Disability Compensation Seeking Among Veterans Evaluated for Posttraumatic Stress Disorder
Abstract
OBJECTIVE: This study sought to further examine the relationship between compensation-seeking status and reporting of symptoms among combat veterans who were evaluated for posttraumatic stress disorder (PTSD). METHODS: Archival data were drawn for 320 adult male combat veterans who were consecutively evaluated at a Department of Veterans Affairs (VA) PTSD outpatient clinic from 1995 to 1999. The veterans were compared on variables from their clinical evaluation, including diagnostic status and self-report measures such as the Minnesota Multiphasic Personality Inventory-2, which includes scales designed to detect feigned or exaggerated psychopathology. RESULTS: Compensation-seeking veterans reported significantly more distress across domains of psychopathology, even after the effects of income had been controlled for and despite an absence of differences in PTSD diagnoses between groups. However, compensation-seeking veterans also were much more likely to overreport or exaggerate their symptoms than were non-compensation-seeking veterans. CONCLUSIONS: This study provided further evidence that VA disability compensation incentives influence the way some veterans report their symptoms when they are being evaluated for PTSD. These data suggest that current VA disability policies have problematic implications for the delivery of clinical care, evaluation of treatment outcome, and rehabilitation efforts within the VA.
People who suffer from severe mental illnesses often experience occupational impairment and related financial hardships (1,2,3,4). Military veterans may apply for service-connected disability payments for any physical or psychiatric condition that first occurred during or was caused by their military service and that impairs their ability to earn a living, including posttraumatic stress disorder (PTSD).
There is a growing trend in the Department of Veterans Affairs (VA) system for veterans to seek such payments. Recent data show that Gulf War veterans draw disability compensation at a much higher rate than veterans of any previous conflict and at almost twice the current rate of World War II veterans (16 percent compared with 8.6 percent) (5). Furthermore, 69 to 94 percent of veterans who seek treatment for PTSD in the VA system apply for psychiatric disability (6,7,8). Evidence suggests that evaluation of PTSD symptoms in this population may be influenced by the substantial financial incentive for veterans to present as socially and occupationally impaired. Given that lifetime prevalence of PTSD among combat veterans is between 9 percent and 31 percent (9,10), this issue is highly relevant to the VA system in terms of both clinical care and disability policy.
Background
In 1996, total compensation and pension expenditures for the VA were estimated to be just over $18 billion, with 2.2 million of the surviving 25.4 million veterans (8.9 percent) receiving some level of service-connected disability benefits (11). If disability status is granted, a rating of severity of disability is made on a scale of zero to 100 percent. The relationship between disability payments and disability ratings is curvilinear, and many benefits—for example, some medical and dental coverage—do not begin until the veteran receives a rating of 100 percent. Even veterans who are rated as 90 percent disabled stand to benefit significantly when their rating increases to 100 percent.
When disability claims are denied or are only partially granted, veterans may appeal the decision an indefinite number of times. These repeat claims outnumber original claims almost three to one and dominate the VA adjudication and appeals system. Veterans who are granted disability compensation must undergo continuing disability review, usually every other year, to determine whether they continue to be eligible for disability payments.
For many veterans who have chronic illnesses, the process of obtaining and maintaining disability payments is a protracted struggle. However, the financial incentives are significant. For example, in South Carolina, where per capita income is about $17,000 before taxes, a single veteran without dependents who was 100 percent service connected in 1999 received an annual tax-free income of $23,868, in addition to other benefits (11).
Studies consistently demonstrate that combat veterans who are evaluated for PTSD in the VA system exhibit extreme and diffuse levels of psychopathology across instruments that measure different domains of mental illness and extreme elevations on the validity scales of the Minnesota Multiphasic Personality Inventory (MMPI) in the direction of overreporting (12,13). These validity scales—for example, the F-K index—take into account the stereotypes held by many lay people who assume that serious mental illnesses involve a large number of bizarre symptoms, such that high scores indicate endorsement of items that are rarely endorsed even by persons with the most severe mental illness. An in-depth discussion of how these validity scales were developed, what they mean, and how they should be applied to veterans has been published elsewhere (14).
