Pathways Into and Through Mental Health Services for Children and Adolescents
Abstract
OBJECTIVE: This study examined points of entry into the mental health service system for children and adolescents as well as patterns of movement through five service sectors: specialty mental health services, education, general medicine, juvenile justice, and child welfare. METHODS: The data were from the Great Smoky Mountains Study, a longitudinal epidemiologic study of mental health problems and service use among youths. The sample consisted of 1,420 youths who were nine, 11, or 13 years old at study entry. Each youth and a parent were interviewed at baseline and every year thereafter about the use of services for mental health problems over the three-year study period. RESULTS: Population estimates indicated that 54 percent of youths have used mental health services at some time during their lives. The education sector was the most common point of entry and provider of services across all age groups. The specialty mental health sector was the second most common point of entry for youths up to age 13 years, and juvenile justice was the second most common point of entry for youths between the ages of 14 and 16. Youths who entered the mental health system through the specialty mental health sector were the most likely to subsequently receive services from other sectors, and those who entered through the education sector were the least likely to do so. CONCLUSIONS: The education sector plays a central role as a point of entry into the mental health system. Interagency collaboration among three primary sectors—education, specialty mental health services, and general medicine—is critical to ensuring that youths who are in need of mental health care receive appropriate services.
In the past two decades, increased attention has been given to the inadequacies of mental health services provided for children and adolescents (1) as well as attempts to develop, implement, and expand a revised paradigm of care (2,3,4). This revised paradigm is centered on the concept of a system of care that emphasizes individualized services, child- and family-centered planning and service delivery, and coordination among multiple providers and their respective agencies (3). Despite the growing emphasis on the provision of services across time and providers, remarkably little is known about how children and adolescents actually use mental health services.
Much of the work on mental health services for youths has focused narrowly on services provided in inpatient or outpatient mental health settings. Studies of youths with serious emotional disturbance and recent studies of general population samples have shown that, as a result of this narrow focus, many other types of services that youths receive for mental health problems are excluded (5,6,7,8,9,10).
It is known that many youths with emotional and behavioral problems use a variety of types of mental health services during childhood and adolescence (11). It is also known that many youths receive mental health services outside the mental health sector (12). Our analysis focused on four specific questions. First, how many youths in the general population receive services for a mental health problem? Second, where do youths first enter the service system? Third, given their point of entry, what are their subsequent patterns of service use? Finally, how does the severity of an individual's mental health problems and other demographic factors relate to his or her patterns of service use?
Methods
Data
The data described in this study are from the Great Smoky Mountains Study, a longitudinal epidemiologic study of mental health problems and service use in a predominantly rural region of the southeastern United States (13,14). The study began in 1993 and is ongoing. A total of 4,500 youths aged nine, 11, and 13 years were randomly selected from all public school districts in 11 participating counties. Two-stage sampling was used to ensure adequate numbers of youths with psychiatric problems and service use. A screening questionnaire based on externalizing items from the Child Behavior Checklist (15) was used to oversample youths with behavioral problems. Parents completed the questionnaire by telephone or, if the family did not have a telephone, in person. Of the 4,500 families selected, a total of 433 (9.6 percent) were found to be ineligible—for example, the child's date of birth was incorrect in school records or the family no longer resided in the area. Of the 4,067 eligible families, 3,896 (95.8 percent) completed the screening questionnaire. All youths with scores above a predetermined cutoff point, as well as a 10 percent sample of youths with lower scores, were recruited into the study. This process resulted in a sample of 1,346 youths, 1,073 (80 percent) of whom participated in the study.
The target geographic region includes the Qualla Boundary, home to the Eastern Band of the Cherokee Nation. Because many of the American Indian youths attended reservation schools, they were not included in the sampling frame for the main study. Therefore, a parallel study was conducted in the same geographic region and included all nine-, 11-, and 13-year-old American Indians in the area. Thus 431 American Indian youths were identified, 347 (80 percent) of whom participated in the study.
