P.R.N. (As-Needed) Orders and Exposure of Psychiatric Inpatients to Unnecessary Psychotropic Medications
Abstract
OBJECTIVE: The objective of this study was to evaluate whether the practice of writing standing p.r.n. (as-needed) orders exposes psychiatric inpatients to unnecessary psychotropic medications. METHODS: Medical records for 223 new hospital admissions between July 15 and October 15, 1999, when p.r.n. orders were allowed, and 224 new admissions between November 15, 1999, and February 15, 2000, when p.r.n. orders were not allowed and only "now" orders were permitted, were reviewed from the three acute adult psychiatric units of the Arkansas State Hospital in Little Rock. Data were collected on demographic and clinical characteristics, scheduled and unscheduled psychotropic medications as noted in the medication administration records, use of seclusion and restraint, and incident reports of physical aggression. The mean numbers of unscheduled psychotropic medication doses administered during the two periods were compared. RESULTS: The number of unscheduled psychotropic medications administered decreased from 1,812 in the first period to 976 in the second period (adjusted mean doses per admission, 7.8 to 4.3). The decrease in use of unscheduled medications when standing p.r.n. orders were no longer allowed was not associated with corresponding increases in adverse events: there were fewer incidents of restraint (four compared with eight), fewer incidents of seclusion (41 compared with 48), and fewer incidents of physical aggression (35 compared with 40). In addition, there were no significant changes in the dosages of scheduled psychotropic medications on day 7 of admission, indicating that physicians were not increasing dosages in response to the elimination of p.r.n. orders. CONCLUSIONS: The practice of writing p.r.n. orders may expose psychiatric inpatients to unnecessary psychotropic medications.
The use of pro re nata (p.r.n., or as-needed) psychotropic medications among hospitalized psychiatric patients is a common practice with an estimated prevalence of use ranging from 23 percent to 86 percent (1,2). When a physician writes a p.r.n. order, he or she writes orders for one or more psychotropic medications to be given at the discretion of a nurse, provided that the specified indications are met. Psychotropic medications that are commonly prescribed for this purpose include sedative antihistamines (hydroxyzine and diphenhydramine), benzodiazepines (mainly lorazepam), and antipsychotics (mainly chlorpromazine and haloperidol) (3,4,5). Common p.r.n. indications and reasons for use of these medications include prevention or containment of agitation, physical aggression, and anxiety (1,3,4,5,6,7,8). The scientific literature addressing the epidemiology, predictors, and rationale for use of p.r.n. psychotropic medications is sparse.
The underlying rationale for the use of p.r.n. orders is that nursing staff need to be able to administer psychotropic medications in a timely manner to prevent or contain agitated or violent patients in an acute psychiatric ward without having to first call a physician (3). This rationale assumes that, in the absence of p.r.n. orders, nurses would be unable to maintain a safe milieu, with resultant increases in adverse events, such as physical aggression and use of seclusion and restraint. However, we were unable to find any published data supporting this assumption.
We had the opportunity to address this issue after the Arkansas State Hospital instituted a policy in November 1, 1999, that prohibited standing p.r.n. orders for psychotropic medications. This policy was based on a conservative interpretation of guidelines of the Center for Medicare and Medicaid Services (CMS, formerly the Health Care Finance and Administration) (9). Nonscheduled psychotropic medications that were deemed necessary for symptomatic management of patients required the approval of a physician as a "now" order. On further clarification from CMS, the new policy was rescinded on February 25, 2000.
This institutionwide change in policy presented a unique opportunity for us to address two questions. First, did the change in policy to one of allowing no p.r.n. orders result in changes in the frequency of use of unscheduled psychotropic medications? Second, if there was a change in use of unscheduled psychotropic medications, was this change associated with any adverse events?
Methods
Setting, design, and subjects
The study was a retrospective review of medical records, with a pre- and postcomparison design, and was limited to patients in the three acute adult units of the Arkansas State Hospital in Little Rock, which is the only public psychiatric hospital in Arkansas. Study participants included all patients who were newly admitted to these units between July 15 and October 15, 1999, inclusive, when p.r.n. orders were allowed, and between November 15, 1999, and February 15, 2000, inclusive, when p.r.n. orders were not allowed and only physician-ordered "now" orders were permitted. Eligible participants during the two study intervals were identified from the hospital administrative database. The study was approved by the local institutional review board, which also waived the requirement to obtain informed consent.
Data collection
Multiple data sources were used. Medical records of the study participants were reviewed and relevant data abstracted onto a structured data-collecting instrument by three of the authors (PBT, SLP, and ALH). As an integral part of quality assurance at the Arkansas State Hospital, medical records are periodically reviewed and audited, especially records on medication use and use of seclusion and restraint. We thus expected that the relevant data items in the medical records would be relatively well documented.