Combat veterans also are prone to inflating their reports of combat exposure over time (15). This general reporting pattern significantly complicates the assessment of symptoms for the purposes of both diagnostic decision making and evaluation of treatment outcome and frequently casts doubt on the credibility of symptom reports (13). We have previously discussed possible explanations for this pattern (13), including co-occurrence of symptoms, a "cry for help," a sociological phenomenon known as Vietnam syndrome, and the influence of systemic variables within the VA.
Some researchers have speculated that the phenomenon of apparent symptom overreporting may reflect the motivation of veterans to present as severely disabled in order to obtain disability compensation (16,17). Several studies have examined the influence of compensation-seeking status on symptom reporting patterns by using self-report measures of psychopathology. Although two early studies had mixed results (18,19), their conclusions were limited by the manner in which compensation seeking was defined and in how the study participants were grouped for analysis.
Accurately understanding the role of compensation-seeking status requires a definition of "compensation seeking" that maximally differentiates persons who have financial incentives from those who do not. Two studies examined this issue by differentiating veterans on the basis of financial incentive (7,8). Veterans were classified into two groups at the time of evaluation. Compensation-seeking veterans were those who were currently seeking or planning to seek VA disability compensation or increases in existing disability payments for PTSD. Non-compensation-seeking veterans were those who were not intending to seek VA disability compensation for their PTSD symptoms.
The proportion of veterans who were classified as compensation seeking in each of these two studies was identical at 69 percent. Compensation-seeking veterans received significantly higher pathological scores on clinical measures and obtained much higher elevations on MMPI validity scales associated with symptom exaggeration and malingering than did non-compensation-seeking veterans. These results were obtained despite the fact that the two groups did not differ in the frequency of PTSD diagnoses. Furthermore, differences on most indexes exceeded effect sizes of 1.0, even when the effects of income, Global Assessment of Functioning (GAF) scores, and clinician-rated severity of PTSD were controlled for.
Evidence also suggests that the MMPI validity scales can be used to identify veterans who may be exaggerating their psychopathology in order to gain disability compensation. Specifically, veterans with F-K indexes of more than 13 were not significantly more likely to be seeking compensation (20), whereas those with F-K indexes of more than 22 were, and they scored much higher on self-report measures of psychopathology despite having lower rates of PTSD diagnoses and similar rates of other psychiatric diagnoses (21). (Possible scores on the F-K index range from −30 to 60, with higher scores indicating greater symptom exaggeration or malingering.) These data suggest that the availability of disability benefits influences the way in which veterans present their difficulties. This conclusion is consistent with evidence that persons from other compensation-seeking populations—for example, injury and pain litigants—also tend to overreport symptoms (22).
The study reported here used archival data to further examine the relationship between compensation-seeking status and symptom reporting among combat veterans who were evaluated for PTSD. Specifically, we were interested in comparing the symptom reports of combat veterans who were seeking compensation for any type of disability with the reports of those who were not seeking such compensation. We hypothesized that differences consistent with the results of previous research would be demonstrated between these two groups.
Methods
Participants
Archival data were drawn for 320 male combat veterans aged 18 years or older who were consecutively evaluated at a VA PTSD outpatient clinic from 1995 to 1999. The study was conducted after approval had been obtained from an institutional review board, including a waiver of the requirement for obtaining informed consent. Compensation-seeking status was obtained through interviews, chart reviews, and self-report items included in a psychosocial history questionnaire. Study participants were classified as compensation seekers if they had already applied or were planning to apply for any type of VA disability compensation. Participants were classified as non-compensation seekers if they were not intending to apply for any type of VA disability compensation.
Data on compensation-seeking status were available for 193 veterans (60 percent), including 143 compensation seekers (74 percent) and 50 non-compensation seekers (26 percent). Our experience with the PTSD clinic suggests that the lack of data for 40 percent of the total sample was due to changes and fluctuations in procedures for conducting evaluations over time rather than the result of any systematic source of bias or error. However, we conducted statistical analyses to compare veterans for whom compensation-seeking status was available with veterans for whom it was not. The rate of disability seeking was 5 percent higher than in previous studies, which have focused specifically on compensation seeking for PTSD (7,8).
