Pediatric Emergency Department Assessment of Psychological Trauma and Posttraumatic Stress
Abstract
OBJECTIVES: This study aimed to describe the kinds of stressors and the extent of symptoms of posttraumatic stress disorder (PTSD) that were reported by children and their parents in a pediatric emergency department and to examine the response rate to an emotional trauma questionnaire in this setting. METHODS: Three self-report questionnaires were given to patients aged eight to 21 years and to their primary caretakers: a brief assessment of service use, the Posttraumatic Stress Reaction Index (PTSRI), and the Impact of Event Scale (IES). RESULTS: Sixty-four of 81 families who were approached agreed to participate (consent rate of 79 percent), and 62 completed the questionnaires. Fifty-six patients reported at least one event that met DSM-IV-TR criteria for emotional trauma. The average number of reported events per child was 3.14 (range, 0 to 7). Eighteen patients met threshold criteria for severity of PTSD symptoms. Twenty-five patients reported that the most distressing traumatic event that they experienced was related to a medical illness. Patients with PTSD reported exposure to more adverse life events than patients without PTSD. IES scores reported by caretakers who identified the same event as their child as the most stressful were as high as those of caretakers who reported a different event as the most stressful. CONCLUSIONS: Exposures to emotionally traumatic events and PTSD symptoms are commonly reported in the pediatric emergency department. Asking children and their parents about their history of emotional trauma when they visit the emergency department is possible and can be well received.
The prevalence of posttraumatic stress disorder (PTSD) among adolescents in the United States has been estimated at 6 percent (1) in community settings. PTSD symptoms and exposure to emotionally traumatic events have been associated with greater use of medical services (2) and to nonadherence to treatment (3,4,5). These findings suggest that screening for symptoms of PTSD, if feasible, could be used to alert physicians to the elevated likelihood of morbidity in identified cases (2,3,5).
Clinical and epidemiologic studies have tried to assess the degree of children's exposure to adverse life events, particularly as it relates to the occurrence of child abuse and violence (6,7). However, other forms of emotional trauma have not been as well characterized or studied, and a DSM-IV-TR criterion A definition of a traumatic event (8) has not been used in previous prevalence studies conducted in primary care pediatric settings (9). It is important to perform a broad and precise study of trauma exposure, including traumatic events other than exposure to violence, because traumas other than violence and abuse have also been associated with specific disabilities.
For example, studies conducted in specialty care settings have shown that emotional trauma associated with medical illness is prevalent (10,11,12,13) and is associated with poor medical outcome (14). Treatment of PTSD related to medical illness may improve outcome (5,15). Emotional traumatization by severe medical illness, unlike child abuse, does not necessarily involve a profound disruption of family structure or loss of trust in the child's primary support system (16) and thus may be more amenable to focused treatment strategies than the emotional trauma associated with abuse.
Despite these data, screening for exposure to emotionally traumatic events and symptoms of PTSD is not routinely attempted in pediatric care settings. A concern may be that patients who seek medical care may be reluctant to disclose emotionally traumatic events or will be adversely affected by disclosure and not be able to receive proper care.
Perhaps because of these considerations, no published broad studies have been conducted in pediatric primary care settings that focus on the nature of emotionally traumatic events reported by children who present for medical care. An inner-city pediatric emergency department may be the only point of contact for routine medical care for an especially underprivileged social stratum (17). Thus the visit to the pediatric emergency department may present a window of opportunity to screen patients and attempt interventions.
The primary aims of this study were to describe the kind of stressors and the extent of PTSD symptoms and traumatic exposure reported by a sample of children and their parents when approached in the pediatric emergency department and to examine the response rate to a structured emotional trauma questionnaire in order to determine whether patients and families are likely to agree to answer these questions in the pediatric emergency department. Secondary aims were to explore whether symptoms of emotional trauma may sometimes be clinically important in this setting, such as in predicting service use and informing management in the pediatric emergency department; to examine whether reporting the experience of more adverse events is associated with self-reported symptoms of emotional trauma; and to examine the degree of distress experienced by a caretaker in relation to the child's traumatic experience compared with other stressors in the parent's life. Because this study predated the September 11, 2001, attack on the World Trade Center, it provides a rare glimpse into the pre-September 11 characteristics of traumatization in New York City.
Methods
A convenience sample of eight- to 21-year-old patients and their families was recruited between September 2000 and May 2001 during evaluation of the patients in the pediatric emergency department. The limited availability of interviewers, who did not belong to the medical staff, accounted for the long study period. Critically ill patients were excluded. Full written consent and assent were obtained in accordance with guidelines of our institutional review board. Clinical staff were made aware of the study and were free to interrupt the assessments if medically indicated.