Data from the Great Smoky Mountains Study are weighted so that the two samples and the two-stage sampling approach reflect the general population (13). The weights are inversely proportional to the sampling probability for youths selected through the two-stage sampling and reflect the known population proportion of American Indians in the 11-county region. The numbers (Ns) reported throughout this article are the actual numbers of interviewed families, and all percentages are weighted to reflect the population from which the sample was selected.
Combining the samples resulted in a total sample of 1,420 youths who entered the study when they were aged nine, 11, or 13 years. Demographic and mental health characteristics of the sample are summarized in Table 1. The sample was predominantly white, which is consistent with the racial distribution of the participating region, and nearly 30 percent of the youths lived in poverty according to the federal definition of poverty. Rates of mental health problems reflect the proportion of youths who met criteria for a psychiatric diagnosis, functional impairment, or both (serious emotional disturbance) during any of the four annual waves of data collection. Nearly 40 percent of the youths met criteria for a diagnosis or impairment, and an additional 15 percent met the criteria for serious emotional disturbance.
Data from the Great Smoky Mountains Study provide a unique opportunity to address questions about children's and adolescents' use of mental health services. First, because the sample is representative of the general population, it can be used to explore patterns of entry and service use among youths with mild problems as well as among those with serious problems. Second, detailed prospective data about service use among youths are available for three years, and additional retrospective data on lifetime use of services are available. Third, the study conceptualizes mental health services broadly. Data are available on services that are traditionally categorized as mental health services, referred to in this article as specialty mental health services, such as services provided by psychiatric hospitals, community mental health centers, psychologists, and psychiatrists in private practice as well as mental health services provided in other sectors, such as schools, the child welfare sector, the general medicine sector, the juvenile justice sector, and in the community.
Data collection
Each youth and a parent (the biological mother in 84 percent of cases) were interviewed at baseline and annually thereafter. Interviews were conducted separately with the parent and the youth by different interviewers. In addition, parents were contacted every three months between annual waves to provide updated information on service use. These interviews were conducted by telephone or, for families without a telephone, in person. The data reported in this article include four waves of annual data and associated quarterly follow-up interviews.
Measures
The analyses centered on two instruments: the Child and Adolescent Psychiatric Assessment (CAPA) (16,17) and the Child and Adolescent Services Assessment (CASA) (18,19).
Child and Adolescent Psychiatric Assessment. The CAPA assesses psychiatric symptoms and associated functional impairment (16,17,20). One-week test-retest reliability among youths from inpatient and outpatient settings was 1.0 for substance abuse or dependence, greater than .80 for depression and dysthymia, .65 to .75 for anxiety disorders, and .55 for conduct disorder. The lower reliability for conduct disorder can be accounted for in part by attenuated reports at the second interview by youths who admitted to lying during the first interview.
To simplify data on diagnoses and functional impairment, we combined parent and youth data and classified youths at each annual interview into one of three categories of mental health. The first category included youths with serious emotional disturbance. These youths met DSM-III-R criteria for a well-defined emotional or behavioral disorder and reported additional functional impairment. The second category included youths who either reported functional impairment but did not meet DSM-III-R criteria for a disorder or who met diagnostic criteria but did not report significant additional impairment. The final category included youths who had neither a DSM-III-R diagnosis nor substantial functional impairment. Such youths may display no symptoms of a psychiatric disorder or may have symptoms that are below the threshold required to meet diagnostic criteria.
Child and Adolescent Services Assessment. The CASA gathers information from parents and youths about more than 30 types of services that youths might use to address behavioral or emotional problems (18,19). For each type of service, the respondent indicates whether the youth has ever used that service, and, if so, whether the youth used the service during the three months preceding the interview. If the youth has ever used the service, the respondent is asked for the date of first use of the focal service type. For services used in the past three months, additional information is collected about the volume and content of treatment. For the analyses reported here, services were categorized into five sectors: the specialty mental health sector, including inpatient and outpatient services; the education sector; the child welfare sector; the juvenile justice sector; and the general medicine sector. Test-retest reliability for the CASA is good to excellent (k=.4 to .6 for school services, k=.5 to .8 for outpatient services, and k=.6 to 1.0 for inpatient, out-of-home, and juvenile justice services) (18,19). Comparisons with provider records showed 90 percent agreement on whether services were received (18).
