Gambling Disorders Among Homeless Persons With Substance Use Disorders Seeking Treatment at a Community Center
Abstract
OBJECTIVES: Epidemiological research suggests that homelessness is a risk factor for elevated levels of psychiatric comorbidity and other health risks. This study examined the prevalence of disordered gambling and its association with treatment of psychiatric and substance use disorders among a cohort of homeless people seeking treatment at a community services program. METHODS: Between 1998 and 2000, intake workers evaluated the level of gambling disorder among 171 consecutive homeless persons with substance use disorders who sought treatment at the Moving Ahead Program in Boston. Program staff administered the DSM-IV subscale of the Massachusetts Gambling Screen at intake. RESULTS: The prevalence rates of level 2 and level 3 gambling disorders were 12.8 percent and 5.5 percent, respectively. These rates are higher than that of the general adult population but comparable to those of other patients with substance use disorders and psychiatric diagnoses. Program participants with level 3 gambling disorders had been homeless more often and at a younger age and had had less substance abuse treatment and more psychiatric treatment than participants with level 1 or level 2 gambling disorders. Participants with level 2 gambling disorders had been homeless more often and for a longer duration than participants without gambling disorders. CONCLUSIONS: These findings should encourage clinicians working with homeless people to screen for gambling-related problems and disorders.
Intake workers and other treatment providers often overlook the possibility of gambling-related problems among the profoundly poor. Recent research has demonstrated an elevated rate of probable pathological gambling among persons who are at least partially dependent on community centers for food assistance, material assistance, or lodging (1). Homeless people accounted for a segment of the cohort of Lepage and associates (1), but they were not distinguished from the others who also sought help at community centers.
Homelessness is a serious public health problem. Investigators have studied the epidemiology of homelessness across an array of health concerns. For example, homeless persons have higher levels of diseases and disorders of the digestive, nervous, and respiratory systems than persons who are not homeless (2). In addition, the homeless have unmet physiological and safety needs and are deficient in self-esteem (3). A 1998 report of the International Union of Gospel Missions summarized results of a nonscientific survey of self-selected respondents. The survey found that 18 percent of men and women at rescue missions believe that gambling is one reason for their homelessness and that 70 percent believe that the prevalence of gambling opportunities had inhibited them from bettering their lives (4). The study reported here provides the first scientific estimates of gambling disorders in a cohort of homeless people who sought treatment.
Recent evidence has demonstrated that the prevalence estimates of disordered gambling are lowest among adults in the general population, are higher among adolescents and college students, and are highest among prison inmates and patients receiving treatment for substance abuse and other disorders (5,6,7,8,9,10,11,12,13). In one of the first comprehensive reviews of pathological gambling (14) and the first effort to provide a public health perspective on the problem (15), investigators concluded that vulnerable population segments represent high-risk groups that require additional study.
Homelessness is an important health risk. Studies have described the higher prevalence of mental illness (16), drug and alcohol abuse (2,16), and depression and loneliness (17) among the homeless population. These issues are exacerbated by specific health care problems, such as lack of coordinated medical care and lack of knowledge of health maintenance activities (18). In addition, homeless persons have been found to show little regard for their personal health and to have inadequate coping and life management skills (18). Poverty also is often associated with greater financial risk taking, perhaps because of the psychoeconomics of gambling (19). For example, people of lesser means play the lottery more than people of greater means (20). People living in poverty perceive greater potential to change their lives from a gambling win than people living in wealth. In addition, people with wealth perceive little opportunity to change their lives from a gambling win—unless the magnitude of the potential win reaches a particularly meaningful level. This psychoeconomic driving force is powerful; it can subdue forces in the social setting that encourage abstinence or moderation.
The epidemiology of gambling disorders suggests that homelessness is a risk factor for elevated levels of psychiatric comorbidity. The co-occurrence of these problems suggested three primary hypotheses for this study. First, we hypothesized that homelessness would be associated with a higher prevalence of disordered gambling than in the general population. Research has demonstrated that gambling and substance abuse are often comorbid (8,13). Thus we expected the most serious level of gambling disorder—level 3, or pathological gambling—to be associated with more psychosocial problems than subclinical (level 2) or asymptomatic (level 1) gambling disorder. Finally, we expected greater rates of alcohol and drug treatment experience among homeless people seeking treatment who have also experienced co-occurring gambling disorders.