The Mount Sinai Medical Center's pediatric emergency department serves an eclectic population of affluent and poor neighborhoods. The medical center is not a designated medical trauma center. Thus children with severe injuries—for example, victims of motor vehicle accidents or serious burns—are not usually served in this pediatric emergency department.
The self-report questionnaires were given to the child and the primary caretaker. A total of three questionnaires were administered: a brief assessment of the reason for the visit to the pediatric emergency department and of service use; the Posttraumatic Stress Reaction Index (PTSRI) (unpublished copyrighted instrument, Rodriguez N, Steinberg A, Pynoos RS, 1998), which includes questions about the kind of emotionally traumatic events to which the child was exposed and the child's emotional response to them; and the Impact of Event Scale (IES) (18), which asks about the caretaker's emotional response to the child's identified traumatic event or to other emotionally traumatic events in the caretaker's own life.
The first questionnaire asked the respondent to report the reason for the current pediatric emergency department presentation, the extent of use of the pediatric emergency department in the past three months, and chronic illnesses.
An earlier version of the second questionnaire, the PTSRI, was the first PTSD screen to be used with children. It has been validated against clinical diagnoses. The newer version includes an emotional trauma screen consisting of 11 questions about several kinds of potentially traumatic events: being in a disaster; being in a bad accident; being in a place where a war is going on; being hurt very badly by a family member; witnessing a family member being hurt by another family member; being beaten up, shot, or threatened in your neighborhood; seeing somebody else being beaten up, shot, or threatened in your neighborhood; having your private parts touched by another person; finding out about the death or serious injury of a close family member or friend; having a very serious medical problem; and experiencing another stressful event (specify). The respondent is asked to choose the most traumatic event among those identified in the previous screen and is then asked whether the event was perceived as physically threatening and whether the response to the event at the time it occurred met the DSM-IV-TR criteria. Finally, a third section asks about DSM-IV-TR PTSD symptoms, which are rated on a Likert scale ranging from 1 to 4, with higher scores indicating worse symptoms. For the purpose of defining an above-threshold PTSD category, on the basis of our previous observations on the threshold value among children who received a transplant (5) we used a restrictive approach that counts an answer as positive only if the respondent states that the symptoms have been experienced at least once a week (a score of 2 or above).
On the basis of previous observations that parents are not always aware of the child's exposure to and symptoms of trauma (5,19), we used the child's report as the PTSD and trauma variable. The PTSRI was administered to children in its two versions: a child version (for children aged eight to 12 years) and an adolescent version (for those aged 12 and older). Although the PTSRI is an accepted trauma assessment tool, the scores obtained by using this instrument are not synonymous with a psychiatric diagnosis.
The third questionnaire, the IES, was used to determine emotional distress among the primary caretakers. The IES is a 15-item questionnaire that asks about symptoms of intrusion and avoidance but not about hyperarousal symptoms of PTSD. The IES has been the most widely used measure of PTSD symptoms and has been examined in numerous clinical settings (20). Although cutoff points have been established, the questionnaire is most frequently used to determine a general level of distress rather than to make a categorical diagnosis of PTSD.
In the study reported here, the primary caretakers were asked to identify the "worst experience of your life"—that is, the worst experience of the caretakers' own lives—and answer the IES questions in relation to that event, whether this was related to their child's trauma or not. This approach was used to enable us to compare the level of caretaker's distress that is associated with the child's emotionally traumatic exposure with other stressors that the caretakers have encountered in the course of their own lives.
A pediatric emergency department attending physician who was not involved in data gathering reviewed the cases and determined whether information obtained in the interviews was clinically relevant—that is, whether it had the potential to alter the management of the case in the pediatric emergency department or lead to a new referral.
Statistical analysis was conducted by using SPSS, version 10. To analyze the association between PTSD and past exposure, we used logistic regression analysis, using age and sex as covariates. For the relationship between service use (pediatric emergency department visits) and PTSD, we rank ordered the number of visits so as to reduce the effect of extreme observations and performed an analysis of variance (ANOVA). At a second stage, we used number of exposures, and then age and sex, as covariates to control for the potential effects of these variables. PTSD symptoms were summarized into a dichotomy (PTSD or no PTSD) by using preestablished cutoff points for the children but were totaled as a continuous variable for the parents. This approach was used because the child PTSD measure was DSM-IV compatible, whereas the parents' measure was not.