Procedure and instruments
Psychiatric diagnoses were based on DSM-IV (23). All PTSD diagnoses were determined on the basis of team consensus (a psychiatrist, a clinical psychologist, and a social worker) after a thorough evaluation, including a chart review, psychosocial and military history interviews, and the Clinician-Administered PTSD Scale (CAPS-1), a structured clinical PTSD interview (24).
Additional clinical information was obtained by using a battery of self-report measures, including the Minnesota Multiphasic Personality Inventory-2 (MMPI-2), a widely used 567-item true-false questionnaire that assesses a wide range of domains related to psychopathology and test-taking attitude, including scales designed to detect feigned or exaggerated psychopathology (25); the Beck Depression Inventory (BDI), a widely used, well-validated, 21-item self-report measure of depressive symptoms (26); the Dissociative Experiences Scale (DES), a 28-item self-report measure of dissociative symptoms (27), with a behaviorally anchored, fixed response format (DES-FRF) found to have good alternate form reliability (r=.71) with the original DES, strong internal consistency (alpha=.95), and a significantly lower inverse relationship with intelligence (r=−.18) compared with the original DES (r=−.42) (28); and the Mississippi Combat PTSD Scale (M-PTSD), a 35-item Likert-scale measure of combat-related PTSD symptoms that has been widely used and has strong psychometric properties (29).
Statistical analyses
Because compensation-seeking status was available for only 60 percent of the veterans in our archival data set, we first conducted multivariate analyses of variance and chi square tests to compare clinical and demographic characteristics of veterans for whom compensation-seeking status was available and those for whom it was not. These analyses were conducted to ensure that there were no obvious sources of systematic bias in the way in which this variable was assessed or reported.
Analyses were then conducted to determine whether there were any demographic differences between the two groups. For continuous-scaled variables, t tests for independent samples were used; robust t tests were used when group variances were not equal—that is, when Levene's test of equal variances was significant at p<.05. Test-taking attitude was used to screen out data from veterans who completed the MMPI-2 in a grossly invalid manner, such as engaging in mostly true or mostly false responding (true response inconsistency [TRIN]>100), random responding (variable response inconsistency [VRIN]>80), or missing responses (more than 15 items left blank). These criteria resulted in the exclusion of 17 compensation-seeking and five non-compensation-seeking veterans. Thus 171 veterans (126 compensation seekers and 45 non-compensation seekers) were included in the study.
Three separate one-way multivariate analyses of covariance (MANCOVAs) were conducted to compare the two groups on MMPI-2 scales, of which all adjusted for the covariate of income, which was the single demographic variable found to be different between the two groups. The groups were first compared on the ten MMPI-2 K-corrected clinical scale raw scores, then on the 15 MMPI-2 content scale raw scores, and finally on three MMPI-2 raw-scored validity (overreporting, or "fake-bad") scales designed to detect feigned psychopathology (the F, the Fp, and the F-K index).
Individual MANCOVA alpha levels of .05 were implemented for testing effects, using Wilks' lambda statistic. Significant multivariate effects were followed by univariate tests to assess which particular scales differentiated groups (alpha=.01, to control for multiple comparisons). As an additional method of exploring the relationship between compensation-seeking status and validity scale scores, a 2 × 2 chi square analysis was conducted to test the hypothesis that extreme exaggeration (an Fp score greater than 7) would be more likely than nonexaggeration (an Fp score less than 2) for the purposes of seeking VA disability compensation (25,30).
Next, three separate analyses of covariance (ANCOVAs) were conducted to compare compensation-seeking veterans and non-compensation-seeking veterans on other self-report measures, adjusting for income. Separate ANCOVAs used scores on the BDI, the M-PTSD, and the DES-FRF as dependent variables. An alpha level of .01 was set for these analyses to control for multiple comparisons.
Last, a sequential logistic regression analysis was implemented to examine whether there was a relationship between compensation-seeking status and the presence of a PTSD diagnosis, with income controlled for. First, income was tested for its possible effect on disability status. PTSD diagnosis was subsequently entered to determine whether it had an effect on disability status beyond that accounted for by income. In a separate logistic regression analysis, PTSD diagnosis was entered first, followed by income to assess whether income had a significant effect on disability status beyond that achieved by PTSD diagnosis.
