The New York-New York Housing Initiative and Use of Public Shelters by Persons With Severe Mental Illness
Abstract
OBJECTIVE: The study examined changes in the use of shelters in New York City by mentally ill persons with a history of homelessness who received housing placements through the New York-New York (NY/NY) housing initiative between 1990 and 1999 and the impact of the initiative on the overall demand for shelter beds in the city. METHODS: Computerized service records on housing, shelter use, and health care services were linked to create an integrated data set for 3,167 persons who received NY/NY housing placements, which provided mental health services, and for a matched control group of persons with mental illness who used shelters but did not receive housing placements. Regression analyses were used to assess the relationships between shelter use and receipt of a placement. Differences in postplacement shelter use between NY/NY housing recipients and the matched control group were then examined at an individual level and a population level. RESULTS: Heavy users of the shelter system were more likely to be placed in NY/NY housing. In the two-year postplacement period, persons who received a NY/NY housing placement used, on average, 128.2 fewer shelter days than those in the control group. In 1996, the NY/NY housing initiative reduced the average nightly census in New York City shelters by an estimated 4.6 percent. CONCLUSIONS: Providing housing combined with mental health services is an effective approach to reducing shelter use among mentally ill persons who have a history of homelessness.
Research suggests that only a minority of the homeless population can be called chronically homeless. This group, which typically experiences few but extended spells of homelessness, represents less than 15 percent of all homeless persons and collectively uses more than half of all shelter beds. This group of chronically homeless persons has significantly higher rates of mental illness than the rest of the sheltered homeless population (1,2).
A number of studies have suggested that housing combined with mental health services may be an effective intervention for this group. Although community-based housing for persons with mental illness comprises several distinct approaches to configuring housing and services (3,4), it commonly features housing with rent that is based on the tenant's income, combined with social and clinical services that are available either on site or on a mobile, as-needed basis. Provision of both housing and mental health services has resulted in a lower incidence of subsequent episodes of homelessness than provision of standard mental health services without housing (5,6,7) and of housing without mental health services (8,9). Thus moving chronically homeless persons from shelters to permanent housing is not only appropriate and humane but also promises to greatly reduce demand for homeless services by targeting a relatively small group of the heaviest service users that is considered to be among the most difficult homeless populations to serve (10).
In 1990, New York State and New York City, through the jointly funded New York-New York (NY/NY) agreement, initiated one of the largest community-based mental health housing initiatives to date. NY/NY made resources available to create 3,300 housing units and social services support for persons who had been homeless and who had a psychiatric diagnosis (11,12). After the inception, a marked decline was noted in demand for single adult shelter beds in New York City. However, it is uncertain how much of this decline can be attributed to NY/NY housing.
This study determined whether NY/NY targeted chronic shelter users for housing placement and assessed the subsequent impact of these placements on levels of shelter use—both individually among NY/NY users and aggregately with respect to the overall shelter census—between 1989 and 1999. The results make it possible to evaluate the potential for realizing disproportionate reductions in shelter demand by targeting chronic users (13,14).
Methods
Data
Data were drawn from an integrated database of shelter users in New York City created by linking records from automated management information systems maintained by public service providers (15). The principal data sets used for the study are maintained by the New York City Department of Homeless Services (DHS) and the New York City Human Resources Administration (HRA). DHS has been tracking shelter use since 1986 for its single adult shelter network. This database contains information on dates and duration of individual shelter stays and on a limited set of characteristics and circumstances for individual shelter users. HRA maintains records for each person placed in housing through NY/NY. The database includes demographic characteristics and the date and type of housing placement. No information on the duration of the NY/NY placement was available for this study. Psychiatric diagnoses, including substance abuse status, were obtained from linked data sets containing information about the receipt of inpatient and outpatient services from New York State Medicaid, the New York City Health and Hospitals Corporation, the New York State Office of Mental Health, and the U.S. Department of Veterans Affairs. Records were merged across the six data sets on the basis of four matching identifiers: Social Security number, first name, last name, and date of birth. Further details on this process are available from the authors.
