled analyses, which are described in detail below.
One-way ANOVAs were applied to compare violent and nonviolent subjects on demographic variables as well as on total scores on the PCL:SV and, separately, on the items in parts 1 and 2 of the PCL:SV. Kruskal-Wallis analyses were used to examine the associations between individual item scores and a history of violence.
Results
The PCL:SV was administered to 51 subjects. The 26 violent subjects included 17 men and nine women. Twenty of the violent subjects had schizophrenia, and six had schizoaffective disorder. The 25 nonviolent subjects included 14 men and 11 women. Fifteen of the nonviolent subjects had schizophrenia, and ten had schizoaffective disorder. All of the violent subjects and 14 of the 25 nonviolent subjects were inpatients at the time of participation in the study. Inpatient records were available for the remaining 12 subjects. As indicated in Table 1, data were missing for some measures, such as demographic variables.
As shown in Table 1, violent subjects had significantly higher mean Hollingshead index scores (lower socioeconomic status) and more arrests than nonviolent subjects, both for violent and nonviolent offenses. However, the differences between the two groups in age, age of onset of psychiatric symptoms, and estimated IQ were not statistically significant.
Table 1 also shows that violent subjects had significantly higher total PCL:SV scores than nonviolent subjects, as well as higher scores for part 1 of the PCL:SV, which measures interpersonal and affective traits, and for part 2, which measures antisocial behaviors.
As shown in Table 2, significant correlations were found between measures of criminality and mean PCL:SV scores, including total score and scores on parts 1 and 2. A significant inverse relationship was noted between PCL total scores and part 2 scores and age of onset of psychosis.
The items from the PCL:SV are listed in Table 3. The association with history of violence was significant for all but four items of the PCL:SV— superficial, grandiose, deceitful, and lacks goals. As shown in Table 3, the first three items (superficial, grandiose, and deceitful) were not traits of many subjects in either group. In contrast, item 9, lacks goals, applied to most subjects in both groups.
Standard cutoffs (25) for the PCL:SV total score classify individuals scoring 12 or less as nonpsychopathic. Those who score 18 or higher are classified as psychopathic. Scores between 13 and 17 (inclusive) indicate possible psychopathology. Using these cutoffs, eight of the 26 violent subjects (31 percent) were classified as nonpsychopathic. Thirteen violent subjects (50 percent) were classified as possibly psychopathic. None of the nonviolent subjects scores above 12 on the PCL:SV. The frequency of the PCL:SV diagnostic categories differed between groups (p<.001, two-tailed Fisher's exact tests for a 2-by-3 contingency table).
Table 4 shows the mean PCL:SV scores of violent and nonviolent subjects with and without a history of substance abuse or dependence. A post hoc exploratory analysis of the interrelationship between violence, substance abuse or dependence, and psychopathy was also undertaken. A two-way ANOVA (violence by substance abuse) of total PCL:SV scores revealed a significant main effect of violence (F=95.34, df=1,47, p<.001), but neither the main effect of substance abuse nor the violence-by-substance abuse interaction was significant. Thus, even when violence history was taken into account, a history of substance abuse or dependence was not related to the total PCL:SV score.
Scores on parts 1 and 2 were also analyzed separately. The main effect of violence was significant on both part 1 (F=40.06, df=1,47, p<.001) and part 2 (F=52.94, df=1,47, p<.001), but the main effect of substance abuse was significant only on part 2 (F=10.22, df=1,47, p=.002). No significant violence-by-substance abuse interactions were noted. Substance abusers scored higher than those who were not substance abusers only on part 2, which measures the social deviance symptoms of psychopathy, and not on part 1, which measures interpersonal and affective symptoms.
Both substance abuse and violence contributed directly to ratings for items 11 and 12 of the PCL:SV— adolescent antisocial behavior and adult antisocial behavior, respectively. Part 2 scores were therefore recalculated to include only items 7 through 10, and the ANOVA was repeated. The main effect of violence remained significant (F=37.86, df= 1,47, p<.001), but not the main effect of substance abuse or the violence-by-substance abuse interaction. Thus the higher scores of substance abusers on part 2 were related only to two items: item 11, adolescent antisocial behavior, and item 12, adult antisocial behavior. When these two items were eliminated, the difference between scores on part 2 of substance abusers and those who did not abuse substances was not significant.