Methods
Participants and setting
The participants were 171 consecutive homeless persons seeking treatment at the St. Francis Moving Ahead Program in Boston between 1998 and 2000. Among these program participants, 88 (51.5 percent) reported having a history of psychiatric treatment.
The Moving Ahead Program provides an intensive 14-week plan for homeless persons who have a history of substance abuse and are seeking treatment. Program components include assessment of job readiness, preemployment training, life skills training, job placement assistance, and work experience. The full-time, five-days-a-week curriculum blends counseling, self-assessment, skills development, and work experience. The goal is to develop the self-efficacy and daily living and work skills necessary for homeless adults to gain the confidence and resources needed to change their lives. The program provides homeless persons a chance to change their lifestyle by offering training activities essential to attaining self-sufficient, independent living.
The job readiness component of the Moving Ahead Program includes a six-week internship or trial work period, which begins during the seventh week of the program. The "students," or clients, begin an internship developed by program staff members to reflect each student's special interests. Students work at their internship sites about 14 to 16 hours a week.
Inclusion criteria
Those who seek entry into the Moving Ahead Program must meet several criteria. They must be at least 18 years old; they must be, or recently have been, homeless (at the time of admission, they must be residing in a residential program); they must have a history of substance abuse; and they must be committed to returning to work. Once admitted to the program, they receive a weekly stipend to help with living expenses while they are enrolled.
Dependent measures
This study used the Massachusetts Gambling Screen (21) adaptation of DSM-IV (22) criteria for pathological gambling. The Massachusetts Gambling Screen is a 12-item questionnaire designed to screen for pathological gambling according to DSM-IV criteria. The instrument is scored as follows: a value is assigned for each yes and each no response to the questions, and the points are tallied. The designation of nonpathological gambler or pathological gambler is made on the basis of a total score of less than 5 or of 5 or more, respectively.
In this study, the DSM-IV subscale of the Massachusetts Gambling Screen yielded an item Cronbach's alpha reliability coefficient of .91; this index provides evidence that the DSM-IV subscale was very reliable in a clinical application with a homeless population (23).
Procedures
Staff of the Moving Ahead Program interviewed all treatment seekers during the intake process and administered the DSM-IV subscale of the Massachusetts Gambling Screen as part of the program's standard intake protocol. Information obtained included psychosocial, vocational, legal, and medical history. The data were classified according to the universal classification system first suggested by Shaffer and Hall (24) to minimize pejorative language and provide guidance to public health planners.
This classification system can be summarized briefly as follows. Level 1 gamblers are those who either have not gambled or have gambled without experiencing any adverse consequences. As a result, this group is asymptomatic. Level 2 gamblers are those who have experienced any adverse symptoms; some level 2 gamblers are in transition and moving toward level 1 or toward level 3. Level 3 gamblers are those who satisfy the criteria for pathological gamblers as defined by the American Psychiatric Association's diagnostic criteria (22,25,26). Level 4 gamblers are those who meet level 3 criteria and who also seek treatment for their gambling-related problems; this level was created primarily for population-based treatment planning. Since this study examines only those who sought treatment, level 3 and level 4 gamblers are conceptually the same; therefore, only the prevalence of levels 1 through 3 among these treatment seekers is reported.
Results
Since various diagnostic tests have shown that the homogeneity of variance associated with several comparisons of interest is not always equal, we used nonparametric statistical tests, such as the Kruskal-Wallis test, when appropriate, and parametric tests, such as the t test and one-way analysis of variance (ANOVA), when the data satisfied Levene's tests for homogeneity of variance.