All persons placed in NY/NY housing are considered mentally ill; mental illness among shelter users is determined on the basis of diagnoses associated with one inpatient stay or two outpatient visits (16) in the four health care systems or through a DHS intake assessment. Diagnoses considered to reflect mental illness include ICD-9 codes 290, 293-299, 300-302, and 306-319.
We identified all shelter users who had a record of a mental illness diagnosis or assessment. Next, we created a data set for shelter users with a NY/NY placement and shelter users who had a psychiatric diagnosis but no record of receiving a placement. A group of matched controls were selected from the latter group with the use of propensity score matching procedures (17,18). We used propensity score matching to reduce multiple matching factors to a single composite score on the basis of the probability of assignment to the treatment group, conditional on demographic characteristics (age, race, and sex), diagnosis (schizophrenia, affective disorder, and drug or alcohol dependence), and preintervention shelter use (number of bed-days used and the duration between the last use of a shelter and the time of intervention) during the year before the intervention. For each case-control pair, the NY/NY placement date represents the point of intervention.
Analysis
We began by assessing differences in demographic and clinical characteristics and shelter use patterns of persons placed in NY/NY housing and mentally ill shelter users who were not placed. Bivariate distributions and the results of chi square tests were used to examine the differences between persons selected for NY/NY housing and other shelter users. A multivariate logistic regression model was then used to estimate the adjusted odds ratios (with confidence intervals) for the likelihood of shelter users being selected to receive a NY/NY placement. We hypothesized that persons selected for placement would be more likely to exhibit patterns of homelessness that were consistent with chronic use patterns—that is, more shelter days consumed over fewer discrete shelter stays.
We then compared postplacement shelter use between the NY/NY intervention group and matched controls. The effect of placement on the number of postintervention shelter days used was estimated with the use of a multivariate least-squares regression and generalized estimating equations to accommodate nonindependent observations such as matched pairs. The regression model controlled for various demographic and clinical characteristics and the use of shelters before the intervention.
Finally, we used the between-group difference in postintervention shelter days to estimate the impact of NY/NY on the shelter system's annual average daily census (ADC). The ADC is calculated by dividing the total number of shelter beds used during the year by the total number of days in that year. The actual ADC was compared with a projected ADC in which the postintervention shelter stays for each member of the study group were replaced by postintervention shelter stays of the corresponding matched control. The difference between the two calculations of the ADC equals the estimated change in shelter use attributable to NY/NY housing. We hypothesized that NY/NY housing would be associated with reduced postintervention shelter days and reductions in the ADC for single adult shelters.
Results
As shown in Table 1, shelter users who received placements differed from other mentally ill shelter users in demographic characteristics and, to a lesser extent, in clinical characteristics. The NY/NY group was older, and participants were more likely to be black and male and to have veteran status. The group was also more likely to have a diagnosis of drug or alcohol dependence, schizophrenia, and affective disorder. The NY/NY group was also more likely to have used more shelter days.
Adjusted odds ratios indicated that being 55 years old or older, being male, and having a diagnosis of alcohol or drug dependence each was associated with significantly lower odds of receiving a NY/NY placement. Conversely, being in the 40- to 54-year age group, being black, having a diagnosis of schizophrenia or affective disorder, and being a veteran were each associated with higher odds of receiving a placement. Persons whose first shelter episode occurred in earlier years were more likely to receive a placement, as were those who used more shelter days and fewer shelter stays. These findings support the hypothesis that chronic shelter use (a large number of days and few stays) increased the odds of receiving a placement.
The process of matching NY/NY participants to mentally ill shelter users in the control group was successful (data not shown). No significant differences in demographic characteristics were found between cases and controls of the matched-pair groups. Although significant differences in the prevalence of some clinical diagnoses were found between the two groups, the absolute difference was no more than 3 percent for any diagnosis: schizophrenia, 52.5 for the NY/NY group and 55.3 percent for the control group; personality or neurotic disorder, 29.4 and 31.9 percent; and co-occurring severe mental illness and chemical dependency, 35.4 and 37.7 percent.
A paired t test showed no significant difference between the two groups in the mean number of shelter days used during the year before the intervention (132.4 for the study group and 131.6 days for the control group). However, statistically significant differences were noted between groups in the duration of the gap between the last use of a shelter and the intervention date, suggesting that, on average, persons who received NY/NY placements had used a shelter more recently than their counterparts.