Analysis
In the first portion of the results section, details are provided on the proportion of youths who used services and the types and amount of services they received. Subsequent analyses examined pathways into and through care for youths and examined factors related to service use patterns. Much of the analysis focused on frequencies and descriptive statistics. All analyses for which statistical significance is reported were run with the use of sandwich estimators to properly account for the weighted data and to provide accurate parametric estimates and standard errors of the mean (20).
Missing data. In the Great Smoky Mountains Study data set, very few data are missing within interviews. However, data are missing because of attrition or because parents did not complete all quarterly interviews. All four annual in-person interviews were completed by 994 (70 percent) of the families, and an additional 241 (17 percent) completed three of the four annual interviews. A majority of parents (89 percent, N=1,264) also provided information during at least one of the three interim interviews that occurred between the annual interviews. Families with complete data were somewhat less likely than families with missing data to be living in poverty (35 percent compared with 45 percent; χ2=11.8, df=1, p<.001) but did not differ significantly on other factors, such as the child's age, sex, race, psychiatric diagnoses, or functional impairment.
To examine the possible effect of missing data on the results, we imputed data by using a method that borrows from both regression and hot deck imputation (22). This method calculates the empirical distribution of the missing data conditional on the value observed in the nearest available neighbor and imputes the missing value from this empirical distribution. Comparison of nonimputed and imputed data showed only minimal differences in service use rates; the nonimputed data were slightly more conservative. All analyses were run with the use of both imputed and nonimputed data with, as appropriate, a variable indicating the number of missing waves. The imputed data did not lead to any conclusions different from those derived from the nonimputed data. Therefore, results of the analyses run with imputed data are not presented.
Time frames. We present the prevalence of service use for three time frames: one year, three years, and lifetime. The three-year period started at the conclusion of the baseline interview and continued through the wave 4 annual interview. Use of this time frame allowed us to make a temporally clean distinction between baseline characteristics of the youths and their families and service use during the subsequent three-year interval. Estimates of one-year prevalence of service use are included to facilitate comparisons with other studies that used this more common time frame. Lifetime service use covered birth through ages 12 to 16 years (depending on how old the youths were when they entered the study). True lifetime estimates would likely be higher than those reported here, because none of the youths have yet "aged out" of the period of potential service use.
Results
Use of mental health services
Population estimates for three years indicated that 632 youths (33.6 percent) received services for emotional, behavioral, or substance use problems from one or more of the five service sectors. As shown in Table 2, services were provided most often by the education sector (470 youths, or 24.1 percent). Specialty mental health services were used by 265 youths (14.2 percent of the population).
During any year, service use was approximately half that observed for the full three years. Overall, in any given year, 18 to 19 percent of the population used services from one or more sectors. Approximately 11 percent of youths used education services, 7 percent used specialty mental health services, 4 percent used general medical services, and 1 to 2 percent used child welfare or juvenile justice services.
Population estimates of lifetime service use (birth through wave 4 interview) were slightly less than two times those seen during the focal three-year period. At some point in their lives, approximately half (54 percent) of the population used services from one or more of the five sectors. Services from the education sector were most common (42 percent), followed by specialty mental health services (24 percent), general medicine services (15 percent), and child welfare or juvenile justice services (4 percent to 7 percent).
Entry points
More than half (60.1 percent) of all youths who received services at some time during their lives entered the service system by first receiving services from the education sector (Table 3). Approximately a quarter (27.3 percent) entered the service system through the specialty mental health sector, and 12.9 percent gained access through the general medical sector. Few service users gained access through the child welfare or juvenile justice system.