Demographic data collected included age, gender, race, marital status, education, date of admission, date of discharge, admission unit, and whether treatment was voluntary or court ordered. Data on clinical characteristics included DSM-IV admission and discharge diagnoses, presenting symptoms, history of alcohol and drug abuse, year of first psychiatric hospitalization, and family history of mental illness. Data on scheduled psychotropic medications were collected from the medication administration records and included the name of the medication, dosage, schedule, route of administration, start and stop dates, and changes in dosage and schedule during the hospital stay. Dosage data from day 7 of admission were used to measure whether there were any changes in the dosages of scheduled medications during the two study intervals.
Data on unscheduled psychotropic medications administered through either p.r.n. or "now" orders were collected from the medication administration records for p.r.n. medications and from nursing notes and included the name of the medication, dosage, route of administration, time and date given, and reasons for administration. Data on p.r.n. orders for psychotropic medications were collected from physicians' orders and from the medication administration record for p.r.n. medications and included the name of the medication, dosage, schedule, route, and indication.
Data on the use of seclusion and restraint were obtained from logs within the medical records and included date and time of use, duration, and reason for use. For every "out of the ordinary" incident on the unit, staff are required to fill out an incident report and submit it to the hospital's quality assurance office. All incident reports filed by the units during the study periods were reviewed, and incidents of physical aggression in the units and those associated with study participants were identified.
Analysis
The total number of unscheduled psychotropic medication doses given to study participants for each period was summed. The mean numbers of unscheduled doses were compared between the two periods. We also performed an analysis by using the rate of unscheduled medications per admission per week (the number of unscheduled psychotropic medications divided by the number of days in the hospital multiplied by 7) as the unit of analysis. Because both results were similar, only the mean is presented.
Statistical differences were tested by using Student's t test for continuous variables and the chi square test for categorical variables. To adjust for factors that may affect use of unscheduled medications, we performed multiple regression analysis using PROC GLM. The model included terms that were set a priori and those that were significantly different between the two groups. All analyses were performed with PC-SAS version 8.2 (SAS Institute Inc, Cary, North Carolina), and all p values are two sided.
Results
The two study samples included 218 patients with 231 admissions during the period when p.r.n. orders were allowed (the first period) and 219 patients with 226 admissions during the period when p.r.n. orders were not allowed (the second period). The analysis reported here is based on the 223 admissions during the first period and 224 admissions during the second period for which we were able to review medical records.
The two groups were comparable in their demographic and clinical characteristics with the exception of age and marital status; patients from the period when p.r.n. orders were allowed were more likely to be younger and single (Table 1). Patients from the period when p.r.n. orders were allowed also tended to be less educated, to have fewer involuntary admissions, to be more likely to have a primary diagnosis of a psychotic disorder, and to have a longer duration of mental illness than the participants from the later period, although these differences between the two groups were not statistically significant.
During the period when p.r.n. orders were allowed, 95 percent of the study participants (212 admissions) had at least one written p.r.n. order. This figure dropped to 7.6 percent (17 admissions) during the period when p.r.n. orders were not allowed.
As shown in Table 2, the proportion of patients who were given at least one unscheduled psychotropic medication decreased significantly from 79 percent (175 admissions) during the first period to 67 percent (148 admissions) during the second period. The total number of unscheduled psychotropic medication doses administered also decreased from 1,812 to 976, for unadjusted means of 8.1 and 4.4, respectively. The adjusted mean number of doses per admission was 7.8 and 4.3 for the two periods, respectively.
A small percentage of admissions accounted for a disproportionately large number of the unscheduled psychotropic medication doses administered. In the period when p.r.n. orders were allowed, 30 (14 percent) of 223 patients received 969 (54 percent) of the 1,812 unscheduled medication doses. In the period when p.r.n. orders were not allowed, 11 (5 percent) of the 224 patients received 409 (42 percent) of the 976 unscheduled doses.
The most frequently used unscheduled psychotropic medications included antipsychotics (mostly haloperidol and chlorpromazine) (685 doses, or 38 percent, during the first period compared with 404 doses, or 41 percent, during the second period), benzodiazepines (mostly lorazepam and clonazepam) (641 doses, or 35 percent, compared with 310 doses, or 32 percent), sedatives (mostly hydroxyzine, trazodone, and zolpidem) (431 doses, or 24 percent, compared with 221 doses, or 23 percent), and anticholinergics (mostly benztropine) (52 doses, or 3 percent, compared with 41 doses, or 4 percent). Patients with a primary diagnosis of a psychotic disorder or bipolar disorder accounted for 70 percent (N=1,972) of the unscheduled doses during both periods.