Results
The statistical analyses that compared veterans for whom compensation-seeking status was available with veterans for whom it was not showed no significant between-group differences on any clinical self-report measures, diagnostic rates, or demographic variables. This finding was consistent with our expectation that there would be no obvious sources of systematic bias in the way in which the variable compensation-seeking status was assessed or reported in our archival data set.
The mean±SD age of the compensation-seeking veterans was 49.01± 5.80 years, and the mean age of the non-compensation-seeking veterans was 50.22±8.18 years; no significant difference was observed between the two groups. Veterans in the compensation-seeking group had an average of 12.39±2.25 years of education, compared with 12.27±2.53 in the non-compensation-seeking group, and there was no significant difference between the two groups. The average annual income of the compensation-seeking group was $17,649.83± 17,217.36, compared with $25,011.32± 17,747.11 in the non-compensation-seeking group; the difference between the two groups was significant (t=−.25, df=161, p<.05). Groups were also compared by using chi square analyses on nominal-scaled demographic variables, including ethnicity, relationship and employment status, branch of military service, and era of war served, of which none yielded significant between-group differences (Table 1).
The results of the MANCOVAs that compared compensation-seeking and non-compensation-seeking veterans on the MMPI-2 clinical scales, adjusted for income, are summarized in Table 2. Overall, the difference between the two groups was significant (F=2.09, df=10, 126, p<.05). Compensation-seeking veterans scored significantly higher on scales that measured health concerns, depression, somatization, anger and hostility, paranoid ideation, anxiety and obsessive rumination, difficulties thinking and concentrating, and social introversion.
The results of the MANCOVAs that examined the MMPI-2 content scales are also shown in Table 2. Overall, the difference between the two groups was significant (F=2.67, df=15, 121, p<.05). Compensation-seeking veterans scored significantly higher on scales that measured anxiety, obsessive rumination, depression, health concerns, bizarre thought processes, cynicism, low self-esteem, family discord, work interference, and negative treatment indicators.
A significant difference between the groups was also noted in the MANCOVAs that examined differences on the MMPI-2 validity (overreporting) scales (overall F=3.54, df=3, 133, p<.05). The compensation-seeking group obtained higher scores on all three scales (Table 2). The 2 × 2 chi square analysis exploring the relationship between compensation-seeking status and Fp classification of extreme exaggeration versus nonexaggeration was significant (χ2=5.25, df=1, N=162, p<.05), with significantly more compensation-seeking veterans classified as extreme exaggerators.
The ANCOVA results shown in Table 3 demonstrate that, with adjustment for income, compensation-seeking veterans obtained significantly higher scores on the BDI, the DES-FRF, and the M-PTSD.
The results of the logistic regression analysis are shown in Table 4. With income controlled for, no significant relationship was apparent between compensation-seeking status and the presence of a PTSD diagnosis. When income was entered into the regression model first, PTSD diagnosis did not predict compensation-seeking status beyond that predicted by income alone. When PTSD diagnosis was entered first, income was a significant predictor of disability status beyond the contribution of PTSD diagnosis alone.
Discussion
This study examined symptom reporting patterns among two groups of combat veterans who were evaluated for PTSD: those who were seeking compensation for any type of VA disability and those who were not. Overall, veterans who were seeking compensation obtained significantly higher pathological scores on a variety of self-report measures of psychopathology, including most clinical and content scales of the MMPI-2 and other measures of depression, dissociation, and PTSD symptom severity. This was true even when the effects of income—the sole demographic variable that proved to be significantly different between the two groups—was controlled for.
However, compensation-seeking veterans also evidenced greater elevations than non-compensation-seeking veterans on primary validity scales of the MMPI-2 (31) and were significantly more likely to be classified as extreme exaggerators. Thus it appears that veterans who were seeking compensation were much more likely to overreport or exaggerate their symptoms than those who were not seeking compensation. This pattern of differences closely resembles those found in previous studies that compared veterans who were specifically seeking compensation for PTSD-related disability with non-compensation-seeking veterans (7,8), although the effects we found in our study were somewhat smaller.