Approximately 9 percent of youths who used services entered through more than one sector simultaneously, meaning that we could not determine the order of entry from the data. It is likely that many simultaneous entries were actually sequential, with the time between entry to different sectors being quite short and probably being viewed by the parent and the child as part of a single episode. Compared with the 23 percent of single-sector entrants who entered through specialty mental health, 75 percent of youths who entered the system through multiple sectors entered through this sector.
Use of multiple sectors
Overall, 45 percent of service users received services from more than one sector (either concurrently or sequentially). Youths who entered services through multiple sectors simultaneously, by definition, met the criteria for multiple-sector use. Youths who entered the service system through single sectors had different probabilities of using additional sectors according to the sector of entry (χ2=48.2, df=4, p=.001). The use of additional sectors was most common among youths who initially entered services through the specialty mental health sector (62 percent) and least common among youths initially entering through the education sector (31 percent). Those who entered through the child welfare, juvenile justice, or general medicine sectors fell between these extremes (36 percent, 40 percent, and 47 percent, respectively).
Service mix and sequence
Service mix and sequence are reported for youths who entered services through the education sector, the specialty mental health sector, the general medicine sector, or multiple sectors. The number of youths who entered through the juvenile justice or child welfare sector was too small to warrant detailed analysis of subsequent patterns of sector use. To identify the actual sequence of sectors in which individual youths received services, we constructed string variables that describe the chain of services used. Chains that included at least five youths and represented the sector sequences of at least 2 percent of the entry sector are reported.
Education sector. As described above, the education sector was the most common point of entry into mental health services for youths and also the point of entry that was least likely to be followed by involvement with other sectors. Consequently, the most common chain of services for youths who entered services through this sector was a single-link chain consisting of only the education sector. Among the youths who entered services through the education sector and who used subsequent services, chains that began with this sector and that included just one other sector were the most common (76 percent of multisector users). Among the two-sector chains, the most common subsequent sector was the specialty mental health sector (58 percent) or the general medicine sector (28 percent).
Specialty mental health sector. In contrast with youths who entered services through the education sector, a majority of youths who entered services through the specialty mental health sector (62 percent) used services from additional sectors. These additional sectors included the education sector (57.5 percent), the general medicine sector (29.8 percent), and the child welfare sector (20.6 percent).
Twenty-seven different chains of service use were observed for youths who entered mental health services through the specialty mental health sector. These chains ranged from a single-link chain (specialty mental health only) to eight different four- to five-sector chains. Despite this complexity, 71 percent of the youths who entered services through this sector fit into one of two simple chains. The most common (38 percent of specialty mental health entrants) was a single-sector chain comprising only specialty mental health services. The next most common pattern (32.4 percent of sector entrants) was a two-sector chain beginning with specialty mental health services and including subsequent services in education.
General medicine sector. The general medicine sector fell between the extremes noted for the education sector and the specialty mental health sector in terms of entrants who went on to use other sectors. Of youths who entered mental health services through the general medicine sector, 47 percent subsequently received services from one or more additional sectors. As with the education and specialty mental health sectors, the most common chain was a single link consisting of only the general medical sector (53 percent). Seventeen additional chains were observed, but only four of these described the sector sequences of at least 2 percent of entrants. The most common of these were two-sector chains that included the general medicine sector, followed by the education sector (12.1 percent) and the general medicine sector, followed by the specialty mental health sector (10.5 percent). Observed three-sector chains included the general medicine, specialty mental health, and education sectors (9.6 percent) and the general medicine, education, and specialty mental health sectors (3.7 percent).
Multiple-sector entry. Of the 9.1 percent of youths who entered services through more than one sector simultaneously, most had the specialty mental health sector as one of their points of entry. The most common combinations were the specialty mental health and education sectors (29 percent of multisector entrants), the specialty mental health and child welfare sectors (26.5 percent), and the specialty mental health and general medicine sectors (18 percent). The only other combination that included at least 2 percent of multisector entrants was the education sector and the general medicine sector (13 percent). Multiple-sector entry seems to capture a distinct type of service user. For all single-sector entrants, the most common chain of sectors was a single-link chain that included only the sector of entry. By definition, multisector entrants could not display this simple pattern of service use. Beyond this definitional difference, very few multisector entrants received services only from the sectors through which they entered. Of youths who entered through multiple sectors, 95.4 percent displayed a service-sector chain that included at least one sector in addition to the sectors through which they entered.
