Multiple Psychotropic Pharmacotherapy Among Child and Adolescent Enrollees in Connecticut Medicaid Managed Care
Abstract
OBJECTIVES: The authors sought to determine the prevalence, patterns, and demographic correlates of multiple psychotropic pharmacotherapy in a statewide sample of low-income children and adolescents in community-based clinical care. METHODS: The Medicaid managed care database of the Connecticut Department of Social Services was the source of linked encounter and pharmacy information for the one-year period ending June 30, 1999. Period prevalence was calculated for children and adolescents ranging in age from newborn through 18 years who had any psychotropic drug prescription claims during the study period. For each participant, multiple psychotropic pharmacotherapy was defined as having claims for prescriptions for medications in two or more different psychotropic drug classes during a seven-day period. Age, gender, race, and state custody status were examined across groups, and multiple psychotropic pharmacotherapy patterns were identified. RESULTS: Of the 196,505 youths in Medicaid managed care, 9,447 received at least one psychotropic medication, yielding a period prevalence of 4.8 percent. Among youths who received psychotropics, 13.6 percent had received multiple psychotropic pharmacotherapy. Multivariate logistic regression revealed that participants who received psychotropics, alone or in combination, were significantly more likely to be in state custody, male, and older than other participants and less likely to be African American or Hispanic. Stimulants, antidepressants, and mood stabilizers were the most commonly dispensed agents. The most common drug class combinations were an antidepressant plus an antipsychotic, a stimulant plus an antidepressant, and a stimulant plus an alpha2 agonist. CONCLUSIONS: Our findings revealed sociodemographic differences in psychopharmacological care among young Medicaid managed care enrollees and the common occurrence of multiple psychotropic pharmacotherapy.
The empirical foundations of pediatric psychopharmacology have rapidly expanded during the past two decades (1). Especially promising are a series of randomized controlled trials that documented the short-term efficacy among children and adolescents of psychotropic medications for disorders such as attention-deficit hyperactivity disorder (ADHD), obsessive-compulsive disorder, generalized anxiety disorder, and major depressive disorders (2).
Despite these advances, however, the field continues to have limited empirical data on the treatment of youths with complex and comorbid conditions. Further, current reimbursement mechanisms have put a premium on brief, symptom-targeted interventions such as pharmacotherapy, leading to treatment plans that do not necessarily follow available guidelines for the treatment of children and adolescents (3).
There is compelling pharmacoepidemiological evidence to document the increasing prevalence of psychotropic drug use among children, even those of preschool age (4). Moreover, the use of combined psychotropic drug treatment is on the rise. In a study of community mental health centers in Baltimore County, an increase in the use of multiple concurrent psychotropics was described for the period between 1988 and 1994: from 9 percent to 21 percent among outpatients taking medications and from 26 percent to 42 percent among inpatients (5). A recent study stated that 30 percent of children with ADHD co-occurring with another disorder received concurrent medications, compared with 10 percent of those with ADHD alone (6). A North Carolina Medicaid managed care study found that of 6,984 youths for whom a selective serotonin reuptake inhibitor (SSRI) was prescribed in 1998, 30.1 percent also received a stimulant during the same year (7). In a small case series, 50 of 83 children (60 percent) living in a residential treatment center received combination treatments (8).
Although there is limited empirical evidence to support its use, combined pharmacotherapy is becoming an increasingly accepted practice in pediatric psychopharmacology (9). In the hands of experienced clinicians, rational use of combined psychotropic medications may result in positive effects for the pediatric patient. For example, clinicians may resort to combination treatments in order to address a comorbid condition or to augment the benefits of one medication.
At the same time, combined psychopharmacotherapy can be an unjustified practice, as when duplicative agents (two or more agents in the same class) or offsetting agents (two or more medications with opposing actions) are initiated (10). Failure to prune ineffective medications during ongoing treatment is one of the common pathways from rational to irrational polypharmacy (11). Drug interactions are another important consideration during combined treatment. Problems can arise either from pharmacokinetic factors—such as effects mediated by the cytochrome P-450 system (12)—or from poorly understood pharmacodynamic mechanisms that may have additional developmentally sensitive implications—such as the purported toxicity associated with stimulant and alpha2 agonist combinations (13).