Implications
Clinical care. The specter of disability payments may affect clinical care in several ways. Exaggeration of symptoms complicates differential diagnosis and the development of appropriate treatment plans. Furthermore, the effectiveness of treatment may be undermined in that the contingencies of the system reward illness behaviors and the maintenance of symptoms. Experience suggests that many patients acknowledge using treatment sessions as a means of documenting, through clinicians' progress reports, their psychiatric difficulties. The provision of permanent disability payments may also foster the harmful notion that recovery from PTSD or successful management of symptoms is not possible.
Clinicians in VA practice settings should expect that many veterans will present with unrealistic pictures of their symptoms, but such behavior should not necessarily be taken as evidence of malingering. If the MMPI-2 is used, traditional cutoff points on the validity scales (F-K scores greater than 13) may not be appropriate. Instead, population-specific cutoff points (F-K scores greater than 22) should be considered (20). On the other hand, careful follow-up evaluation of veterans who overreport their symptoms is warranted, including careful assessment of military documentation, structured interviews, and perhaps even psychophysiological assessment.
Treatment outcome research. The evaluation of treatment outcome results in clinical trials is a related area of concern. Treatment efficacy data for combat-related PTSD are currently lacking. Furthermore, in many studies PTSD treatment effect sizes were larger in nonveteran samples than among veterans (32). This observation may be at least partially attributed to the overreporting response pattern and the reluctance of many veterans to acknowledge therapeutic gains because they have financial incentives not to do so.
Although there have been few direct empirical studies of this hypothesized association between compensation seeking and treatment, several studies have had results that deserve mention. One study found that veterans who were classified on the MMPI as "symptom overreporters" were less likely to manifest improvement after six weeks of partial hospitalization, even though clinicians did not consider them to be more dysfunctional than other veterans before treatment (33). In addition, several treatment outcome studies showed disparities between veterans' extreme self-reported symptom patterns and other data collected through clinicians' ratings, psychophysiological measures, and daily symptom frequency counts (34,35,36). Finally, data from a study of veterans who were treated for PTSD within the VA system indicated that compensation-seeking status had a significant treatment effect among inpatient veterans, although no such effect was found among outpatient veterans (6).
Future research directions. Veterans who have PTSD often experience severe psychiatric, medical, social, and occupational impairment that results in persisting financial hardships. They therefore require and deserve appropriate assistance in these areas. However, our understanding of the influence of veterans' disability compensation seeking on their use of medical, rehabilitative, and cash assistance programs remains undeveloped. Further research is needed to better understand how compensation-seeking status influences the evaluation of treatment outcome; to explore the relationship between disability, compensation seeking, and the use of general medical services in the VA health care system (37) and the interface with other disability providers, such as Social Security Disability Insurance (38); to test the effectiveness of state-of the-art supported employment services (39,40,41), an innovative advance over standard vocational rehabilitation services offered by the VA whose effectiveness for persons with severe PTSD has been very poor (42,43); and to better understand the costs associated with federal disability policies and different VA disability evaluation strategies, which meet the moral imperative of reintegrating very ill, disabled, indigent, and isolated veterans into mainstream community life (44,45,46).
Conclusions
This study provided further evidence that VA disability compensation incentives may influence the way some veterans report their symptoms when they are being evaluated for PTSD. Although there were no differences in the frequency of PTSD diagnoses between the veterans in this study who were seeking compensation and those who were not, the compensation-seeking veterans reported significantly more distress across domains of psychopathology. Yet veterans who sought compensation were also much more likely to overreport or exaggerate their symptoms than those who were not seeking compensation. These data suggest that current VA disability policies have problematic implications for the delivery of clinical care, evaluation of treatment outcome, and rehabilitation efforts within the VA.
Acknowledgments
This work was partially supported by grants MH-01660 and MH-61983 from the National Institute of Mental Health to Dr. Frueh. The study was also supported by the Office of Research and Development, Medical Research Service, Department of Veterans Affairs.