Results
Eighty-one patients and their families were approached. Of these, 64 (79 percent) gave informed consent. Two of these patients were discharged immediately after the consent procedure and terminated their participation before answering the PTSRI. Thus the final cohort consisted of 62 patients who answered the PTSRI and the introductory questionnaire. Thirty-three primary caretakers answered the IES questionnaire. The patients' age distribution is presented in Table 1. Thirty-eight respondents (61 percent) were female, 38 (61 percent) were Caucasian, 15 (24 percent) were Hispanic, and nine (5 percent) were African American.
Patients' burden—that is, time taken to answer the questionnaires—averaged 30 to 40 minutes for the three questionnaires and up to 25 minutes for the PTSRI alone (range, five to 25 minutes).
Fifty-six patients (90 percent) reported at least one event that met DSM-IV-TR criteria for emotional trauma. The average number of reported adverse life events per child in this cohort was 3.14 (range, 0 to 7). Eighteen patients (29 percent) met the predetermined threshold criteria for severity of PTSD symptoms.
Twenty-five patients (40 percent of the total) reported that the most distressing emotionally traumatic event that they experienced was related to a chronic medical illness, most commonly the child's illness but sometimes the illness of a family member. Thus stressors related to a medical illness were by far the most frequently cited emotionally traumatic events in this study. Types of emotional traumas that were reported as "most distressing" are listed in Table 1.
In most cases (48 patients, or 77 percent), the most distressing emotional trauma was not immediately related to the current visit to the pediatric emergency department. Thus the patients were reporting mainly about past exposure and not about the event that directly led to the visit to the pediatric emergency department.
Patients who had PTSD reported, on average, exposure to more adverse life events than patients who did not meet threshold criteria (a mean±SD of 2.53±1.63 for patients without PTSD, compared with 4.44±1.50 for patients with PTSD). Using logistic regression, we assessed the association of PTSD with the number of reported adverse events, controlling for age and gender. A statistically significant association was noted between PTSD and past exposure, with no significant interactions between the covariates and the independent variable (χ2=17, df=1, p<.001).
Considering the IES scores reported for the worst event identified by caretakers, IES scores related to the child's traumatic event were as high as the IES scores that were reported for other kinds of emotional trauma (the mean IES score for the caretakers' symptoms related to the child's event was 32.8±19.26 and for other stressors was 30.6±17.54). Thus traumatic stress symptoms reported by caretakers who referred to an event that was identified as traumatic by the child were as severe as the symptoms reported by caretakers who referred to other kinds of trauma.
Patients with above-threshold PTSD symptoms reported a higher number of visits to the pediatric emergency department in the three months preceding the interview than patients who did not report these symptoms (Table 2). We rank ordered the number of visits to heighten the distinction among patients who reported fewer visits as explained above—three patients who reported ten or more visits and 54 patients who reported one to three visits—so as to minimize the effect of statistical outliers. The ANOVA revealed that the rank-transformed number of visits was significantly larger for patients with PTSD (F=12.82, df=1, 57, p=.001). After we controlled for the number of reported adverse life events, there was still a significant association between PTSD and the number of visits (F=6.75, df=1, 56, p=.02), which suggests that service use was related to the emotional impact of trauma and that this relationship was not entirely due to the number of reported exposures per se. This relationship persisted after we controlled for age and sex.
A reviewer who was not involved in clinical care or in the survey determined that for ten of 62 patients (16 percent), clinical management in the pediatric emergency department may have been significantly altered by knowledge of the emotional trauma history. The following case history is presented as an illustration of a potential—but not proven—benefit of such a screen.
A nine-year-old girl presented with an episode of syncope after an inpatient noninvasive evaluation for the same complaint that revealed no reason for the syncope except a mild sinus arrhythmia. The girl experienced a fainting episode two days after her discharge from the inpatient unit. A consulting cardiologist was called with the specific request to consider a cardiac catheterization and electrophysiological studies. While waiting for the consultation, the patient was interviewed by the research team. She revealed that the salient trauma in her life was watching her 21-year-old sister fall down and lose consciousness. After that episode, the older sister was given a diagnosis of multiple sclerosis, had a few other fainting episodes, and was unable to walk for a few months. The patient described vivid intrusive recollections of the event and heightened general anxiety since then.
With the patient's permission, these findings were shared with the cardiologist, who decided not to perform the catheterization on the basis of this history. A psychiatric follow-up was recommended. Two and four weeks after the visit, the patient had had no further fainting episodes, although she complained of lightheadedness.
Discussion
In a context in which terrorist attacks are discussed and anticipated, the question of whether children and caretakers are willing to answer a direct inquiry about emotional trauma carries a special significance. Thus the most important finding of our study is that, in contrast with our expectations, patients were not reluctant to answer the questions, as indicated by the high response rate.