Combined therapy is thus fraught with potential pitfalls. These include the resort to stand-alone pharmacotherapy dislocated from a multifaceted treatment approach and the temptation to add a second medication in lieu of other modes of treatment, such as psychotherapy (14).
One of the primary aims of pharmacoepidemiology is to examine trends in clinical practice. Despite growing empirical support for psychopharmacological interventions for children with certain psychiatric disorders, a gap between research and practice remains, and clinicians are often constrained to making choices with incomplete evidence-based guidance. Indeed, randomized clinical trials are unlikely to investigate more than a small fraction of potential combination treatments. Moreover, the algorithms or consensus guidelines that have been published (15), although they provide some support for combination treatments, are neither an accurate reflection of current clinical practices nor a substitute for the level of empirical support provided by randomized clinical trials. A claims-based study describing community practice patterns can be an informative initial step toward understanding current combination psychotropic interventions and can guide future research efforts on this type of treatment.
The objective of this study was to determine the prevalence, patterns, and demographic correlates of psychotropic drug use in general, as well as of multiple psychotropic pharmacotherapy in particular, in a statewide sample of low-income children and adolescents receiving community-based clinical care.
Methods
Study design
This cross-sectional study used Connecticut Medicaid managed care administrative and pharmacy data. Institutional review board approval was obtained from the Yale University School of Medicine and the University of Connecticut School of Medicine. The ethical and confidentiality guidelines proposed for the analysis of large population-based data sets as specifically relevant to psychiatric research were followed throughout (16).
Sources of data and analytic approach
Linked encounter data and pharmacy claims data were derived from the Connecticut Medicaid managed care database, which is maintained by the Connecticut Department of Social Services through Qualidigm. The study population included all children and adolescents ranging in age from newborn through 18 years who were continuously enrolled in the Connecticut Medicaid managed care program between July 1, 1998, and June 30, 1999. Children with any claims for psychotropic drugs were identified from a comprehensive National Drug Code registry. Psychotropics were placed in one of six classes: stimulants, antipsychotics, antidepressants, mood stabilizers, alpha agonists, and anxiolytics. Antihistamines (including hydroxyzine), beta blockers, and anticholinergic agents were specifically excluded from the analysis, as were antiepileptic drugs dispensed for a seizure disorder as primary diagnosis. For the purposes of this study, patients with multiple psychotropic pharmacotherapy were defined as individual enrollees with prescription claims for medications from two or more different psychotropic drug classes during a seven-day interval following the index prescription. The seven-day sliding window was selected in an effort to maximize the capture of concurrent use of different psychotropics; it is consistent with published methods (17). Psychiatric diagnoses were based on ICD-9 codes appearing on the reimbursement claims (code range 290.00 to 319.99). Age, gender, race, and state custody status were examined across groups, and the most common patterns of multiple psychotropic pharmacotherapy were identified.
Statistical analyses
Data were summarized across sociodemographic characteristics for the dichotomous outcomes of two dimensions: presence or absence of psychotropic drug use for the entire study population and presence or absence of multiple psychotropic pharmacotherapy for study participants taking psychotropics. Separate logistic regression models were fitted to estimate the effects of the independent variables on each of the two outcomes. Results are presented as odds ratios (ORs) and 95 percent confidence intervals (CIs), both for the unadjusted (bivariate) and adjusted (multivariate) models. Backward elimination was used for all adjusted models. All analyses were conducted with SAS version 8.0. Unless otherwise specified, all results are significant at less than .001.