Duration of service use
We examined the duration of service use during the three focal years of data collection for the Great Smoky Mountains Study. Among youths who received any services during this 36-month period, 38 percent received services for three months or less, 47 received services for three to 12 months, and only 14 percent used services for 12 months or more.
Factors related to sector of entry
Problem severity. It was possible to examine the relationship between the severity of youths' problems around the time of entry and the sector of entry for the three-year period of the Great Smoky Mountains Study and thus for youths who first used services during this period. We designated the annual interview that was temporally closest to the time of service entry to determine clinical status at entry.
Among youths who entered services during the three-year focal period, 55 percent did not meet criteria for a DSM-III-R diagnosis or functional impairment near the time of service entry. A total of 57 percent of this mildly troubled group entered services through the education sector. Of those with the least severe problems, an additional 14 percent entered services through multiple sectors, 13 percent through general the general medicine sector, 9 percent through the juvenile justice sector, 6 percent through the specialty mental health sector, and less than 1 percent through the child welfare sector. At the other extreme, youths with serious emotional disturbance were overrepresented as entrants through multiple sectors (30 percent of serious emotional disturbance entrants) and the general medicine sector (36 percent), and they were less likely than other youths to enter through the education sector (22 percent).
Among youths with a psychiatric diagnosis or functional impairment (but not both), approximately half entered services through the education sector, and approximately 15 percent entered through the specialty mental health sector. Youths with a psychiatric diagnosis only were nearly as likely as youths with serious emotional disturbance to enter services through the general medicine sector (30 percent of diagnosis-only entrants). Youths with functional impairment only were virtually the only youths to enter services through the child welfare sector (9 percent of impaired entrants).
Age. Youths of different ages had different probabilities of entering the various service sectors. Overall, very few youths entered services before the age of five years or after the age of 13 years (4 percent and 7 percent, respectively). Thirty-four percent entered between the ages of five and eight years. Slightly more than half of all service users entered services between ages nine and 13 years (55 percent).
Across all age groups, the education sector was the most common point of entry. For youths who entered services before the age of five years, 44 percent entered through this sector; for those who entered services between the ages of five and eight, 48 percent; for youths who entered between the ages of nine and 13 years, 62 percent; and for youths who did not enter services until after the age of 13 years, 52 percent. However, the second most common sector of entry differed by age group. For children up to age 13, the specialty mental health sector was the second most common point of entry (34 percent for those younger than five years, 23 percent for those aged five to eight years, and 18 percent for those aged nine to 13 years). For youths who entered services between ages 14 and 16, the juvenile justice sector was the second most common sector of entry (18 percent).
Sex and ethnicity. Overall, the sector of entry was not significantly different between the sexes or across racial groups. The only significant effect was that African American youths tended to be more likely than white youths to enter services through the child welfare sector (χ2=8.75, df=1, p=.003). Otherwise, boys, girls, African Americans, American Indians, and whites displayed very similar patterns of entry into services in this predominantly rural region.
Factors related to multiple-sector strings
As noted above, youths who entered services through the education sector were the least likely to subsequently use other sectors. Logistic regression was used to examine whether education per se was associated with lower subsequent use or whether the education sector was simply serving a type of youth who was unlikely to receive subsequent services, regardless of point of entry. Even after we controlled for severity of problems, age at entry, sex, and race, youths who entered services through the education sector were significantly less likely to receive subsequent services from other sectors than youths who entered through any other sector (odds ratio=.16, 95 percent confidence interval=.08 to .34).