Discussion and conclusions
The findings of this study demonstrate that psychopathic personality traits are associated with some of the violent behavior in some patients with schizophrenia. The relatively low prevalence of psychopathy in this sample— five of 51 subjects, or roughly 10 percent— is similar to the base rates reported in other civil psychiatric samples (25). Nevertheless, these data demonstrate a significant association between psychopathy as a dimensional construct and violence. Even moderate PCL:SV scores, in the range associated with possible psychopathy, were associated with violence in this sample. In contrast, the nonviolent subjects all scored below the cutoff for possible psychopathy. Thus, as expected, comorbidity between schizophrenia and psychopathy was higher among violent patients (20 percent) than among nonviolent patients (0 percent).
Psychopathy is defined in terms of characteristic interpersonal, affective, and behavioral symptoms, the latter including repeated violation of social norms. The higher PCL:SV scores of the violent subjects were not solely due to the assaultive acts by which that group was defined. If that were the case, the association between violence and psychopathy would have been tautological and trivial. Violent subjects had higher scores on both part 1 of the PCL:SV, which measures interpersonal and affective traits, and part 2, which measures antisocial behaviors. Although violent subjects scored higher on items to which a history of violent behavior per se might contribute directly, such as items 11 and 12 measuring adolescent and adult antisocial behavior, they also scored higher on items that do not necessarily have any particular association with violence. The fact that violent subjects had significantly more arrests than nonviolent subjects indicates that violent subjects had engaged in antisocial activities even outside the hospital environment.
Early age of onset of psychiatric symptoms has been reported to be associated with persistent violence (30) or belligerence (31) in psychotic inpatients. The data reported here suggest that the relationship may be mediated by psychopathy; a significant negative correlation between age of onset and PCL:SV score was found. Because the previous studies were all retrospective, it is difficult to be sure what symptoms actually emerged at the time of onset. In a classic paper, Bender (32) described the concept of "pseudopsychopathic schizophrenia" in adolescent boys who first lose impulse control and then develop chronic schizophrenia as adults. It is possible that the first contact with psychiatric services among patients with reported early onset of schizophrenia (30,31) was actually occasioned by symptoms that we would currently describe as indicative of conduct disorder or personality disorder.
Approximately two-thirds of the violent subjects in this sample were rated as possibly or definitely psychopathic. Patients with schizophrenia who are both psychopathic and violent may have a personality disorder that precedes the emergence of psychotic symptoms. Alternatively, such patients may constitute a hitherto unclassified subtype of schizophrenia, characterized by early onset of symptoms of conduct disorder and persistent violent behavior, as well as other symptoms indicative of personality disorder.
Some limitations of the study should be noted. The relatively small sample size and strict inclusion criteria have implications for the generalizability of the results. Only patients who were repetitively assaultive or who were never assaultive and never threatening were included. We cannot extrapolate the prevalence of psychopathy in schizophrenia from these data.
A less obvious limitation derives from our initial exclusion of subjects with a history of substance abuse from the nonviolent group. Substance abuse and aggression have been reported to be correlated (33), specifically among patients with schizophrenia (14). Our data probably underestimate the prevalence of substance abuse among nonviolent patients with schizophrenia and among nonpsychopathic patients with schizophrenia, 76 percent of whom were in the nonviolent group.
Nevertheless, post hoc analyses indicated only a marginal association between substance abuse and psychopathy. The associations were limited to items on part 2 of the PCL:SV, which measures antisocial behaviors; the association appears to derive solely from two items— adolescent and adult antisocial behavior. Ratings on these two items reflect the degree to which the subject engaged in antisocial activities in adolescence and adulthood; substance abuse directly contributes to ratings on these items. When these two items were eliminated from the analysis of scores on part 2, no association between substance abuse and psychopathy was found in this sample, although the association between violence and psychopathy remained. Thus the principal finding of the study appears not to have been confounded by the selection bias related to substance abuse.
A final limitation is that although published data indicate that the PCL:SV is a reliable instrument, no reliability data are available for the PCL:SV ratings in this study, which were completed by a single rater.
The authors are affiliated with the Nathan S. Kline Institute for Psychiatric Research, 140 Old Orangeburg Road, Orangeburg, New York 10962 (e-mail, [email protected]). Dr. Nolan, Dr. Volavka, and Dr. Czobor are also affiliated with the department of psychiatry at New York University School of Medicine in New York City.