Results
Study population and period prevalence rates
The total study population consisted of 196,549 individuals enrolled in the Connecticut Medicaid managed care program for any length of time during the study period. As shown in Table 1, ethnic background and gender were evenly distributed across the study population, and age was skewed toward younger enrollees: more than 85 percent were 14 years or younger. A small fraction of children were in the custody of the Connecticut Department of Children and Families.
At least one psychotropic medication was dispensed to a total of 9,447 participating youths during the study period, yielding a period prevalence of 4.8 percent. Among these youths, 1,286 (13.6 percent) fit the definition of multiple psychotropic pharmacotherapy, yielding a period prevalence of .7 percent. Stimulants were the most commonly dispensed psychotropic class, accounting for almost half the total prescriptions. The rank order for other drug classes as well as the more commonly found multiple psychotropic pharmacotherapy patterns are presented in Table 2.
Diagnoses
Information on primary diagnosis was available for 5,397 (57.1 percent) of the participants taking psychotropics. The three most common diagnoses associated with psychotropic use were disruptive disorders, including ADHD and conduct disorder (57.9 percent of participants with diagnoses available); affective disorders, including unipolar and bipolar depression (17.2 percent of participants); and anxiety disorders, including generalized anxiety disorder and obsessive-compulsive disorder (17.2 percent of participants) (4). Other disorders—developmental, psychotic, personality, eating, or substance abuse—were each present in fewer than 5 percent of participants.
Demographic predictors
As shown in Table 3, univariate analyses revealed that children taking psychotropic medications were significantly more likely to be in state custody, male, white, and older than peers who were not taking psychotropics (10.5±3.8 years compared with 7.7±5.3 years). These four characteristics also significantly differentiated youths receiving multiple psychotropic pharmacotherapy from their peers who were not taking psychotropics (11.5±3.5 years compared with 10.4±3.8 years). Odds ratios derived from adjusted logistic regression models are included in Table 3.
Discussion and conclusions
This study documented a 4.8 percent period prevalence of psychotropic drug use among children enrolled in Connecticut Medicaid managed care. This rate is virtually identical to that reported in 1995 for children enrolled in Kansas Medicaid, the most recent study for which comparable data are available (18). Consistent with earlier reports, our findings reveal differences in age, gender, and ethnicity among youths who received psychotropic medications. Age differences are of a particularly timely relevance, because psychotropic medication rates among preschool children have recently attracted widespread attention in both the scientific and the lay press. Findings from our study corroborate the frequent use of psychotropics in this age group. For example, among 35,274 children aged two to four years, stimulants were prescribed for 396, yielding an age-specific period prevalence of 11.2 per 1,000. This rate is in keeping with preschooler rates recently reported in two studies. In a study by Zito and colleagues (4), the prevalence of stimulant use in 1995 ranged from 5.1 to 12.3 per 1,000, and in a study of 1998 North Carolina Medicaid data the prevalence was 13 per 1,000 for children ages 1 to 5 (7). Even if not strictly comparable, all three studies point to a prevalence in the range of .5 to 1.3 percent in this very young age group—one for which the empirical database is especially limited.
Overall, boys were 2.4 times as likely to receive psychotropics as were girls, and children aged ten to 14 years were at least 1.4 times as likely as those in any other age group. This distribution pattern, together with stimulants' being the most commonly prescribed psychotropic class (Table 2), suggests that ADHD is the main condition targeted pharmacologically. Our diagnostic information, although limited, corroborates this impression: almost 60 percent of youths for whom data were available had a primary diagnosis of ADHD. Moreover, the second and third most common patterns of multiple psychotropic pharmacotherapy were stimulant plus antidepressant and stimulant plus alpha agonist—combinations suggested in a recently published algorithm for ADHD when stimulants alone are not effective (15,19).