Subjects
A total of 164 of the 171 consecutive homeless persons who sought treatment completed all of the dependent measures necessary for this study, yielding an overall completion rate of 96 percent. Table 1 summarizes demographic and other characteristics of the study participants. Participants ranged in age from 18 to 59 years. Their mean age at intake was 36 years. More than half (53 percent) were male, and two (1 percent) were transgender. More than half (94, or 55.6 percent) of the participants identified themselves as white; 49 (29 percent) were African American, and 26 (15.4 percent) were from other ethnic groups. About 70 percent (118 participants) had never been married, 14.8 percent (25 participants) were divorced, 8.3 percent (14 participants) were separated, and 4.7 percent (eight participants) were legally married. Additionally, two (1.2 percent) were living as married, and two (1.2 percent) were widowed.
Ninety-five (71.4 percent) of the participants reported having a job during the previous 12 months: 43 participants (26.5 percent) reported wages and 42 (25.9 percent) reported public assistance to be their major source of support during the previous year. The mean number years of schooling completed was 11.5; 77 participants (45.6 percent) had completed high school or a GED equivalent, 37 (21.9 percent) had completed grade school, 13 (7.7 percent) had completed a two-year college program, and 13 (7.7 percent) had completed a four-year college program.
More than 30 percent of participants reported that they had been homeless only once, 40 (23.8 percent) twice, and 25 (14.9 percent) three times. The mean±SD age when participants first became homeless was 27.57±10.3 years. A total of 133 participants (78.2 percent) reported having previous alcohol treatment, and 137 (80.6 percent) reported having drug treatment. About half of the participants (87, or 51.8 percent) had had psychiatric treatment at some point in their life.
Prevalence of disordered gambling
Because various staff members conducted intake interviews, we tested the distribution of participants with gambling disorders by levels 1, 2, and 3 for interviewer effects. There were no significant patterns across the various interviewers in the program, so the data were aggregated across the interviewers for the remaining analyses. The data from the Massachusetts Gambling Screen yielded past-year estimates for the rates of level 1, level 2, and level 3 gambling disorders among the homeless, substance-abusing persons who sought treatment in the program. Table 2 summarizes these findings.
Gambling and social problems
Homeless persons seeking treatment who had level 3 gambling disorders were different from those with level 1 or level 2 gambling disorders on a variety of measures. Those with level 3 disorders were younger than their non-level 3 counterparts (30.22±8.6 years compared with 36.28±7.8 years; t=2.25, df=166, p<.03), had been homeless more often during their lifetime (χ2=8.359, df=2, p<.05), and became homeless at a younger age (19.1±10.1 years compared with 28.2±10.1 years; t=2.64, df=165, p<.01). In addition, level 3 gamblers had completed fewer years of school (9.88±2.03 compared with 11.70± 2.65; t=1.92, df=161, p<.06).
ANOVA revealed no differences in the previous year's work history—in whether participants held part-time or full-time jobs or did odd jobs or in days worked (all F values were nonsignificant) across levels of gambling. However, program participants with gambling disorders tended to work more than others, but at part-time instead of full-time jobs. For example, level 3 gamblers were almost six times as likely as other treatment seekers to have had odd jobs (odds ratio [OR]=5.94, 95 percent confidence interval [CI]=.94 to 37.62).
Finally, gender was significantly associated with gambling levels (χ2= 15.85, df=4, p<.005). More male than female participants had experienced both level 2 and level 3 gambling disorders; 12 (63 percent) of level 2 gamblers and six (67 percent) of level 3 gamblers were male.
Gambling and previous treatment experience
Significantly fewer participants with level 3 gambling disorders had been in methadone treatment compared with level 1 and level 2 gamblers (χ2= 6.503, df=2, p<.05). In addition, significantly more level 3 participants had received other forms of psychiatric treatment than level 1 and level 2 participants (χ2=7.552, df=2, p< .05). Level 3 gamblers were twice as likely as non-level 3 gamblers to have had a history of additional psychiatric treatment (OR=2.02, 95 percent CI=.77 to 5.31).
Fewer level 3 gamblers completed detoxification services than non-level 3 gamblers (χ2= 5.869, df=2, p<.05). Although level 3 gamblers had completed detoxification services less often, there were no significant differences between level 3 gamblers and their level 2 and level 1 counterparts in the number of times they had entered alcohol treatment or drug treatment.