Dr. Frueh, Dr. Elhai, Dr. Gold, Dr. Monnier, Dr. Magruder, and Dr. Arana are affiliated with the Veterans Affairs Medical Center in Charleston, South Carolina, and the department of psychiatry and behavioral sciences at the Medical University of South Carolina in Charleston. Dr. Keane is with the National Center for PTSD of the Veterans Affairs Medical Center in Boston and with Boston University School of Medicine. Send correspondence to Dr. Frueh at the Mental Health Service (116), Veterans Affairs Medical Center, 109 Bee Street, Charleston, South Carolina 29401-5799 (e-mail, [email protected]).
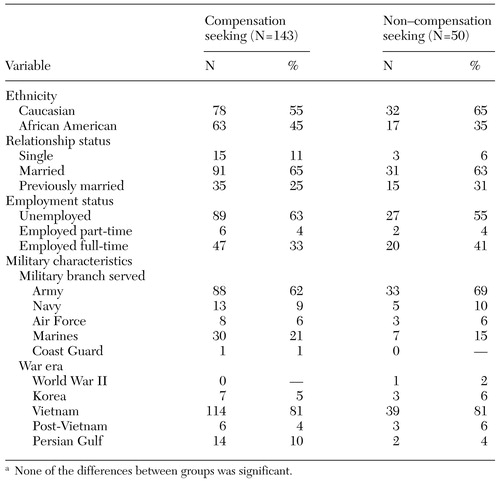 |
Table 1. Demographic characteristics of compensation-seeking and non-compensationseeking veteransa
a None of the differences between groups was significant.
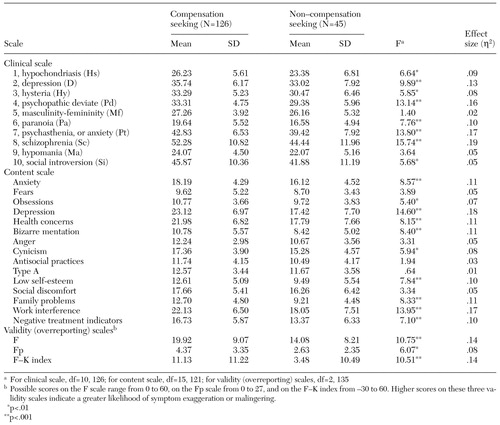 |
Table 2. Results of multivariate analyses of covariance for the clinical and content scales of the Minnesota Multiphasic Personality Inventory-2 for compensation-seeking and non-compensation-seeking veterans
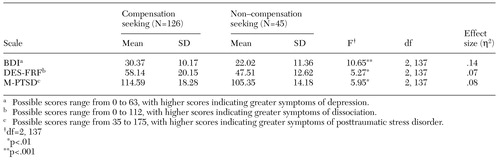 |
Table 3. Results of analyses of covariance for the Beck Depression Inventory (BDI), the Dissociative Experiences Scale, fixed-response format (DES-FRF), and the Mississippi Combat PTSD Scale (M-PTSD) for compensation-seeking and non-compensation-seeking veterans
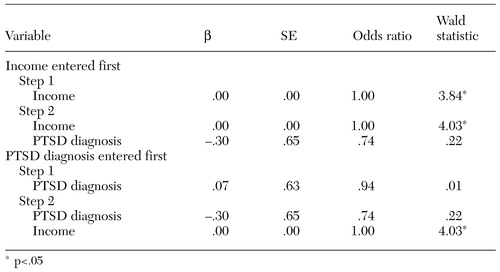 |
Table 4. Results of sequential logistic regression analyses for income and diagnosis of posttraumatic stress disorder (PTSD) in predicting compensation-seeking status among 132 veterans
1. Berndt ER, Koran LM, Finkelstein SN, et al: Lost human capital from early-onset chronic depression. American Journal of Psychiatry 157:940-947, 2000Link, Google Scholar
2. Drake RE, McHugo GJ, Bebout RR, et al: A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Archives of General Psychiatry 56:627-633, 1999Crossref, Medline, Google Scholar
3. Kouzis AC, Eaton WW: Psychopathology and the initiation of disability payments. Psychiatric Services 51:908-913, 2000Link, Google Scholar
4. Petrila J, Brink T: Mental illness and changing definitions of disability under the Americans With Disabilities Act. Psychiatric Services 52:626-630, 2001Link, Google Scholar
5. Gulf War veterans draw disability compensation at a higher rate than those from any other conflict. Wall Street Journal, Oct 27, 1999, p A1Google Scholar
6. Fontana A, Rosenheck R: Effects of compensation seeking on treatment outcomes among veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease 186:223-230, 1998Crossref, Medline, Google Scholar
7. Frueh BC, Smith DW, Barker SE: Compensation seeking status and psychometric assessment of combat veterans seeking treatment for PTSD. Journal of Traumatic Stress 9:427-439, 1996Crossref, Medline, Google Scholar
8. Frueh BC, Gold PB, de Arellano MA: Symptom overreporting in combat veterans evaluated for PTSD: differentiation on the basis of compensation seeking status. Journal of Personality Assessment 68:369-384, 1997Crossref, Medline, Google Scholar
9. Centers for Disease Control and Prevention: Health status of Vietnam veterans. JAMA 259:2701-2724, 1988Crossref, Medline, Google Scholar
10. Kulka RA, Schlenger WE, Fairbank JA, et al: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