Consistent with previous studies (7,20,21), our data reveal that children from minority groups are less likely to have psychotropics prescribed for them. For example, when the analysis was adjusted for potential confounders, white youths were 2.4 times and 1.7 times as likely to have psychotropics prescribed as were their black or Hispanic peers, respectively. This consistently documented racial and ethnic disparity may reflect differences in access to care or different attitudes or cultural beliefs among various groups—about mental health in general or about the use of psychotropics in particular. In addition, racial and ethnic misclassification is a small possibility to consider in the analysis of large databases. Regardless of the underlying reason for these differences, additional study is clearly warranted to understand and address such disparities in psychotropic drug use.
Children in state custody represented only 4.7 percent of the Medicaid population yet accounted for 17.8 percent of the psychotropic prescriptions filled. This 4.5-fold higher rate emerged as the single strongest predictor of psychotropic drug use in our study. Given that children in state custody are a vulnerable group at high risk of serious psychopathology, this is not an entirely surprising finding. To our knowledge, rates of psychotropic drug use for children in state custody have not been previously studied. However, two studies of children in the Los Angeles County foster care system (representing a segment of children in state custody) have documented a threefold higher rate of psychotropic drug use than in the control group of youths in the community (22,23), and a third study has found similar patterns among foster care youths covered by a mid-Atlantic state Medicaid program (24).
As defined here, multiple psychotropic pharmacotherapy is a common practice in pediatric pharmacotherapy; 13.6 percent of youths for whom psychotropics are prescribed receive more than one psychotropic. Given the cross-sectional nature of our study, it was not possible to determine with certainty whether agents were used concurrently (as an additive strategy) or sequentially (for example, as part of a cross-tapering switch). To minimize this potential misclassification, we restricted combination use to medications from different drug classes, because medications in the same class would be more suggestive of a switching pattern. Only a longitudinal approach can distinguish such underlying prescription patterns; however, our findings suggest that treatment with more than a single psychotropic agent during this conservatively defined time interval are common in this Medicaid population, possibly as part of a change to more stable medication regimens. In addition to revealing multiple psychotropic pharmacotherapy as a common treatment pattern, our study found significant sociodemographic factors associated with its occurrence. Children who were ten years of age and older, male, white, or in state custody were all more likely to receive multiple psychotropic pharmacotherapy. These characteristics also predict psychotropic drug use in general, although they warrant particular attention as predictors of multiple pharmacotherapy. In the one previous study that assessed predictors of polypharmacy among adults, neither age, sex, nor race was a significant factor (10).
Our study has several limitations. First, claims-based data provide minimal clinical information, and that information is of uncertain quality; there is no readily available way of validating assigned diagnoses. Moreover, a primary diagnosis was missing for 42.9 percent of children treated with psychotropics during the study period. Although this is a substantial proportion of participants, it is not an uncommon one in comparable pharmacoepidemiology surveys. For example, a recent outpatient study found that no psychiatric diagnosis was made in more than 30 percent of visits involving a psychotropic medication (25). The investigators suggested that such a deficiency might be related to either of two factors: primary care physicians' limited knowledge about, or comfort with, assigning psychiatric diagnoses; or clinicians' resorting to pharmacological intervention when addressing vague behavioral problems for which there is no clear diagnosis.
A second limitation is that our choice of a one-week interval to estimate multiple psychotropic pharmacotherapy is potentially problematic. In the absence of a standardized time interval for the assessment of polypharmacy, some investigators (7,26) have chosen a one-year window. However, such a choice, while increasing the sensitivity of our findings, would have done so at the expense of an unacceptable number of false positives—that is, cases of sequential rather than concurrent use of different medications. Indeed, when we used a three-month window, our estimate of multiple psychotropic pharmacotherapy more than tripled, to 42 percent. Our ultimate choice for the briefer window of time is consistent with the published experience of another group (17) and protects from overestimation of multiple psychotropic pharmacotherapy (false positives). Clearly, the best way to estimate the prevalence and specific patterns of multiple psychotropic pharmacotherapy, and to differentiate concurrent from stepwise or sequential drug use, would be to track participants longitudinally. Other informative next steps toward this end might be targeted chart reviews and surveys of the decision-making processes of community practitioners. Despite the uncertainty of our one-week window, our study does provide initial insights into an increasingly common practice within the field of pediatric psychopharmacology.