Even though the matching process was specifically designed to match all persons selected for placement who were in a shelter at the time of the intervention with persons who were also in a shelter at that time, a slight but statistically significant difference was found in the proportion of persons who were in a shelter when the intervention began—44.3 in the study group compared with 40.7 percent in the control group. Some study group members were matched with persons who were not in a shelter at the time of the intervention because of the limited number of controls available. Being in a shelter at the time of the intervention can be presumed to come with a substantially higher risk of postintervention shelter use, especially for persons in the control group, whose living situation was not affected by the intervention. Thus our analysis may have underestimated the reduction in shelter use associated with housing placement.
In the two years after the intervention, persons who received a NY/NY placement were less likely to use shelters—35.6 compared with 72.3 percent. In addition, they used substantially fewer shelter days—28.1 compared with 153.1. Even after the analysis adjusted for the demographic and clinical variables in Table 1, persons who received a placement used 128.2 fewer shelter days in the two years after placement (95 percent confidence interval, 120.6 to 135.9, p<.001).
As shown in Figure 1, until shortly before the intervention point, both groups used a steadily increasing number of shelter days per month. After the intervention, the number of days used by the study group declined dramatically and then held steady at a much lower rate, whereas use for the control group declined much more gradually. At the end of the postintervention period, the rates of use were at the lowest points for both groups, but the rate for the control group was more than three times higher.
Figure 2 shows the impact of NY/NY housing based on differences in the projected average daily census if such placements were not available. The percentage difference increased steadily to 4.6 percent in 1996 and then started to decline in 1998, when no more new placements occurred. Even though the impact of NY/NY on the ADC is evident, the census would have declined markedly in the absence of NY/NY.
Discussion
NY/NY housing placements were associated with substantial decreases in subsequent shelter use in a group of persons with severe mental illness and a history of heavy shelter use. The findings support the effectiveness of NY/NY housing placement when combined with services for a group that is considered to be among the most difficult homeless populations to serve. The results showed that persons with NY/NY placements and a history of using shelters used, on average, 132.4 shelter days in the year before placement and only 28.1 shelter days in the two years after placement.
These substantial reductions in shelter use on an individual level also led to measurable reductions in aggregate demand on the New York City shelter system. NY/NY housing is estimated to have accounted for a decrease of 4.6 percent in the demand for shelter during 1996 and for an overall 2.4 percent decrease between 1989 and 1999. However, the relative magnitude of the impact is difficult to gauge. On one hand, the ability of a 3,300-bed initiative to make such an impact on a system that in 1995 provided accommodations for 24,153 persons is noteworthy and highlights the returns that can be realized by targeting housing toward persons with patterns of chronic homelessness. On the other hand, although the NY/NY program clearly contributed to the general decline in shelter use by single adults in the 1990s, the start of the decline preceded any substantial impact NY/NY housing had on the system—and even without NY/NY housing, the census would have dropped markedly.
The NY/NY initiative was not only implemented on a scale large enough to have a measurable impact on New York City's shelter system but it also set a standard of quality for the provision of housing and mental health services in the community (11). Specifically, the level of funding for NY/NY housing, its the administrative structure, and the provision of services in conjunction with housing serve as safeguards against the provision of substandard housing and care that have recently come to light among numerous adult homes in New York City that are not affiliated with the NY/NY program (19). Furthermore, the availability of NY/NY housing coincided with substantial reductions in placements of homeless mentally ill persons into adult homes in the city (personal communications, Tempel C, New York Field Office for the Corporation for Supportive Housing, 2002; Lasicki T, Association for Community Living of New York State, 2002; and Nortz S, Coalition for the Homeless, 2002).
Reductions in shelter use over time and changes in patterns of homelessness over the life span are poorly understood, especially among heavy users of shelters. Our analysis controlled for one possible exit from the shelter system—placement in supported housing programs not affiliated with the NY/NY program. However, the relationship of other factors, such as intercity migration, mortality, incarceration, and institutionalization, to reductions in shelter use over time warrant further research.