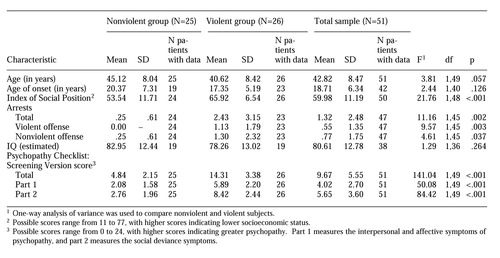 |
Table 1. Demographic and symptom characteristics of violent and nonviolent patients with schizophrenia or schizoaffective disorder and associations of these characteristics with a history of violent behavior
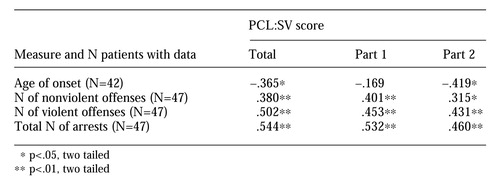 |
Table 2. Correlations of scores on the Psychopathy Checklist: Screening Version (PCL:SV) with measures of criminality and age of onset of psychiatric symptoms among patients with schizophrenia or schizoaffective disorder
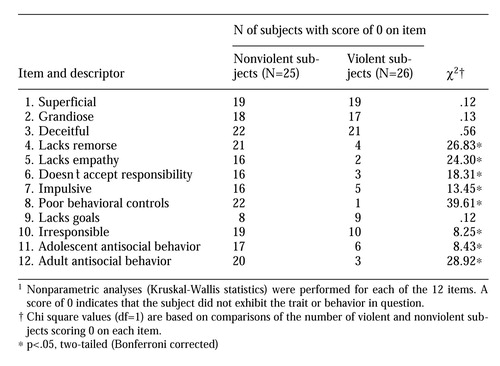 |
Table 3. Relationship between history of violence and item scores on the Psychopathy Checklist: Screening Version1
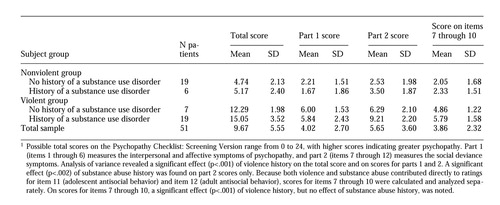 |
Table 4. Means and standard deviations of scores on the Psychopathy Checklist: Screening Version of violent and nonviolent patients with and without a history of a substance use disorder1
1. Wong S: Is Hare's Psychopathy Checklist reliable without the interview? Psychological Reports 62:931-934, 1988Google Scholar
2. Alm PO, af Klinteberg B, Humble K, et al: Psychopathy, platelet MAO activity, and criminality among former juvenile delinquents. Acta Psychiatrica Scandinavica 94:105-111, 1996Crossref, Medline, Google Scholar
3. Belmore MF, Quinsey VL: Correlates of psychopathy in a noninstitutional sample. Journal of Interpersonal Violence 9:339-349, 1994Crossref, Google Scholar
4. Hare RD, McPherson LM, Forth AE: Male psychopaths and their criminal careers. Journal of Consulting and Clinical Psychology 56:710-714, 1988Crossref, Medline, Google Scholar
5. Hare RD, McPherson LM: Violent and aggressive behavior by criminal psychopaths. International Journal of Law and Psychiatry 7:35-50, 1984Crossref, Medline, Google Scholar
6. Hare RD, Hart SD, Harpur TJ: Psychopathy and the DSM-IV criteria for antisocial personality disorder. Journal of Abnormal Psychology 100:391-398, 1991Crossref, Medline, Google Scholar
7. Harris GT, Rice ME, Quinsey VL: Violent recidivism of mentally disordered offenders: the development of a statistical prediction instrument. Criminal Justice and Behavior 20:315-335, 1993Crossref, Google Scholar
8. Hart SD, Hare RD: Psychopathy: assessment and association with criminal conduct, in Handbook of Antisocial Behavior. Edited by Stoff DM, Brieling J, Maser J. New York, Wiley, 1997Google Scholar
9. Rice ME: Violent offender research and implications for the criminal justice system. American Psychologist 52:414-423, 1997Crossref, Medline, Google Scholar
10. Hare RD: A research scale for the assessment of psychopathy in criminal populations. Personality and Individual Differences 1:111-119, 1980Crossref, Google Scholar
11. Hare RD: Psychopathy and antisocial personality disorder: a case of diagnostic confusion. Psychiatric Times, Feb 1996, pp 39-40Google Scholar
12. Volavka J: Neurobiology of Violence. Washington, DC, American Psychiatric Press, 1995, pp 175-179Google Scholar
13. Eronen M, Hakola P, Tiihonen J: Mental disorders and homicidal behavior in Finland. Archives of General Psychiatry 53:497-501, 1996Crossref, Medline, Google Scholar
14. Swanson JW: Mental disorder, substance abuse, and community violence: an epidemiological approach, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994Google Scholar
