Datapoints: Treatment of Attention-Deficit Hyperactivity Disorder by Different Physician Specialties
In recent years, increased national attention has been drawn to the diagnosis and treatment of attention-deficit hyperactivity disorder (ADHD). Much of the attention has focused on the large variation in practice patterns found in community studies, with the assumption that most children with ADHD are treated by primary care providers (1). It is not known what proportion of children treated for ADHD are cared for by psychiatrists or to what extent quality-of-care concerns raised by these community studies apply to the care provided by psychiatrists.
This column examines office visits for ADHD by patients age 14 or younger across physician specialties, including psychiatry. It uses weighted data from the 1995 National Ambulatory Medical Care Survey (NAMCS). ADHD-related office visits were identified by one of the following criteria: the International Classification of Diseases (ICD) code for ADHD listed in one of the diagnosis fields; at least one psychostimulant prescribed, supplied, administered, or continued during the visit; or a marked checkbox indicating an ADHD diagnosis.
A total of 3,423,089 ADHD-related visits were identified in 1995, representing 3.2 percent of all physician visits by patients age 14 or younger. Comparison with 1985 NAMCS data showed a fivefold increase in the number of ADHD-related visits between the two surveys. This increase may be partly attributed to the ADHD checkbox item, which was not included in the 1985 survey. However, disregarding this criterion, ADHD-related visits tripled between 1985 and 1995 (2). A psychostimulant was reported in 49 percent of the visits in 1995.
Figure 1 shows the distribution of the ADHD-related visits in 1995 for three physician specialties: primary care (general and family practice, adolescent medicine, pediatrics, geriatric medicine and internal medicine); psychiatry (child and adolescent psychiatry, psychiatry, and psychoanalysis); and other medical specialties, including neurology and child neurology. Visits to psychiatrists accounted for 12.4 percent of all ADHD-related visits, indicating that psychiatrists treat a substantial proportion of the childhood ADHD population. Some evidence suggests that the patients treated by psychiatrists constitute a more complex and more severely ill segment of the ADHD population (3). Therefore, it will be important to characterize the differences in patients seen by psychiatrists and primary care physicians as well as in the treatments they provide. In particular, efforts to improve the quality of care for children and adolescents with ADHD will need to take into account important differences in case mix and practice patterns.
Acknowledgments
The authors thank Julie Magno Zito, Ph.D., Harold Alan Pincus, M.D., Mark Olfson, M.D., M.P.H., and James Thompson, M.D., for their contributions to the analyses on which this report is based. This work was supported in part by a grant from the van Ameringen Foundation.
Dr. Zarin, Ms. Tanielian, and Ms. Suarez are associated with the office of research of the American Psychiatric Association, 1400 K Street, N.W., Washington, D.C. 20005. Mr. Marcus is with the Stanley Center at Western Psychiatric Institute and Clinic in Pittsburgh. Ms. Tanielian and Harold Alan Pincus, M.D., are coeditors of this column.
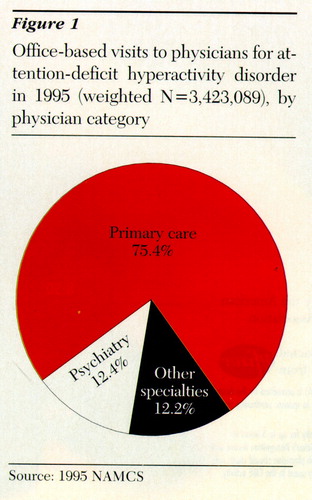
Figure 1. Office-based visits to physicians for attention-deficit hyperactivity disorder in 1995 (weighted N=3,423,089), by physician category
1. Wolraich ML, Lindgren S, Stromquist A: Stimulant medication use by primary care physicians in the treatment of attention-deficit hyperactivity disorder. Pediatrics 86:95-101, 1990Medline, Google Scholar
2. Pincus HA, Tanielian TL, Marcus SC, et al: Prescribing trends in psychotropic medication: primary care, psychiatry, and other medical specialties. JAMA, in pressGoogle Scholar
3. Epstein MA, Shaywitz SE, Shaywitz BA, et al: The boundaries of attention deficit disorder. Journal of Learning Disabilities 24:78-86, 1991Crossref, Medline, Google Scholar



