A Program for Managing Weight Gain Associated With Atypical Antipsychotics
Abstract
This study assessed the efficacy of a weight control program for patients taking atypical antipsychotics. Thirty-one patients with schizophrenia or schizoaffective disorder participated in a 12-week weight control program that incorporated nutrition, exercise, and behavioral interventions. Changes in patients' weight and in body mass index (BMI) were recorded and compared with those of 15 patients in a control group. The intervention group had a mean weight loss of 2.7 kg (six pounds) and a mean reduction of .98 BMI points, compared with a mean weight gain of 2.9 kg (6.4 pounds) and a mean gain of 1.2 BMI points in the control group. These data suggest that the intervention was effective in this group of patients. Professionals treating persons who are taking atypical antipsychotics should encourage them to engage in weight control activities.
Atypical antipsychotics are associated with superior tolerability, adherence, and relapse prevention and have led to improved treatment for patients with serious mental illness. However, they are also associated with weight gain. Medication-induced weight gain has been well documented for both conventional neuroleptics and atypical antipsychotics (1,2,3).
According to the guidelines of the National Heart, Lung, and Blood Institute (NHLBI) (4), treatment of overweight or obese adults is a two-step process involving assessment and treatment management. Assessment includes assessing body mass index (BMI), diet, waist circumference, risk status, and level of motivation. The BMI is one of the most accurate ways to determine whether an adult is overweight. It is a gauge of total body fat, calculated by dividing the person's weight (in kilograms) by his or her height (in square meters). A person with a BMI of 25 or greater is considered to be overweight and with a BMI of 30 or greater is considered to be obese.
According to the NHLBI's guidelines, treatment strategies for overweight and obesity include modifications in diet, behavior, and physical activity. Combined therapy that incorporates all three approaches is most successful. Weight loss has many health-related benefits: reduction in risk of diabetes and cardiovascular disease (4,5,6), reduction of serum triglycerides and total and low-density lipoprotein (LDL)-cholesterol concentrations, increase in high-density lipoprotein (HDL)-cholesterol concentrations, and reduction in blood glucose concentrations and in hemoglobin A1c among patients with type 2 diabetes.
Currently, there are no established weight loss interventions for patients with schizophrenia. Schizophrenia is frequently accompanied by deficits in attention, motivation, and memory that could directly affect patients' ability to benefit from such programs. However, existing data suggest that such patients can benefit from weight-gain prevention strategies and weight loss interventions. Wirshing and associates (7) reported success with a stepwise approach with patients taking atypical antipsychotics. Patients were referred to a "wellness clinic," which involved a rigorous evaluation of exercise and dietary habits. Preliminary findings from a small pilot program (8) further suggest that psychoeducational interventions prevent weight gain associated with atypical antipsychotics.
The purpose of the study reported here was to demonstrate the feasibility and efficacy of a weight control program for adults with severe mental illness who had gained weight while taking atypical antipsychotics. We hypothesized that patients who participated in a structured weight control program would lose more weight than those who received usual psychiatric care.
Methods
Thirty-one patients in a partial hospitalization program who had a diagnosis of schizophrenia or schizoaffective disorder participated in a 12-week weight control intervention (April to July of 2001). All had been taking an atypical antipsychotic for at least three months and had a BMI of at least 26 or had experienced a weight gain of at least 2.3 kg (five pounds) within two months of starting the medication.
All patient weight records from the partial hospitalization programs at the facility were reviewed. If weight records were available for the same time frame as the study period, the charts of these patients were retrospectively analyzed. A total of 15 of these patients were matched for weight collection time frame, age, BMI, diagnosis, and atypical antipsychotic medication and constituted the control group.
Measures included weight, BMI, attendance (participation in individual or group intervention activities), blood pressure, pulse, hunger, nutrition knowledge, and exercise level. Hunger was self-reported on a 5-point Likert scale, with higher scores indicating greater hunger. Exercise was measured as the number of days on which exercise occurred and the number of minutes of exercise. Nutrition knowledge was assessed with 16 multiple-choice questions. Attendance was used as a measure of treatment compliance.