The rates of exposure to adverse events reported in this study seem high (a mean of 3.14 adverse events reported per child). Only the most stressful event was examined in detail in the questionnaire, and 90 percent of the children did identify at least one DSM-IV-TR criterion A emotionally traumatic event. In this context, it is not surprising that the rate of PTSD was 29 percent in our cohort. Larger studies seem to be indicated to examine whether our findings are indeed representative of urban emergency department settings.
We found high levels of emotional trauma symptoms in this study, which predated the September 11, 2001, attack on the World Trade Center and the Pentagon. Our findings suggest that current high levels of reported distress or PTSD symptoms in New York City should be interpreted cautiously and should not be automatically attributed to September 11 and the threat of terrorism.
Several limitations of this study must be acknowledged. First, we used a convenience sample, and the relatively small number of participants introduces some degree of uncertainty about the generalizability of the results. However, our results are at the very least an indication that trauma rates may be high, and they strongly suggest that further research is indicated. Second, we could not ascertain the clinical diagnosis of PTSD—this would have necessitated an interview with an experienced clinician. Third, results obtained in our setting may not be applicable to other settings.
PTSD symptoms were associated with more reported service use. This finding is consistent with other reports (2). Although it is possible that addressing trauma-related symptoms would lead to decreased use of the pediatric emergency department, our study did not directly investigate this possibility.
The emotionally traumatic impact of chronic or acute medical illness has been investigated in several pediatric disease processes (5,10,11,16,21), but a study in a specific general pediatric outpatient setting has not been previously attempted. Our results point to the importance and magnitude of traumatization due to a medical illness, both to the child and to the caretaker. The potentially traumatic impact of medical illness is rarely addressed routinely in medical settings—the settings in which it is expected to be most prevalent.
When considering the trauma that caretakers identified as the worst trauma, we found that a child's trauma can be as distressing to a caretaker as other types of trauma that the caretaker has experienced. Symptoms reported in this study were related mainly to events that were not at the core of the current visit to the pediatric emergency department. Thus the finding that caretakers are extremely distressed by the child's reported traumatic event is probably not an artifact of the setting but rather represents a real effect of the child's emotionally traumatic experiences on the caretakers.
Conclusions
Exposures to emotionally traumatic events and symptoms of PTSD are commonly reported in the pediatric emergency department. Asking patients and their parents about their history of emotional trauma when they visited the pediatric emergency department was possible and seemed to be well received. We hope our results will encourage other clinicians to ask about emotional trauma and that the findings will serve as an indication that larger studies are feasible and are needed to address the prevalence and impact of emotional trauma in similar settings.
Acknowledgments
This study was supported in part by a Klingenstein 3rd Generation Foundation Fellowship award and by grant MH-63755 from the National Institutes of Health to Dr. Shemesh and by a Brookdale Foundation grant to Dr. Yehuda.
Dr. Shemesh, Dr. Newcorn, Dr. Schmeidler, and Dr. Yehuda are affiliated with the department of psychiatry at Mount Sinai Medical Center in New York City; Dr. Shemesh is also affiliated with the department of pediatrics, and Dr. Schmeidler is also affiliated with the department of biomathematical sciences. Dr. Keshavarz, Ms. Leichtling, Mr. Weinberg, Mr. Mousavi, and Dr. Sadow are with the department of emergency medicine at Mount Sinai Medical Center; Dr. Keshavarz and Dr. Sadow are also affiliated with the department of pediatrics. Send correspondence to Dr. Shemesh at Department of Psychiatry, Box 1230, Mount Sinai Medical Center, 1 Gustave L. Levy Place, New York, New York 10029 (e-mail, [email protected]).
