Diagnostic Profiles Associated With Use of Mental Health and Substance Abuse Services Among High-Risk Youths
Abstract
This study examined use of mental health services by 947 high-risk youths in a publicly funded system of care to determine how single and comorbid diagnostic profiles (psychiatric and substance use disorders) were associated with use of a variety of types of formal and informal services. Use of professional services was most likely for youths with non-substance use psychiatric disorders, those with comorbid disorders, and those for whom high caregiver strain was reported. Use of informal services, such as peer support groups, was most likely for youths with substance use disorders, those with comorbid disorders, and those who had had police contact. Unmet need for mental health services was greatest among youth with substance use disorders only.
Underuse of mental health services by adolescents with psychiatric disorders is a significant public health problem (1). Youths who have had contact with public service sectors such as child welfare, juvenile justice, and mental health services are a particularly high-risk group with elevated rates of psychiatric disorders (2,3). These youths have relatively high rates of mental health service use, but little is known about what types of services are used by youths with different diagnostic profiles.
Adults with psychiatric comorbidity—the co-occurrence of a substance use disorder with another psychiatric disorder—are more likely to use mental health services than those with a single diagnosis (4), but this relationship has not been demonstrated among youths. The purpose of this study was to examine how single and comorbid diagnostic profiles are associated with the use of a variety of mental health services among youths in public service sectors; the study controlled for the effects of other sociodemographic and family variables known to predict service use, including age, gender, race, caregiver strain, and police contact.
Methods
Participants
Participants were a subgroup of all youths whose cases were active in one or more of five San Diego County public sectors of care—child welfare, juvenile justice, special education, alcohol and drug, and mental health—from January through June 1997. Interviews were completed between October 1997 and February 1999, and complete data were obtained for 1,715 (66 percent) of the eligible sample (3). The 947 participants were aged 13 to 18 years.
Sample weights were assigned to represent the original sample of all youths in the system of care. All numbers reported reflect actual numbers available for analysis; percentages reflect sample weighting procedures.
Of the study subsample of 947, a total of 628 youths (66 percent) were male. The mean±SD age was 15.9±1.6 years. The racial and ethnic distribution was 341 (33 percent) Caucasian, 272 (32 percent) Latino, 194 (21 percent) African American, 75 (8 percent) Asian American or Pacific Islander, and 65 (7 percent) multiracial or other.
Procedure and measures
To assess past-year psychiatric disorders, youths and their parents were interviewed individually with the youth and parent reports of the Diagnostic Interview Schedule for Children (DISC-IV) (5). The youths were assessed for substance use disorders with the youth report of the Composite International Diagnostic Interview—Substance Abuse Module (CIDI-SAM). Youths were assessed for functional impairment with the Children's Global Assessment Scale and the Columbia Impairment Scale. Youths and their parents were interviewed about service use with the parent and youth reports of the Services Assessment for Children and Adolescents (SACA) (6). Parents were administered the Caregiver Strain Questionnaire (7).
Youths were classified into five diagnostic groups: comorbid psychiatric and substance use disorders (N=174), psychiatric disorder only (N=385), substance use disorder only (N=58), no diagnosis with functional impairment (N=143), and no diagnosis and no functional impairment (N=187). Within each group that had a diagnosis, youths could have multiple diagnoses; for example, youths in the group with psychiatric disorders only could have multiple non-substance use diagnoses.
Mental health services were classified into three groups: professional outpatient, 24-hour care, and informal. Professional outpatient included visits to a professional psychologist, counselor, mental health clinic, day treatment program, and alcohol-drug treatment facility; visits to a pediatrician, another type of M.D., and the emergency department; and in-home therapy for emotional or behavioral reasons. Included in 24-hour care were psychiatric hospitalization and a residential treatment center or group home. Informal services included peer counseling, support groups, and alternative healers. Two summary categories were created: any professional care, which included professional outpatient and 24-hour care; and any service, which included all professional and informal services.
Chi square analyses tested for significant differences in service use rates across diagnostic groups. Multiple logistic regression analyses tested whether these differences remained when the analysis controlled for the effects of potential confounders such as sociodemographic characteristics and caregiver strain. All analyses were conducted with STATA, version 7.0, with data weighted to represent the system-of-care population.
Results
Rates of service use were high: 693 youths (70 percent) received some kind of service, including informal services such as peer support. Significant differences were found across diagnostic groups in rates of use of any service and in use of each category of service except 24-hour care. Youths with psychiatric disorders, with or without comorbid substance use disorders, were most likely to receive any service and to receive professional outpatient services. For example, of the 385 youths with only psychiatric disorders, 273 (70 percent) received outpatient services, whereas, of the 58 youths with only substance use disorders, 29 (46 percent) received outpatient services, including substance abuse treatment.
Youths with substance use disorders, with and without comorbid psychiatric disorders (N=232), were most likely to receive informal services: 106 (46 percent) of these youths received such services. In comparison, of the 385 youths with only psychiatric disorders, 72 (17 percent) received informal services. Unmet need was greatest for youths with substance use disorders only: 22 (37 percent) of that group did not receive any type of mental health service, compared with 26 (19 percent) of those with comorbidity and 79 (23 percent) of those with psychiatric disorders only.