A third limitation is that the Connecticut Medicaid managed care database did not include information on prescribers' professional affiliation, such as physicians, physician assistants, or clinical nurse specialists, or their specialty training, such as primary care medicine, pediatrics, or psychiatry. Previous studies have documented that in the treatment of ADHD, for example, the majority of psychotropic medications are prescribed not by mental health specialists but rather by general practitioners (27,28). Another consideration is that the more complicated or treatment-refractory cases may in turn be referred to specialists, who may follow different prescription patterns, including combination treatments (29). In a previous study of adults, physician specialty (psychiatry versus nonpsychiatry) was found to be the single strongest positive predictor of polypharmacy (10). Two subsequent studies have also found physician specialty to be significantly related to psychotropic combination prescription patterns for youths (26,30). Such findings have direct training and administrative implications, supporting the need for more extensive training in psychopharmacology for pediatricians and other primary care practitioners, the procurement of appropriate staffing, and the facilitation of more efficient referral pathways to specialists.
Despite its limitations, our study documented rates and patterns of psychotropic drug use among young Connecticut Medicaid managed care enrollees that are comparable to rates in other parts of the country. In particular, our study replicated findings of both clear differences among racial groups in this modality of treatment and the use of psychotropic drugs among as many as 1 percent of preschoolers. Moreover, our study showed that a considerable proportion of children receiving psychotropics have been treated with two or more such agents within a one-week period. Future claims-based research in pediatric psychopharmacology will permit the study of changes over time in this modality of treatment, as well as the characterization of the extent and patterns of multiple psychotropic pharmacotherapy in community-based clinical settings.
Acknowledgments
This work was supported by the Connecticut Department of Social Services, contract #083 PSA MED 997 to Qualidigm; by Scientist Career Development Award K01 MH01792 to Dr. Martin; by Public Health Service grants M01 RR06022, 5P01 HD1DC35482, and 5P01 HD03008; and by National Institute of Mental Health research unit on pediatric psychopharmacology contract MH97 CR0001 to Yale University. The authors are grateful to James Linnane, Judith Meyers, Ph.D., and Mark Schaefer, Ph.D., whose efforts made this collaborative project possible.
Dr. Martin, Dr. Stubbe, and Dr. Scahill are affiliated with the Child Study Center at Yale University School of Medicine, 230 South Frontage Road, New Haven, Connecticut 06520-7900 (e-mail, [email protected]). Dr. Van Hoof and Ms. Sherwin are affiliated with Qualidigm in Middletown, Connecticut. Dr. Van Hoof is also affiliated with the University of Connecticut School of Medicine in Farmington. Earlier versions of this work were presented as posters at the annual meeting of the Drug Information Association held July 7-11, 2001, in Denver and at the annual meeting of the American Academy of Child and Adolescent Psychiatry held October 22-28, 2001, in Honolulu.