The direct impact of the NY/NY housing initiative on the shelter system diminished over time for two reasons. First, even chronic shelter users seem to exit the system eventually without any apparent intervention or at least reduce their reliance on shelters. Thus the longer a person is housed through an intervention such as NY/NY housing, the less that person's tenancy can be associated with a reduction in shelter use. Second, even with the addition of NY/NY housing, one of the largest mental health housing initiatives to date, the need for such housing in New York City and elsewhere far exceeds the available supply (20). Without additions to the supply, new shelter users will occupy the beds once used by tenants of housing provided by the NY/NY program and other similar programs.
Of course, not all homeless people use shelters, and those who do may also sleep outdoors or may be considered homeless when they are in other settings, such as hospitals and jails. When use of shelters is a de facto proxy measure for homelessness, it is assumed that reductions in shelter use reflect overall reductions in homelessness. However, one limitation of this study was that it was not able to measure homelessness in nonshelter contexts.
A second limitation was the differences between persons with NY/NY placements and persons in the matched control group. Even though 26,612 mentally ill shelter users were potential control group members—eight times the number in the study group—attempts to match study group members and controls on many factors—demographic and clinical characteristics and patterns of shelter use—inevitably led to some differences. The most problematic of these differences involved shelter use before the intervention point; although the numbers of days used were similar, differences in use patterns were found. However, the strong effects associated with NY/NY housing persisted even after the analysis controlled for differences in preintervention shelter use, other matching factors, and various nonmatching factors.
Conclusions
The results reported here support the effectiveness of targeting housing and services toward chronically homeless mentally ill persons. Differences in shelter use associated with NY/NY housing placements were found at the individual level and in the overall demand for shelter beds. Although the placements provided by the NY/NY initiative were limited and the program was focused on a specific subgroup of the homeless population, the program represents an important facet of more comprehensive approaches to ending homelessness.
Acknowledgments
Funding for this research was provided by the Corporation for Supportive Housing and the Fannie Mae Foundation. The authors thank Paul Allison, Ph.D., for helpful comments.
Dr. Metraux is a postdoctoral fellow at the Center for Studies of Addiction, Dr. Marcus is research associate, and Dr. Culhane is associate professor at the Center for Mental Health Policy and Services Research at the University of Pennsylvania, 3535 Market Street No. 4095, Philadelphia, Pennsylvania 19104 (e-mail, [email protected]).
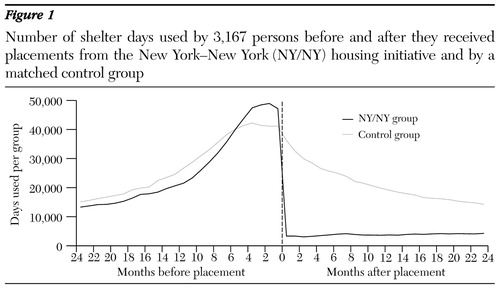
Figure 1. Number of shelter days used by 3,167 persons before and after they received placements from the New York-New York (NY/NY) housing initiative and by a matched control group
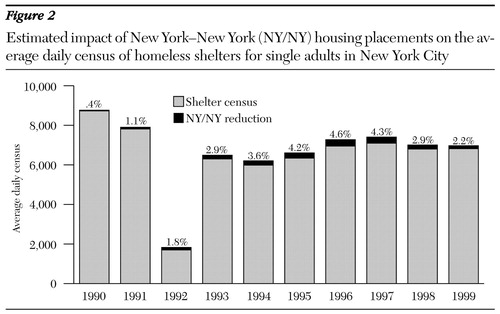
Figure 2. Estimated impact of New York-New York (NY/NY) housing placements on the average daily census of homeless shelters for single adults in New York City
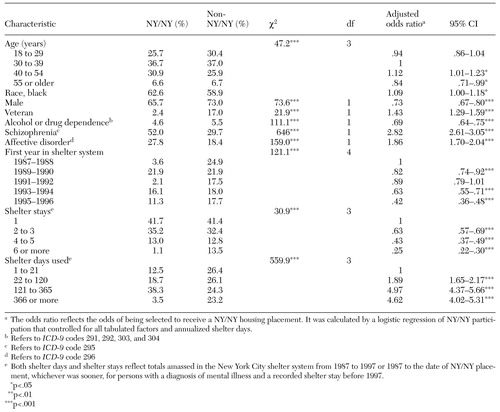 |
Table 1. Characteristics of persons with severe mental illness who used New York City shelters between 1988 and 1997 and who did or did not receive a housing placement under the New York-New York (NY/NY) housing initiative