Discussion
Despite recent efforts aimed at interagency collaboration and development of a coordinated system of mental health services for youths, little is known about how youths actually move into and through the various sectors that provide mental health services. Our analyses showed that about half of all youths in a general population sample used some form of mental health service during their childhood or adolescence. Nearly half of these service users were treated in the specialty mental health sector, three-quarters received services in the education sector, and more than one-quarter received services in the general medical sector. The juvenile justice sector and the child welfare sector each served 8 percent to 12 percent of youths who used services.
The education sector was both the most common point of entry into services and the most prevalent service provider. Youths who entered services through the education sector were the least likely to meet criteria for psychiatric diagnoses. The education sector was also the entry sector with the fewest and shortest chains of subsequent service use. This lack of additional services seems to be explained in part by the types of problems of youths who have gained access to services through education. However, when the severity of problems and other factors are taken into account, entry through education decreased the probability that youths would receive services in subsequent sectors.
By contrast, entry through the specialty mental health sector was associated with more severe disturbance and a greater likelihood of entry into additional service sectors. Specialty mental health also served disproportionately as a point of service entry for youths who first entered services before the age of nine years and stands out because of its role in multiple-sector service entry. Relatively few youths who entered services through the mental health sector were single-sector entrants. Rather, specialty mental health services seem to be part of a package of services delivered as a starting point in a youth's service history.
The observed sequences of service use show a predominance of the education sector and highlight the importance of interagency collaboration among three primary sectors: education, specialty mental health, and general medicine. These three sectors accounted for a majority of all services used by children and adolescents. The child welfare and juvenile justice sectors both served as entry points for some youths and were involved in chains of subsequent service use for others. However, in this general population sample these sectors were only marginally involved in the provision of services.
The Great Smoky Mountains Study provides a unique and powerful data set for examining these issues. However, it also has limitations. All data on service use before study entry—for example, for children aged nine to 13 years—are retrospective. Detailed data on psychiatric diagnosis and impairment are available only for the period of data collection for the Great Smoky Mountains Study. The region included in the sample is predominantly rural and has a children's mental health system that is relatively well developed and has made substantial efforts during the past decade to increase interagency collaboration and cooperation. Thus patterns of service use may not be comparable with those found in urban areas or rural areas with less-developed systems.
Conclusions
The results of this study illuminate ways in which youths with emotional, behavioral, or substance use problems move into and through service sectors. They provide a generally encouraging picture of triage among the sectors. Education, the sector with which all youths have contact, was the point of entry for the largest number of youths, especially in the case of youths who did not have a psychiatric diagnosis.
The specialty mental health sector was the second most common point of entry. Youths who initially entered services through this sector were more likely than youths who entered through the education sector to have a psychiatric diagnosis or functional impairment. The specialty mental health sector was also the sector that was most likely to act simultaneously as a point of entry with another sector and was a common subsequent provider for youths who initially entered services through other sectors. This finding suggests that the specialty mental health sector may occupy a niche as a point of entry for more seriously troubled and multisector youths as well as a follow-up for other services.
These findings support the centrality of the education sector as a provider of services for youths with mental health problems (9,23,24). They also raise the question of exactly what role education plays in the mental health service system. There is evidence that the education sector is a point of entry and a provider of services for youths who have less-severe problems. Thus the fact that youths who entered the service system through the education sector were unlikely to use additional sectors seems appropriate. However, there was also evidence that, when the severity of problems, age, sex, and race were controlled for, youths who initially entered the service system through the education sector were less likely to subsequently use services from other sectors. Only a quarter of youths who entered services through the education sector received any subsequent specialty mental health services. This finding may suggest that, for at least some youths who enter services through the education sector, links to subsequent service sectors are not being made.
These results also suggest that the current emphasis of systems of care for youths with serious emotional disturbance may be too narrowly focused. Although youths with serious emotional disturbance tend to show more complicated and extended patterns of service use and to use services in more sectors, it is clear that these are not the only youths with such patterns of service use. It seems to be crucial to facilitate linkages between service sectors. In particular, because the education sector serves as the initial point of entry for a majority of youths with problems, it is crucial that appropriate linkages be made between the education system and other sectors. In addition, the medical sector was the point of entry for 13 percent of service users. Those who entered through this sector tended to meet the criteria for psychiatric diagnoses, either with or without substantial functional impairment. However, fewer than half of them ever received services from any other sector.