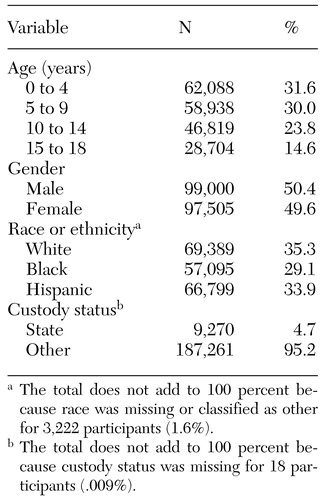 |
Table 1. Demographic characteristics of 196,549 children enrolled in the Connecticut Medicaid managed care program between July 1, 1998, and June 30, 1999
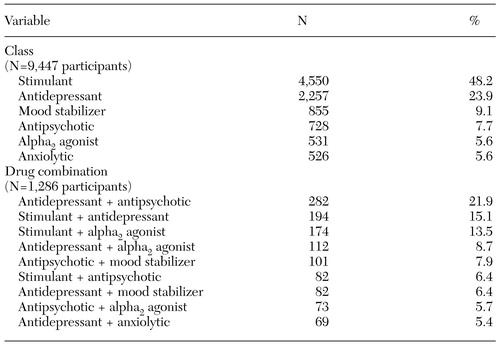 |
Table 2. Distribution of drug classes and of multiple psychotropic pharmacotherapy prescribed for more than 5 percent of study participants
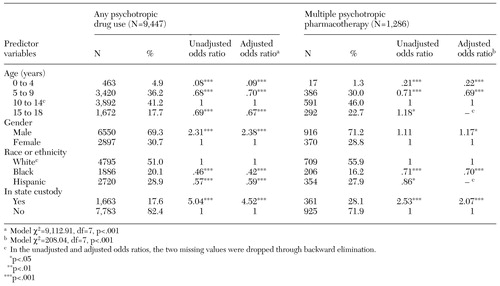 |
Table 3. Logistic regression models of association between demographic variables and psychotropic drug use or multiple psychotropic pharmacotherapy
1. Martin A, Scahill L: Psychopharmacology: Preface (to issue). Child and Adolescent Psychiatric Clinics of North America 9(1): xv-xix, 2000Google Scholar
2. Riddle MA, Kastelic EA, Frosch E: Pediatric psychopharmacology. Journal of Child Psychology and Psychiatry 42(1):73-90, 2001Google Scholar
3. Jellinek MS: Overzealous prescribing of medications (editorial). Journal of the American Academy of Child and Adolescent Psychiatry 37:900-901, 1998Crossref, Medline, Google Scholar
4. Zito JM, Safer DJ, dosReis S, et al: Trends in the prescribing of psychotropic medications to preschoolers. JAMA 283:1025-1030, 2000Crossref, Medline, Google Scholar
5. Safer DJ: Changing patterns of psychotropic medications prescribed by child psychiatrists in the 1990s. Journal of Child and Adolescent Psychopharmacology 7:267-274, 1997Crossref, Medline, Google Scholar
6. Boles M, Lynch FL, DeBar LL: Variations in pharmacotherapy for attention deficit hyperactivity disorder in managed care. Journal of Child and Adolescent Psychopharmacology 11:43-52, 2001Crossref, Medline, Google Scholar
7. Rushton JL, Whitmire JT: Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends:1992 to 1998. Archives of Pediatric and Adolescent Medicine 155:560-565, 2001Google Scholar
8. Connor DF, Ozbayrak KR, Kusiak KA, et al: Combined pharmacotherapy in children and adolescents in a residential treatment center. Journal of the American Academy of Child and Adolescent Psychiatry 36:248-254, 1997Crossref, Medline, Google Scholar
9. Wilens TE, Spencer T, Biederman J, et al: Combined pharmacotherapy: an emerging trend in pediatric psychopharmacology. Journal of the American Academy of Child and Adolescent Psychiatry 34:110-112, 1995Crossref, Medline, Google Scholar
10. Nichol MB, Stimmel GL, Lange SC: Factors predicting the use of multiple psychotropic medications. Journal of Clinical Psychiatry 56:60-66, 1995Medline, Google Scholar
11. Kingsbury SJ, Yi D, Simpson GM: Psychopharmacology: rational and irrational polypharmacy. Psychiatric Services 52:1033-1036, 2001Link, Google Scholar
12. Oesterheld JR, Flockhart DA: Cytochrome P450 mediated drug interactions. Child and Adolescent Psychiatric Clinics of North America 9:43-76, 2000Crossref, Medline, Google Scholar
13. Wilens TE, Spencer TJ, Swanson JM, et al: Combining methylphenidate and clonidine: a clinically sound medication option. Journal of the American Academy of Child and Adolescent Psychiatry 38:614-619; discussion 619-622, 1999Crossref, Medline, Google Scholar
14. Woolston JL: Combined pharmacotherapy: pitfalls of treatment. Journal of the American Academy of Child and Adolescent Psychiatry 38(11):1455-1457, 1999Google Scholar
15. Pliszka SR, Greenhill LL, Crismon ML, et al: The Texas Children's Medication Algorithm Project: report of the Texas consensus conference panel on medication treatment of childhood attention-deficit/hyperactivity disorder: Part 1. attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry 39:908-919, 2000Crossref, Medline, Google Scholar