Discussion and conclusions
The results of this study provide support for each of our primary hypotheses. The study showed that the levels of gambling disorders among this cohort (homeless persons with a history of substance abuse who sought treatment) are higher than those in the general adult population and similar to those of other patients with psychiatric and substance use disorders (13). Also, these estimates are considerably higher than the rates of gambling disorders among the general adult population. Table 3 summarizes these prevalence rates.
In addition, participants with the most serious level of gambling disorder—level 3—experienced an array of psychosocial problems, including more psychiatric treatment for these problems, than participants with level 2 and level 1 gambling disorders. The third hypothesis received only provisional support, since participants with level 3 gambling disorders had experienced more psychiatric treatment than participants with level 1 and level 2 disorders but had entered alcohol and drug treatment at a rate similar to those of their level 1 and level 2 counterparts. Taken together, these findings demonstrate that gambling-related problems among homeless persons who seek treatment are relatively common.
Homeless persons seeking treatment who experience comorbid level 3 gambling disorders can be distinguished from those with level 1 and level 2 disorders on a variety of measures. These differences suggest that homeless treatment seekers with comorbid level 3 gambling disorders have greater access or require more financial resources to permit the incubation or maintenance of a level 3 gambling disorder. This need for money also reflects a psychoeconomic driving force that encourages gambling among the poor.
Skinner (27) was among the first to consider excessive gambling and its relationship to socioeconomic status. He suggested that when the social setting is altered such that the major sources of reinforcement are no longer powerful, then lesser reinforcers gain strength. For homeless persons with limited opportunities for psychosocial reinforcement, gambling and use of intoxicants can gain potency over activities that previously were more important.
Skinner's work also suggests that people require two interactive conditions to develop and maintain a gambling disorder: sufficient leisure time and discretionary income. If either of these factors is absent, gambling disorders will not emerge or will recede. Since participants with level 3 disorders were almost six times as likely as other treatment seekers to have had odd jobs, taking odd jobs might represent an opportunity to simultaneously preserve free time and earn some discretionary income. Nevertheless, the extent to which homeless substance abusers accrue "discretionary" money from odd jobs remains to be determined.
Participants with level 3 gambling disorders entered alcohol and drug treatment programs just as often as those with level 1 and level 2 disorders but completed this treatment less often; they also had received more psychiatric treatment than their counterparts. Thus gambling disorders might interfere with treatment for substance use disorders. Alternatively, disordered gambling might reflect a wholly independent factor that interferes with detoxification while simultaneously encouraging gambling disorders.
Given the range of problems associated with gambling disorders, it is likely that the increased level of comorbid psychiatric issues contributes to treatment dropout (28). Under these circumstances, gambling-related problems pose a risk to successful completion of drug treatment. More research is needed to clarify the complex relationships among these co-occurring problems.
Given the overall prevalence of gambling disorders and related social problems, the findings of this study suggest that treatment providers who care for homeless persons should routinely screen for gambling-related problems just as they should check for substance use and other psychiatric disorders. Once identified by screening efforts, persons with gambling problems should be referred for further evaluation of their gambling and comorbid conditions.
Additional research is needed to determine the likelihood of gambling-related problems among persons seeking treatment who have a history of doing odd jobs instead of holding full-time jobs or remaining unemployed. Until such research is completed, we encourage clinicians simply to screen for gambling-related problems among the homeless population. In addition, we encourage clinicians to include an assessment of the temporal sequencing of psychiatric and social problems, since the specific sequence of symptoms can clarify which disorders are antecedent and consequential and which symptoms increase or decrease the risks associated with developing gambling disorders (29).
Because these findings derive from a single treatment program and a limited geographic venue, the results might not generalize to other homeless treatment-seeking populations. For example, the homeless population living on the street might exhibit a higher or lower prevalence of gambling than the homeless population of the Moving Ahead Program, because the latter were living in a residential program at the time of admission.
Similarly, since our study participants were people who sought treatment, the attributes of our sample might not represent the homeless population, which included non- treatment seekers. For example, because people who seek treatment in general often experience more psychiatric problems than people who do not seek treatment (30), it is reasonable to expect that homeless people who seek treatment also experience more psychopathology than their counterparts who do not seek treatment. Also, because our sample was drawn from a single treatment program, these findings also might be limited in how accurately the treatment program itself represents treatment seekers from other regions or programs.