This article presents an initial view of service patterns in a representative population of children and adolescents. Additional studies are needed to examine detailed information on help seeking and linkages among agencies and service providers. The results of this study show that 45 percent of service users received services from multiple sectors. We do not know why these service users started in a given sector, how many providers they saw within a sector, which specific services they received, or how linkages were made with other sectors or providers. We also do not know whether, for youths who did not use multiple sectors, such patterns reflect appropriate care or indicate a lack of adequate linkages within the system. Future work is needed to further understand the processes that influence observed patterns and outcomes associated with such variations in patterns of care.
The authors are affiliated with the department of psychiatry and behavioral science at the Duke University School of Medicine in Durham, North Carolina. Send correspondence to Dr. Farmer at the Department of Psychiatry and Behavioral Science, Services Effectiveness Research Program, Duke University School of Medicine, DUMC Box 3454, Durham, North Carolina 27710 (e-mail, [email protected]).
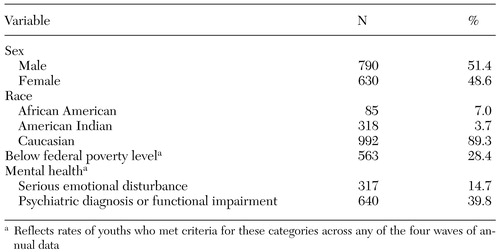 |
Table 1. Characteristics of a sample of 1,420 children and adolescents who participated in a study of mental health problems and service use
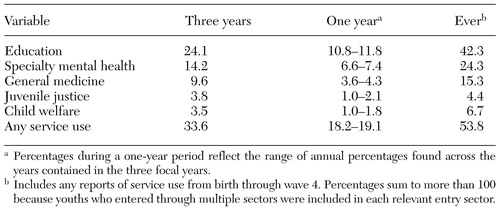 |
Table 2. Population-based rates (%) of service use among children and adolescents
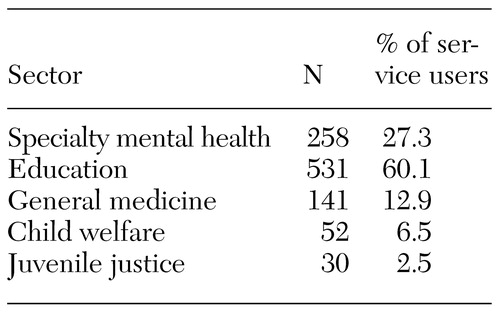 |
Table 3. Service entry by sector in a sample of children and adolescents
1. Knitzer J: Unclaimed Children: The Failure of Public Responsibility of Children and Adolescents in Need of Mental Health Services. Washington, DC, Children's Defense Fund, 1982Google Scholar
2. England MJ, Cole RF: Building systems of care for youth with serious mental illness. Hospital and Community Psychiatry 43:630-633, 1992Abstract, Google Scholar
3. Stroul BA, Friedman RM: A System of Care for Children and Youth With Severe Emotional Disturbances. Washington, DC, CASSP Technical Assistance Center, 1986Google Scholar
4. Lourie IS, Stroul BA, Friedman RM: Community-based systems of care: from advocacy to outcomes, in Outcomes for Children and Youth with Behavioral and Emotional Disorders and their Families: Programs and Evaluation Best Practices. Edited by Epstein MH, Kutash K, Duchnowski A. Austin, Tex, PRO-ED, 1998Google Scholar
5. Burchard JD, Burchard SN, Sewell R, et al: One Kid at a Time: Evaluative Case Studies and Descriptions of the Alaska Youth Initiative Demonstration Project. Washington, DC, Georgetown University Press, 1993Google Scholar
6. Burns BJ, Gwaltney EA, Bishop GK: Case management research: issues and directions, in From Case Management to Service Coordination for Children with Emotional, Behavioral, or Mental Disorders: Building on Family Strengths. Edited by Friesen BJ, Poertner J. Baltimore, Md, Brookes, 1995Google Scholar
7. Cohen P, Kasen S, Brook J, et al: Diagnostic predictor of treatment patterns in a cohort of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 36:989-993, 1992Google Scholar