16. Simon GE, Unutzer J, Young BE, et al: Large medical databases, population-based research, and patient confidentiality. American Journal of Psychiatry 157:1731-1737, 2000Link, Google Scholar
17. Leslie DL, Rosenheck RA: Use of pharmacy data to assess quality of pharmacotherapy for schizophrenia in a national health care system: individual and facility predictors. Medical Care 39:923-933, 2001Crossref, Medline, Google Scholar
18. Fox MH, Foster CH, Zito JM: Building pharmacoepidemiological capacity to monitor psychotropic drug use among children enrolled in Medicaid. American Journal of Medical Quality 15:126-136, 2000Crossref, Medline, Google Scholar
19. Pliszka SR, Greenhill LL, Crismon ML, et al: The Texas Children's Medication Algorithm Project: Report of the Texas consensus conference panel on medication treatment of childhood attention-deficit/hyperactivity disorder: Part 2. tactics: attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry 39:920-927, 2000Crossref, Medline, Google Scholar
20. Zito JM, Safer DJ, dosReis S, et al: Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. Journal of the American Academy of Child and Adolescent Psychiatry 37:179-184, 1998Crossref, Medline, Google Scholar
21. Zito JM, Safer DJ, dosReis S, et al: Methylphenidate patterns among Medicaid youths. Psychopharmacology Bulletin 33:143-147, 1997Medline, Google Scholar
22. Zima BT, Bussing R, Crecelius GM, et al: Psychotropic medication use among children in foster care: relationship to severe psychiatric disorders. American Journal of Public Health 89:1732-1735, 1999Crossref, Medline, Google Scholar
23. Zima BT, Bussing R, Crecelius GM, et al: Psychotropic medication treatment patterns among school-aged children in foster care. Journal of Child and Adolescent Psychopharmacology 9:135-147, 1999Crossref, Medline, Google Scholar
24. DosReis S, Zito JM, Safer DJ, et al: Mental health services for youths in foster care and disabled youths. American Journal of Public Health 91:1094-1099, 2001Crossref, Medline, Google Scholar
25. Goodwin R, Gould MS, Blanco C, et al: Prescription of psychotropic medications to youths in office-based practice. Psychiatric Services 52:1081-1087, 2001Link, Google Scholar
26. Zito JM, Safer DJ, dosReis S, et al: Psychotherapeutic medication patterns for youths with attention-deficit\hyperactivity disorder. Archives of Pediatric and Adolescent Medicine 153:1257-1263, 1999Crossref, Medline, Google Scholar
27. Zarin DA, Tanielian TL, Suarez AP, et al: Treatment of attention-deficit hyperactivity disorder by different physician specialties. Psychiatric Services 49:171, 1998Link, Google Scholar
28. Wolraich ML, Lindgren S, Stromquist A, et al: Stimulant medication use by primary care physicians in the treatment of attention deficit hyperactivity disorder. Pediatrics 86:95-101, 1990Medline, Google Scholar
29. Zarin DA, Suarez AP, Pincus HA, et al: Clinical and treatment characteristics of children with attention-deficit/hyperactivity disorder in psychiatric practice. Journal of the American Academy of Child and Adolescent Psychiatry 37:1262-1270, 1998Crossref, Medline, Google Scholar
30. Bussing R, Zima BT, Belin TR: Variations in ADHD treatment among special education students. Journal of the American Academy of Child and Adolescent Psychiatry 37:968-976, 1998Crossref, Medline, Google Scholar