1. Kuhn R, Culhane DP: Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results from the analysis of administrative data. American Journal of Community Psychology 26:207-232, 1998Crossref, Medline, Google Scholar
2. Burt MR, Aron LY, Lee E, et al: Helping America's Homeless: Emergency Shelter or Affordable Housing? Washington, DC, Urban Institute, 2001Google Scholar
3. Bebout RR, Harris M: In search of pumpkin shells: residential programming for the homeless mentally ill, in Treating the Homeless Mentally Ill: A Task Force Report of the American Psychiatric Association. Edited by Lamb HR, Bachrach LL, Kass FI. Washington, DC: American Psychiatric Association, 1992Google Scholar
4. Ridgway P, Zipple AM: The paradigm shift in residential services: from the linear continuum to supported housing approaches. Psychosocial Rehabilitation Journal 13:11-31, 1990Crossref, Google Scholar
5. Lipton FR, Nutt S, Sabatini A: Housing the homeless mentally ill: a longitudinal study of a treatment approach. Hospital and Community Psychiatry 39:40-45, 1988Abstract, Google Scholar
6. Drake RE, Yovetich NA, Bebout RR, et al: Integrated treatment for dually diagnosed homeless adults. Journal of Nervous and Mental Disease 185:298-305, 1997Crossref, Medline, Google Scholar
7. Hurlburt MS, Wood PA, Hough RL: Providing independent housing for the mentally ill homeless: a novel approach to evaluating long-term housing patterns. American Journal of Community Psychology 24:291-310, 1996Crossref, Google Scholar
8. Caton CL, Wyatt RJ, Felix A, et al: Follow-up of chronically homeless mentally ill men. American Journal of Psychiatry 150:1639-1642, 1993Link, Google Scholar
9. Susser E, Valencia E, Conover S, et al: Preventing recurrent homelessness among mentally ill men: a "critical time" intervention after discharge from a shelter. American Journal of Public Health 87:256-262, 1997Crossref, Medline, Google Scholar
10. Kuhlman TL: Psychology on the Streets: Mental Health Practice With Homeless Persons. New York, Wiley, 1994Google Scholar
11. Houghton T: A Description and History of the NY/NY Agreement to House Homeless Mentally Ill Individuals. New York, Corporation for Supportive Housing, 2001Google Scholar
12. Kennedy SG: New look for SRO's: decent housing. New York Times, Mar 28, 1995, pp B1-B2Google Scholar
13. Culhane DP, Metraux S, Wachter SM: Homelessness and public shelter provision in New York City, in Housing and Community Development in New York City: Facing the Future. Edited by Schill M. Albany, SUNY Press, 1999Google Scholar
14. Culhane DP, Metraux S: Assessing relative risk for homeless shelter usage in New York City and Philadelphia. Population Research and Policy Review 18:219-236, 1999Crossref, Google Scholar
15. Culhane DP, Metraux S: Where to from here: a policy research agenda based on the analysis of administrative data, in Understanding Homelessness: New Policy and Research Perspectives. Edited by Culhane DP, Hornburg SP. Washington DC, Fannie Mae Foundation, 1997Google Scholar
16. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69-71, 1992Abstract, Google Scholar
17. Smith HL: Matching with multiple controls to estimate treatment effects in observational studies. Sociological Methodology 27:325-353, 1997Crossref, Google Scholar
18. Rubin DB: Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine 127:757-763, 1997Crossref, Medline, Google Scholar
19. Levy CJ: Broken homes: a final destination. New York Times, Apr 28, 2002, pp A1,A8-10Google Scholar
20. Winerip M: Bedlam on the streets. New York Times Magazine, May 23, 1999, pp 42-49,56, 63-64,70Google Scholar