Use of unscheduled medication doses were mostly staff initiated, but during the period when p.r.n. orders were allowed, 329 (24 percent) were given at the patient's request. This proportion dropped significantly to 13 percent (N=97) (p<.001) during the period when p.r.n. orders were not allowed.
The day-7 dosages of risperidone, olanzapine, quetiapine, haloperidol, chlorpromazine, lorazepam, and clonazepam as well as the proportion of study participants receiving these scheduled medications were essentially similar during the two periods.
During the period when p.r.n. orders were allowed, eight patients were placed in restraints, compared with four during the period when p.r.n. orders were not allowed. During the first period, 48 patients were placed in seclusion, compared with 41 in the second period. However, the mean number of hours of seclusion in the second period was greater (19.2 compared with 13.1). These differences were not statistically significant.
The number of reported incidents of physical aggression did not increase after the new policy was implemented. A total of 27 admissions accounted for 40 incidents of aggression in the period when p.r.n. orders were allowed, compared with 19 admissions with 35 incidents in the period when p.r.n. orders were not allowed. During the first period there were 14 employee injury reports related to a patient in the study units, compared with 12 such reports in the second period.
The mean length of hospital stay was similar in the two groups (18.3 days in the first period and 18.9 days in the second period).
Discussion and conclusions
Although the use of p.r.n. orders for psychotropic medications is a common practice, there have been few published studies on this topic. Furthermore, the basic question of whether such a practice is necessary for good patient care has not been studied. Taking advantage of a dramatic policy change at our institution, we were able to address this issue. We found a 47 percent decrease in the frequency of use of unscheduled psychotropic medications after the implementation of a policy that prohibited the use of p.r.n. orders, even after we controlled for other factors that could have influenced the use of these medications.
When the policy of disallowing p.r.n. orders was instituted, there were concerns that nurses would not be able to administer unscheduled psychotropic medications in a timely manner. Accordingly, the staff would not be able to prevent and contain disruptive patient behavior or maintain a safe milieu in the units. It was predicted that such an outcome would result in greater use of seclusion and restraint and in more acts of physical aggression. Furthermore, without the ability to write p.r.n. orders, physicians may compensate by writing orders for additional scheduled psychotropic medications or for higher dosages.
Our data indicate that these concerns were unfounded. Although there was a significant decrease in the number of psychotropic medications administered during the period when p.r.n. orders were not allowed, we did not find a corresponding increase in the frequency of adverse events, such as greater use of seclusion and restraint and more incidents of physical aggression. We also did not see a corresponding increase in dosages of scheduled psychotropic medications. Furthermore, there was no evidence to suggest that patients were denied unscheduled psychotropic medications if they were needed.
Clearly, the addition of an extra barrier to the administration of unscheduled medications—that is, having to call a physician—in the period when p.r.n. orders were not allowed played a significant role in changing practice and thus decreasing use of these medications. For example, we found a significant decrease in the use of unscheduled medications that were administered at the patient's request (from 329 to 97 medication doses during the period when p.r.n. orders were not allowed.
We were unable to collect data to evaluate possible adverse effects associated with the use of these unscheduled psychotropic medications. These agents are potent medications, and unnecessary administration may place patients at increased risk of side effects that may be significant (10). In addition, there is concern that p.r.n. orders may be used as "chemical restraints" or for the convenience of staff (5,9,10). The results of our study thus raise the uncomfortable question of whether p.r.n. orders are for the benefit of the patient or of the staff.
At our institution, psychiatrists are readily available 24 hours a day. Thus even when p.r.n. orders were not allowed, nursing staff were able to get approval for an unscheduled medication as a "now" order relatively quickly. Anecdotal reports suggested that physicians rarely denied nursing requests for unscheduled medications, although we were unable to collect data on this issue. However, in hospitals where a physician is not readily available or the unscheduled medications are not readily available without existing p.r.n. orders, obtaining a medication to be given as a "now" order may take excessive time. Under these circumstances, judicious use of p.r.n. orders may be desirable.
In addition to the inherent limitations of a retrospective study, our study has three possible limitations. First, the results are based on data from a single site and thus may not be readily generalizable. However, these findings may be more applicable to public-sector psychiatric hospitals similar to ours. Second, adverse events may have been underreported. However, this possibility was probably not a significant factor, because every incident of seclusion or restraint and every untoward incident must be separately documented at the hospital and is closely audited and monitored by the hospital's quality assurance office. Furthermore, any reporting bias would probably have been in the direction of an increased number of adverse event reports during the period when p.r.n. orders were not allowed, given that both physician and nursing staff were somewhat skeptical of this policy.
Finally, the scope of our study did not allow us to evaluate a bona fide need for the unscheduled psychotropic medications used or to directly measure psychiatric symptoms and functional outcomes. Nevertheless, this is the first study to address the underlying rationale for this practice, and the results are compelling.