8. Greenbaum PE, Dedrick RF, Friedman RM, et al: National Adolescent and Child Treatment Study (NACTS): outcomes for children with serious emotional and behavioral disturbance. Journal of Emotional and Behavioral Disorders 4:103-146, 1996Crossref, Google Scholar
9. Staghezza-Jaramillo B, Bird HR, Gould MS, et al: Mental health service utilization among Puerto Rican children ages 4 through 16. Journal of Child and Family Studies 4:399-418, 1995Crossref, Google Scholar
10. Stroul BA: Systems of Care for Children with Severe Emotional Disturbances: What Are the Results? Washington, DC, CASSP Technical Assistance Center, 1993Google Scholar
11. Silver SE, Duchnowski A, Kutash K, et al: A comparison of children with serious emotional disturbances served in residential and school settings. Journal of Child and Family Studies 1:43-59, 1992Crossref, Google Scholar
12. Staghezza-Jaramillo B, Burd HR, Gould MS, et al: Mental health services utilization among Puerto Rican children ages 4 through 16. Journal of Child and Family Studies 4:399-418, 1995Crossref, Google Scholar
13. Costello EJ, Angold A, Burns BJ, et al: The Great Smoky Mountains Study of Youth: functional impairment and serious emotional disturbance. Archives of General Psychiatry 53:1137-1143, 1996Crossref, Medline, Google Scholar
14. Costello EJ, Angold A, Burns BJ, et al: The Great Smoky Mountains Study of Youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry 53:1129-1136, 1996Crossref, Medline, Google Scholar
15. Achenbach TM, Edelbrock, C: Manual for the Child Behavior Checklist and Child Behavior Profile. Burlington, University of Vermont, 1993Google Scholar
16. Angold A, Costello EJ: A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C). Psychological Medicine 25:755-762, 1995Crossref, Medline, Google Scholar
17. Angold A, Costello EJ: The Child and Adolescent Psychiatric Assessment (CAPA). Journal of the American Academy of Child and Adolescent Psychiatry 39:39-48, 2000Crossref, Medline, Google Scholar
18. Ascher BH, Farmer EMZ, Burns BJ, et al: The Child and Adolescent Services Assessment (CASA): description and psychometrics. Journal of Emotional and Behavioral Disorders 4:12-20, 1996Crossref, Google Scholar
19. Farmer EMZ, Stangl DK, Burns BJ, et al: Reliability of self-reported services use: test-retest consistency of children's responses to the Child and Adolescent Services Assessment (CASA). Journal of Child and Family Studies 3:307-325, 1994Crossref, Google Scholar
20. Angold A, Prendergast M, Cox A, et al: The Child and Adolescent Psychiatric Assessment (CAPA). Psychological Medicine 25:739-753, 1995Crossref, Medline, Google Scholar
21. Binder DA: On the variances of asymptotically normal estimators from complex surveys. International Statistical Review 51:279-292, 1983Crossref, Google Scholar
22. Little RJA, Rubin DB: Statistical Analysis with Missing Data. New York, Wiley, 1987Google Scholar
23. Burns BJ, Farmer EMZ, Angold A, et al: A randomized trial of case management for youth with serious emotional disturbance. Journal of Clinical Child Psychology 25:476-486, 1996Crossref, Google Scholar
24. Farmer EMZ, Stangl DK, Burns BJ, et al: Use, persistence, and intensity: patterns of care for children's mental health across one year. Community Mental Health Journal 35:31-46, 1999Crossref, Medline, Google Scholar