The study participants underwent a screening evaluation, including a psychiatric clinical interview, a physical examination, screening laboratory tests, a comprehensive nutrition assessment, and a motivational assessment. The program incorporated nutrition counseling, exercise, and behavioral interventions designed to help the patients implement healthy lifestyle changes. Motivational counseling techniques (9) were used. Special teaching approaches for persons with cognitive deficits, such as repetition and homework, were used.
The participants attended two group sessions and one 15-minute individual session each week for a total of 25 visits over a 12-week period. One of the two weekly group sessions included teaching healthful weight management techniques, meal planning, label reading, food shopping and preparation, portion control, and healthy snacking. The other weekly group session focused on behavioral management techniques and principles of physical fitness. The patients were educated about developing a slower eating style and differentiating emotional from physiological hunger.
The participants were encouraged to undertake light or moderate exercise at least 20 minutes three to five times a week. Twice a week, an aerobic walking activity was incorporated into the group sessions. This activity consisted of intense sustained walking or an aerobic walking video class. Weekly weight changes and treatment goals were discussed during individual patient appointments.
Weight and BMI were assessed by using analysis of covariance (ANCOVA); baseline weight, BMI, and atypical medication dosage at first visit were used as covariates. For the purpose of this analysis, each patient's dosage of atypical antipsychotic medication was converted to risperidone equivalents and included as a covariate.
Hunger level, exercise level, blood pressure, pulse, and nutrition knowledge were analyzed for the intervention group with a two-tailed Student's t test. Compliance was tabulated for each visit and reported as mean percentage attendance. Data from the last observation were carried forward to the end point for all analyses.
Results
Demographic and clinical characteristics of the two groups are summarized in Table 1. Both groups tended to be obese: the mean BMI at baseline was 34.3 in the intervention group and 33.4 in the control group. Twenty-seven participants (87 percent) completed the 12-week program. Attendance was 77 percent for group sessions and 82 percent for individual sessions.
The patients in the intervention group lost an average of 2.7 kg (six pounds), or 2.7 percent of body weight, and those in the control group gained an average of 2.9 kg (6.4 pounds), or 3.1 percent of body weight. The difference in weight loss between groups was statistically significant. The corresponding change in the mean BMI was a drop from 34.32 to 33.34 (.98 points, or 2.8 percent) in the intervention group and an increase from 33.4 to 34.6 (1.2 points, or 3.6 percent) in the control group. This difference was also statistically significant.
Within the intervention group, significant improvements were noted in hunger rating, nutrition knowledge, and both days and minutes of exercise per week. Pulse and blood pressure did not change significantly.
Discussion
The results of this study demonstrate that patients of partial hospital programs who have schizophrenia or schizoaffective disorder can adhere to and benefit from an intensive weight control program. Whereas the patients in a matched control group continued to gain weight, those in the intervention group lost weight. The participants in the intervention group also showed statistically significant improvement in the amount of exercise they did, the amount of hunger they felt, and their knowledge about nutrition.
Although these results are encouraging, some limitations may apply. Participants were not randomly assigned to groups, and there may have been a selection bias in favor of those who were already motivated to lose weight. All participants in the weight control program, regardless of the atypical agent they were taking, were able to lose weight. However, the number of participants taking each agent was too small to test differences among them. Although the dosage of atypical drug is not clearly related to the risk of weight gain, we examined this variable by entering it as a covariate in the ANCOVA. The effect was nonsignificant.
An additional risk factor, not assessed in this study, is the potential weight gain effect of other medications. Several of the study participants were taking additional psychotropic agents that affect weight. Such medication use is difficult to control for in a treatment setting and constitutes another limitation of this study. Finally, an aggressive intervention such as the program we studied would be difficult to replicate in a private psychiatric office or in an outpatient program in which patients are seen once a month for medication management. Such an intervention is best suited to programs such as day hospital programs, long-term acute care settings, and some outpatient community mental health facilities.