In conclusion, our findings indicate that the use of p.r.n. orders may expose psychiatric inpatients to unnecessary psychotropic medications. Given the objective of regulatory bodies to minimize the use of "chemical restraints" in this population of vulnerable patients, these findings have important policy implications. However, additional studies are needed to verify our findings.
Acknowledgments
This study was partly supported by the Theodore and Vada Stanley Foundation. Dr. Thapa conducted part of this study as a research fellow at the Center for Mental Health Care Research of the National Institute of Mental Health (grant MH-20024-03) in the department of psychiatry of the University of Arkansas for Medical Sciences.
The authors are affiliated with the department of psychiatry at the University of Arkansas for Medical Sciences in Little Rock. Dr. Thapa and Dr. Miller are also affiliated with the Arkansas State Hospital in Little Rock. Dr. Owen is also affiliated with the Health Services Research and Development Center for Mental Healthcare and Outcomes Research of the Central Arkansas Veterans Healthcare System. Send correspondence to Dr. Thapa at the Department of Psychiatry, Slot 554, University of Arkansas for Medical Sciences, 4301 West Markham, Little Rock, Arkansas 72205 (e-mail, [email protected]). A version of this paper was presented at the annual meeting of the American Psychiatric Association held May 18 to 23, 2002, in Philadelphia.
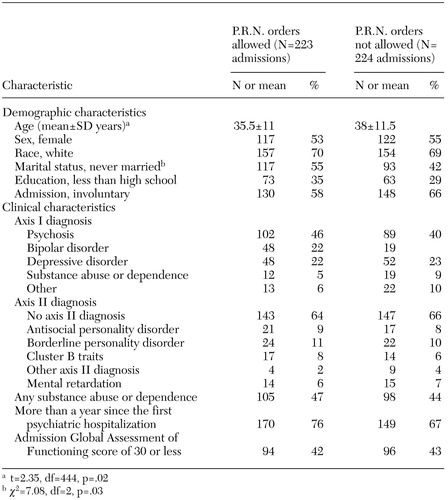 |
Table 1. Demographic and clinical characteristics of patients newly admitted to a state hospital during a period when p.r.n. (as-needed) orders were allowed and a period when they were not allowed
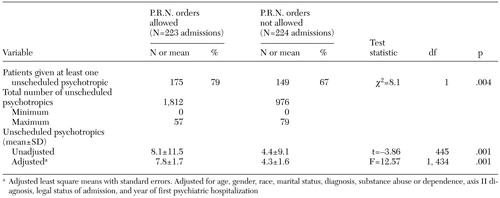 |
Table 2. Total, unadjusted, and adjusted mean number of unscheduled psychotropic medications administered during the period when p.r.n. (as-needed) orders were allowed and the period when they were not allowed
1. Craig TJ, Bracken J: An epidemiologic study of prn/stat medication use in a state psychiatric hospital. Annals of Clinical Psychiatry 7:57–64, 1995Crossref, Medline, Google Scholar
2. Vitiello B, Ricciuti AJ, Behar D: PRN medications in child state hospital inpatients. Journal of Clinical Psychiatry 48:351–354, 1987Medline, Google Scholar
3. Fishel AH, Ferreiro BW, Rynerson BC, et al: As-needed psychotropic medications: prevalence, indication, and results. Journal of Psychosocial Nursing and Mental Health Services 32(8):27–32, 1994Google Scholar
4. Walker R: PRN psychotropic drug use on a psychiatric unit. Psychiatric Quarterly 62 (1):1–8, 1991Google Scholar
5. Craven JL, Voore PM, Voineskos G: PRN medication for psychiatric inpatients. Canadian Journal of Psychiatry 32:199–203, 1987Medline, Google Scholar
6. Gray R, Smedley N, Thomas B: The administration of PRN medication by mental health nurses. Journal of Psychiatric and Mental Health Nursing 4(1):55–56, 1997Google Scholar
7. Kaplan SL, Busner J: The use of prn and stat medication in three child psychiatric inpatient settings. Psychopharmacology Bulletin 33:161–164, 1997Medline, Google Scholar
8. McLaren S, Browne FW, Taylor PJ: A study of psychotropic medication given "as required" in a regional secure unit. British Journal of Psychiatry 156:732–735, 1990Crossref, Medline, Google Scholar
9. Centers for Medicare and Medicaid Services: Interpretive Guidelines for Hospital COP for Patients' Rights. Available at http://cms.hhs.gov/cop/2b.aspGoogle Scholar
10. Ayd Jr FJ: Problems with orders for medication as needed. American Journal of Psychiatry 142:939–942, 1985Link, Google Scholar