15. Link BG, Stueve A: Psychotic symptoms and the violent/illegal behavior of mental patients compared to community controls, ibidGoogle Scholar
16. Junginger J: Command hallucinations and the prediction of dangerousness. Psychiatric Services 46:911-914, 1995Link, Google Scholar
17. Junginger J, Parks-Levy J, McGuire L: Delusions and symptom-consistent violence. Psychiatric Services 49:218-220, 1998Link, Google Scholar
18. Harris GT, Varney GW: A ten-year study of assaults and assaulters on a maximum security psychiatric unit. Journal of Interpersonal Violence 1:173-191, 1986Crossref, Google Scholar
19. Hart SD, Hare RD: Discriminant validity of the Psychopathy Checklist in a forensic psychiatric population. Journal of Consulting and Clinical Psychology 1:211-218, 1989Crossref, Google Scholar
20. Hodgins S, Cote G, Toupin J: Major mental disorder and crime: an etiological hypothesis, in Psychopathy: Theory, Research, and Implications for Society. Edited by Cooke DJ, Forth AE, Hare RD. Dordrecht, The Netherlands, Kluwer Academic, 1998Google Scholar
21. Rice ME, Harris GT: Psychopathy, schizophrenia, alcohol abuse, and violent recidivism. International Journal of Law and Psychiatry 18:333-342, 1995Crossref, Medline, Google Scholar
22. Rasmussen K, Levander S: Symptoms and personality characteristics of patients in a maximum security psychiatric unit. International Journal of Law and Psychiatry 19:27-37, 1996Crossref, Medline, Google Scholar
23. Lachman HM, Nolan KA, Mohr P, et al: Association between catechol-O-methyltransferase genotype and violence in schizophrenia. American Journal of Psychiatry 155:835-837, 1998Abstract, Google Scholar
24. Strous RD, Bark N, Parsia SS, et al: Analysis of a functional catechol-O-methyltransferase gene polymorphism in schizophrenia: evidence for association with aggressive and antisocial behavior. Psychiatry Research 69:71-77, 1997Crossref, Medline, Google Scholar
25. Hart SD, Cox DN, Hare RD: The Hare PCL:SV: Psychopathy Checklist: Screening Version. North Tonowanda, NY, Multi-Health Systems, 1995Google Scholar
26. Hart SD, Hare RD, Forth AE: Psychopathy as a risk marker for violence: development and validation of a screening version of the revised psychopathy checklist, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994Google Scholar
27. Hollingshead AB, Redlich FC: Social Class and Mental Illness: A Community Study. New York, Wiley, 1958Google Scholar
28. Wechsler D: WAIS-R Manual. New York, Psychological Corp, 1981Google Scholar
29. Kaufman AS: Assessing Adolescent and Adult Intelligence. New York, Allyn & Bacon, 1990Google Scholar
30. Krakowski MI, Convit A, Volavka J: Patterns of inpatient assaultiveness: effect of neurological impairment and deviant family environment on response to treatment. Neuropsychiatry, Neuropsychology, and Behavioral Neurology 1:21-29, 1988Google Scholar
31. Sandyk R: Aggressive behavior in schizophrenia: relationship to age of onset and cortical atrophy. International Journal of Neuroscience 68:1-10, 1993Crossref, Medline, Google Scholar
32. Bender L: The concept of pseudopsychopathic schizophrenia in adolescents. American Journal of Orthopsychiatry 29:491-512, 1959Crossref, Medline, Google Scholar
33. Kennedy HG, Grubin DH: Hot-headed or impulsive? British Journal of Addiction 85:639-643, 1990Google Scholar