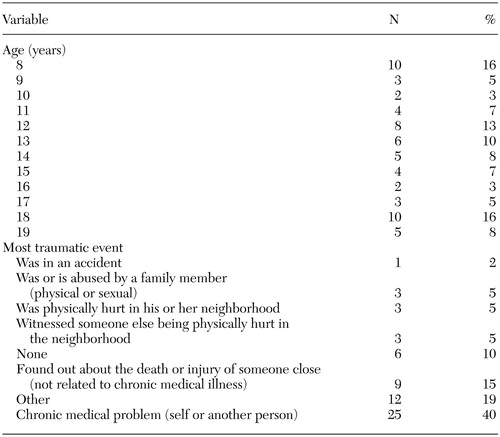 |
Table 1. Study participants' ages at the time of interview in the pediatric emergency department and the most traumatic events reported (N=62)
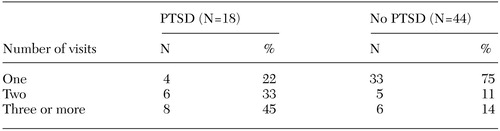 |
Table 2. Patients with and without posttraumatic stress disorder (PTSD) who reported one, two, or at least three visits to the pediatric emergency department in the three months before evaluation
1. Giaconia RM, Reinherz HZ, Silverman AB, et al: Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 34:1369–1380, 1995Crossref, Medline, Google Scholar
2. Stein MB, McQuaid JR, Pedrelli P, et al: Posttraumatic stress disorder in the primary care medical setting. General Hospital Psychiatry 22:261–269, 2000Crossref, Medline, Google Scholar
3. Shemesh E, Rudnick A, Kaluski E, et al: A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI). General Hospital Psychiatry 23:215–222, 2001Crossref, Medline, Google Scholar
4. Lurie S, Shemesh E, Sheiner PA, et al: Nonadherence in pediatric liver transplant recipients: an assessment of risk factors and natural history. Pediatric Transplant 4:200–206, 2000Crossref, Medline, Google Scholar
5. Shemesh E, Shneider BL, Stuber ML, et al: Symptoms of post traumatic stress disorder and nonadherence in pediatric liver transplant recipients. Pediatrics 105:1–7, 2000Crossref, Medline, Google Scholar
6. Schwab-Stone ME, Ayers TS, Kasprow W, et al: No safe haven: a study of violence exposure in an urban community. Journal of the American Academy of Child and Adolescent Psychiatry 34:1343–1352, 1995Crossref, Medline, Google Scholar
7. Schwab-Stone M, Chen C, Greenberger E, et al: No safe haven: II. the effects of violence exposure on urban youth. Journal of the American Academy of Child and Adolescent Psychiatry 38:359–367, 1999Crossref, Medline, Google Scholar
8. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision (DSM-IV-TR). Washington, DC, American Psychiatric Association, 2000Google Scholar
9. Purugganan OH, Stein REK, Silver EJ, et al: Exposure to violence among urban school-aged children: is it only television? Pediatrics 106:949–953, 2000Google Scholar
10. Stuber ML, Nader K, Yasuda P, et al: Stress response following pediatric bone marrow transplantation: preliminary results of a prospective, longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry 30:952–957, 1991Crossref, Medline, Google Scholar
11. Stuber ML, Kazak AE, Meeske K, et al: Predictors of post traumatic stress symptoms in childhood cancer survivors. Pediatrics 100:958–964, 1997Crossref, Medline, Google Scholar
12. Stukas AA, Dew MA, Switzer GE, et al: PTSD in heart transplant recipients and their primary family caregivers. Psychosomatics 40:212–221, 1999Crossref, Medline, Google Scholar
13. Doerfler LA, Pbert L, DeCoimo D: Symptoms of posttraumatic stress disorder following myocardial infarction and coronary artery bypass surgery. General Hospital Psychiatry 16:193–199, 1994Crossref, Medline, Google Scholar
14. Dew MA, Kormos RL, Roth LH, et al: Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. Journal of Heart and Lung Transplantation 18:549–562, 1999Crossref, Medline, Google Scholar
15. Courtemanche DJ, Robinow O: Recognition and treatment of the post-traumatic stress disorder in the burn victim. Journal of Burn Care and Rehabilitation 10:247–250, 1989Crossref, Medline, Google Scholar
16. Pelcovitz D, Libov BG, Mandel F, et al: Posttraumatic stress disorder and family functioning in adolescent cancer. Journal of Traumatic Stress 11:205–221, 1998Crossref, Medline, Google Scholar
17. Smith RD, McNamara JJ: Why not your pediatrician's office? A study of weekday pediatric emergency department use for minor illness care in a community hospital. Pediatric Emergency Care 4:107–111, 1988Crossref, Medline, Google Scholar
18. Horowitz M, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine 41:209–218, 1979Crossref, Medline, Google Scholar
19. Pfefferbaum B: Posttraumatic stress disorder in children: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry 36:1503–1511, 1997Medline, Google Scholar
20. Handbook of Psychiatric Measures. Washington, DC, American Psychiatric Association, 2000Google Scholar
21. Saxe G, Stoddard F, Courtney D, et al: Relationship between acute morphine and the course of PTSD in children with burns. Journal of the American Academy of Child and Adolescent Psychiatry 40:915–921, 2001Crossref, Medline, Google Scholar