Table 1 shows that diagnostic group had a significant association with the likelihood of use of professional outpatient, informal, and any mental health service after the effects of other potential confounders were controlled for. For example, youths with comorbid psychiatric and substance use disorders were significantly more likely to receive outpatient services than were those with no diagnosis and no impairment. Other significant predictors of outpatient service use included younger age, female sex, white race, high caregiver strain, and no police contact. Diagnoses were not significantly associated with 24-hour care, but female sex, high caregiver strain, and contact with the alcohol, drug, or mental health service sectors did predict such use. Significant predictors of the use of informal services were older age, police contact, comorbid diagnoses, and diagnosis of substance use disorder only. Predictors of any service use included female gender, white race, no police contact, high caregiver strain, comorbid diagnoses, and psychiatric diagnoses only. Youths with substance use disorders only were no more likely to use a mental health service than those with no diagnosis and no impairment.
Discussion
Service use rates in this high-risk sample are much higher than for community samples of youths (1), but significant discrepancies by diagnostic profile were found. Youths with non-substance use psychiatric disorders were likely to receive professional mental health services, whether or not they also had a substance use disorder. Use of professional services by youths with psychiatric disorders only and youths with comorbid disorders were equivalent; thus having a comorbid substance use disorder did not significantly elevate the likelihood of receiving mental health services. It is a matter for concern that 46 (30 percent) of those with comorbid disorders did not receive any professional services, given that these youths are at high risk for maladaptive outcomes (8).
Unmet need for services was greatest for the 58 youths with a substance use disorder only. They were most likely to receive informal services, but 29 (55 percent) received no formal services and 22 (37 percent) received no services at all. Given that these youths had substance abuse problems serious enough to meet DSM-IV criteria, it is a matter for concern that so many were receiving no treatment. In addition, the effectiveness of informal services, such as 12-step programs, for youths is debatable (9).
One finding, consistent with much of the literature, was that one of the strongest predictors of use of professional services was parents' reported objective and subjective burden in caring for their child (7). However, caregiver strain did not predict the use of informal services; the strongest predictor was police contact, which was significantly associated with a lower likelihood of professional outpatient service use. Apparently the juvenile justice system prefers to refer youths to peer support services.
Conclusions
Equitable and efficient delivery of effective mental health services to youths with psychiatric disorders is essential for reducing individual and societal costs as these youths age into adulthood. Discrepancies in service use such as those identified here should be addressed by more aggressive outreach and training for "gateway providers" in multiple service sectors to improve identification and referral (10). Of particular concern is the apparent lack of attention to youths with substance use disorders. More research on the complex processes of problem identification, help seeking, and referral is needed to identify the greatest barriers to service use.
Acknowledgments
The data are from the Patterns of Youth Mental Health Care in Public Service Systems Study, which is supported by National Institute of Mental Health grant U01-MH-55282 to Dr. Hough. Preparation of this article was supported by National Institute of Mental Health grant K01-MH-01544 to Dr. Garland.
The authors are affiliated with the Child and Adolescent Services Research Center of Children's Hospital and Health Center, 3020 Children's Way (MC 5033), San Diego, California 92123 (e-mail, [email protected]). Dr. Garland, Dr. Aarons, Dr. Brown, and Dr. Hough are also with the department of psychiatry at the University of California, San Diego.
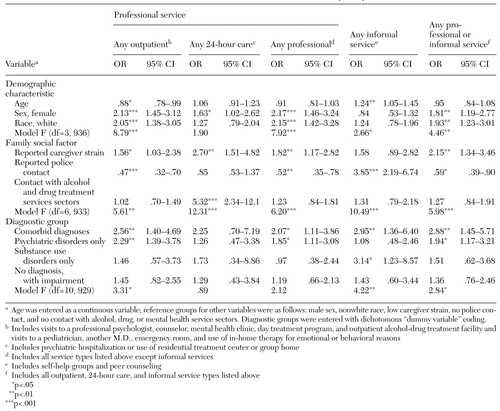 |
Table 1. Associations between model variables and the use of public mental health services by 947 youths
1. Leaf PJ, Alegria M, Cohen P, et al: Mental health service use in the community and schools: results from the four-community MECA study. Journal of the American Academy of Child and Adolescent Psychiatry 35:889-897, 1996Crossref, Medline, Google Scholar
2. Aarons GA, Brown SA, Hough RL, et al: Prevalence of substance use disorders among adolescents in public sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry 40:419-426, 2001Crossref, Medline, Google Scholar
3. Garland AF, Hough RL, McCabe KM, et al: Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry 40:409-418, 2001Crossref, Medline, Google Scholar
4. Wu L, Kouzis AC, Leaf PJ: Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. American Journal of Psychiatry 156:1230-1236, 1999Abstract, Google Scholar
5. Shaffer D, Fisher P, Lucas CP, et al: NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry 39:28-38, 2000Crossref, Medline, Google Scholar
6. Horwitz SM, Hoagwood K, Stiffman AR, et al: Reliability of the Services Assessment for Children and Adolescents. Psychiatric Services 52:1088-1094, 2001Link, Google Scholar
7. Brannan AM, Heflinger GA, Bickman L: The Caregiver Strain Questionnaire: measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders 5:212-222, 1997Crossref, Google Scholar
8. Brown SA, Gleghorn AA, Schuckit MA, et al: Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol 57:314-324, 1996Crossref, Medline, Google Scholar
9. Kelly JF, Myers MG, Brown SA: A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychology of Addictive Behaviors 14:376-389, 2000Crossref, Medline, Google Scholar
10. Stiffman A, Hadley-Ives E, Dore P, et al: Youths' access to mental health services: the role of providers' training, resource connectivity, and assessment of need. Mental Health Services Research 2:141-154, 2000Crossref, Medline, Google Scholar