11. Oboler S: Disability evaluations under the Department of Veterans Affairs, in Impairment Rating and Disability Evaluation. Edited by Rondinelli RD, Katz RT. Philadelphia, Saunders, 2000Google Scholar
12. Fairbank JA, Keane TM, Malloy PF: Some preliminary data on the psychological characteristics of Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 51:912-919, 1983Crossref, Medline, Google Scholar
13. Frueh BC, Hamner MB, Cahill SP, et al: Apparent symptom overreporting among combat veterans evaluated for PTSD. Clinical Psychology Review 20:853-885, 2000Crossref, Medline, Google Scholar
14. Elhai JD, Ruggerio KJ, Frueh BC, et al: The infrequency-postraumatic stress disorder scale (Fptsd) for the MMPI-2: development and initial validation with veterans presenting with combat-related PTSD. Journal of Personality Assessment 79:541-559, 2002Crossref, Google Scholar
15. Southwick SM, Morgan CA, Nicolaou AL, et al: Consistency of memory for combat-related traumatic events in veterans of Operation Desert Storm. American Journal of Psychiatry 154:173-177, 1997Link, Google Scholar
16. Atkinson RM, Henderson RG, Sparr LF, et al: Assessment of Vietnam veterans for posttraumatic stress disorder in Veterans Administration disability claims. American Journal of Psychiatry 139:1118-1121, 1982Link, Google Scholar
17. Lees-Haley PR: Malingering post-traumatic stress disorder on the MMPI. Forensic Reports 2:89-91, 1989Google Scholar
18. Schneider SJ: Disability payments for psychiatric patients: is patient assessment affected? Journal of Clinical Psychology 35:259-264, 1979Google Scholar
19. Jordan RG, Nunley TV, Cook RR: Symptom exaggeration in a PTSD inpatient population: response set or claim for compensation? Journal of Traumatic Stress 5:633-642, 1992Google Scholar
20. Smith DW, Frueh BC: Compensation seeking, comorbidity, and apparent exaggeration of PTSD symptoms among Vietnam combat veterans. Psychological Assessment 8:3-6, 1996Crossref, Google Scholar
21. Gold PB, Frueh BC: Compensation-seeking and extreme exaggeration of psychopathology among combat veterans evaluated for PTSD. Journal of Nervous and Mental Disease 187:680-684, 1999Crossref, Medline, Google Scholar
22. Rothke SE, Friedman AF, Dahlstrom WG, et al: MMPI normative data for the F-K index: implications for clinical, neuropsychological, and forensic practice. Assessment 1:1-15, 1994Crossref, Medline, Google Scholar
23. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
24. Blake DD, Weathers FW, Nagy LN, et al: A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behavior Therapist 18:187-188, 1990Google Scholar
25. Greene RL: The MMPI-2: An Interpretive Manual. Boston, Allyn and Bacon, 2000Google Scholar
26. Beck AT, Steer RA, Garbin MG: Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review 8:77-100, 1988Crossref, Google Scholar
27. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease 174:727-735, 1986Crossref, Medline, Google Scholar
28. Frueh BC, Johnson DE, Smith DW, et al: A potential problem with the response format of the Dissociative Experiences Scale: a significant correlation with intelligence among combat veterans with PTSD. Journal of Traumatic Stress 9:651-656, 1996Crossref, Medline, Google Scholar
29. Keane TM, Caddell JM, Taylor KL: Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. Journal of Consulting and Clinical Psychology 56:86-90, 1988Crossref, Google Scholar