Conclusions
Our data suggest that the weight management intervention was quite effective in this group of patients. A larger and longer randomized trial that examines a variety of issues, including the cost-effectiveness of intensive weight control programs, is warranted. Appropriate attention to this issue may prevent weight gain and promote weight loss, improve the quality of life for patients treated with antipsychotic drugs, and decrease morbidity and mortality due to weight-related disorders. On the basis of our results we believe that professionals treating persons who are taking atypical antipsychotics should educate patients and encourage them to engage in weight control activities.
Ms. Vreeland is affiliated with the University of Medicine and Dentistry of New Jersey (UMDNJ)-Robert Wood Johnson Medical School (RWJMS) departments of psychiatry and family medicine and the UMDNJ School of Nursing and with UMDNJ University Behavioral Health Care (UBHC) in Piscataway. Dr. Minsky and Dr. Stern are with the UMDNJ-RWJMS department of psychiatry and with UBHC. Dr. Menza is with the UMDNJ-RWJMS department of psychiatry. Ms. Rigassio Radler is with the UMDNJ School of Health-Related Professions in Newark. Dr. Roemheld-Hamm is with the UMDNJ-RWJMS department of family medicine in New Brunswick. Address correspondence to Ms. Vreeland at UMDNJ-UBHC, 151 Centennial Avenue, Suite 1500, Piscataway, New Jersey 08855 (e-mail, [email protected]).
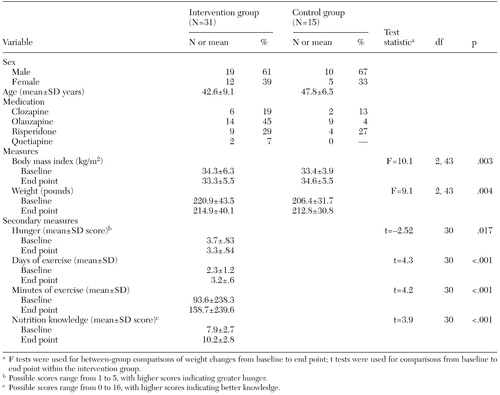 |
Table 1. Demographic and clinical characteristics of a sample of patients with schizophrenia or schizoaffective disorder who participated in a study of a weight control program
1. Allison DB, Mentore JL, Moonseong H, et al: Antipsychotic-induced weight gain: a comprehensive research synthesis. American Journal of Psychiatry 156:1686–1696, 1999Abstract, Google Scholar
2. Ganguli R: Weight gain associated with antipsychotic drugs. Journal of Clinical Psychiatry 60(suppl 21):20–24, 1999Medline, Google Scholar
3. Sacks GS, Guille C: Weight gain associated with use of psychotropic medications. Journal of Clinical Psychiatry 60(suppl 21):16–19, 1999Medline, Google Scholar
4. Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, Md, National Heart, Lung, and Blood Institute. Available at www.nhlbi.nih.gov/guidelines/obesity/ob_home.htm, July 1998Google Scholar
5. Ridgeway NA, Harvill DR, Harvill LM, et al: Improved control of type 2 diabetes mellitus: a practical education/behavior modification program in a primary care clinic. Southern Medical Journal 92:667–672, 1999Crossref, Medline, Google Scholar
6. Field AE, Coakley EH, Must A, et al: Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Archives of Internal Medicine 161:1581–1586, 2001Crossref, Medline, Google Scholar
7. Wirshing DA, Wirshing WC, Kysar L, et al: Novel antipsychotics: comparison of weight gain liabilities. Journal of Clinical Psychiatry 60:358–363, 1999Crossref, Medline, Google Scholar
8. Littrel KH, Petty RG, Hilligoss NM, et al: Educational interventions for the management of antipsychotic-induced weight gain. Presented at the annual meeting of the American Psychiatric Association, New Orleans, May 5–10, 2001Google Scholar
9. Miller WR, Rollnick S: Motivational Interviewing: Preparing People to Change Addictive Behaviors, 2nd ed. New York, Guilford, 2002Google Scholar