30. Arbisi PA, Ben-Porath YS: An MMPI-2 infrequent response scale for use with psychopathological populations: the infrequency psychopathology scale, F(p). Psychological Assessment 7:424-431, 1995Crossref, Google Scholar
31. Rogers R, Sewell KW, Salekin RT: A meta-analysis of malingering on the MMPI-2. Assessment 1:227-237, 1994Crossref, Google Scholar
32. Hidalgo R, Hertzberg MA, Mellman T, et al: Nefazadone in post-traumatic stress disorder: results from six open-label trials. International Clinical Psychopharmacology 14:61-68, 1999Crossref, Medline, Google Scholar
33. Perconte ST, Griger ML: Comparison of successful, unsuccessful, and relapsed Vietnam veterans treated for posttraumatic stress disorder. Journal of Nervous and Mental Disease 179:558-562, 1991Crossref, Medline, Google Scholar
34. Frueh BC, Turner SM, Beidel DC, et al: Trauma management therapy: a preliminary evaluation of a multicomponent behavioral treatment for chronic combat-related PTSD. Behaviour Research and Therapy 34:533-543, 1996Crossref, Medline, Google Scholar
35. Pitman RK, Orr SP, Altman B, et al: Emotional processing and outcome of imaginal flooding therapy in Vietnam veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry 37:409-418, 1996Crossref, Medline, Google Scholar
36. Reist C, Kauffman CD, Haier RJ, et al: A controlled trial of desipramine in 18 men with posttraumatic stress disorder. American Journal of Psychiatry 146:513-516, 1989Link, Google Scholar
37. Marshall RP, Jorm AF, Grayson DA, et al: Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatric Services 49:1609-1611, 1998Link, Google Scholar
38. Rosenheck R, Dausey DJ, Frisman L, et al: Outcomes after initial receipt of Social Security benefits among homeless veterans with mental illness. Psychiatric Services 51:1549-1554, 2000Link, Google Scholar
39. Becker DR, Smith J, Tanzman B, et al: Fidelity of supported employment programs and employment outcomes. Psychiatric Services 52:834-836, 2001Link, Google Scholar
40. Bond G, Drake RE, Becker DR, et al: Effectiveness of psychiatric rehabilitation approaches for employment of people with severe mental illness. Journal of Disability Policy Studies 10:18-52, 1999Crossref, Google Scholar
41. Clark RE, Dain BJ, Xie H, et al: The economic benefits of supported employment for persons with mental illness. Journal of Mental Health Policy and Economics 1:63-71, 1998Crossref, Medline, Google Scholar
42. Rosenheck R, Stolar M, Fontana A: Outcomes monitoring and the testing of new psychiatric treatments: work therapy in the treatment of chronic post-traumatic stress disorder. Health Services Research 35:133-151, 2000Medline, Google Scholar
43. Drew D, Drebing CE, Van Ormer A, et al: Effects of disability compensation on participation in and outcomes of vocational rehabilitation. Psychiatric Services 52:1479-1484, 2001Link, Google Scholar
44. Goldman HH: The obligation of mental health services to the least well off. Psychiatric Services 50:659-663, 1999Link, Google Scholar
45. Rosenheck R, Armstrong M, Callahan D, et al: Obligation to the least well off in setting mental health priorities: a consensus statement. Psychiatric Services 49:1273-1274, 1290, 1998Link, Google Scholar
46. Sayer NA, Thuras P: The influence of patients' compensation-seeking status on the perceptions of Veterans Affairs clinicians. Psychiatric Services 53:210-212, 2002Link, Google Scholar