Acknowledgments
This project was partly supported by funding from the National Center for Responsible Gaming, the Institute for the Study of Pathological Gambling and Related Disorders at Harvard Medical School, and the St. Francis House Moving Ahead Program. The authors thank Joni Vander Bilt, M.P.H., for her important contributions to this project.
Dr. Shaffer and Mr. Freed are affiliated with the division on addictions of Harvard Medical School, 180 Longwood Avenue, Suite 330, Boston, Massachusetts 02115 (e-mail, [email protected]). Mr. Healea is with the Boston University School of Theology.
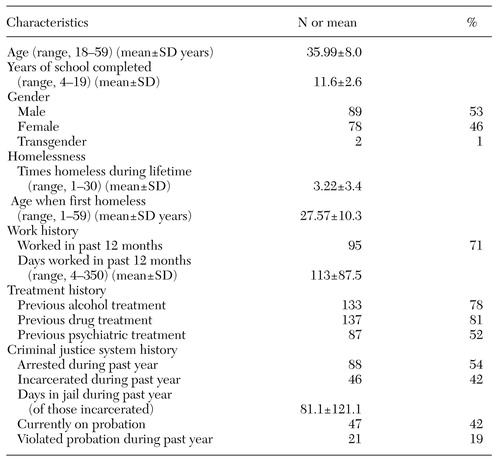 |
Table 1. Demographic and other characteristics of 171 participants in the Moving Ahead Program
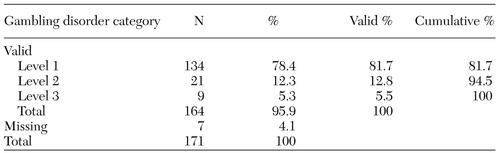 |
Table 2. Past-year prevalence of disordered gambling among 171 participants in the Moving Ahead Program
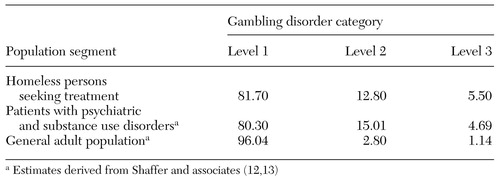 |
Table 3. Past-year prevalence of gambling disorders among population segments (percentages)
1. Lepage C, Ladouceur R, Jacques C: Prevalence of problem gambling among community service users. Community Mental Health Journal 36:597-601, 2000Crossref, Medline, Google Scholar
2. Morris W, Crystal S: Diagnostic patterns in hospital use by an urban homeless population. Western Journal of Medicine 151:472-476, 1989Medline, Google Scholar
3. Burt MR, Cohen BE: Differences among single women, women with children, and single me. Social Problems 36:508-524, 1989Crossref, Google Scholar
4. International Union of Gospel Missions:1998 Gambling and Homelessness Survey. Kansas City, Mo, International Union of Gospel Missions, Association of Gospel Rescue Missions, 1998Google Scholar
5. Langenbucher J, Bavly L, Labouvie E, et al: Clinical features of pathological gambling in an addictions treatment cohort. Psychology of Addictive Behaviors 15:77-79, 2001Crossref, Medline, Google Scholar
6. Lesieur HR, Blume SB: Characteristics of pathological gamblers identified among patients on a psychiatric admissions service. Hospital and Community Psychiatry 41:1009-1012, 1990Abstract, Google Scholar
7. Lesieur HR, Blume SB, Zoppa RM: Alcoholism, drug abuse, and gambling. Alcoholism, Clinical and Experimental Research 10:33-38, 1986Crossref, Medline, Google Scholar
8. Lesieur HR, Heineman M: Pathological gambling among youthful multiple substance abusers in a therapeutic community. British Journal of Addiction 83:765-771, 1988Crossref, Medline, Google Scholar
9. Lesieur HR, Cross J, Frank M, et al: Gambling and pathological gambling among university students. Addictive Behaviors 16:517-527, 1991Crossref, Medline, Google Scholar
10. Lesieur HR, Klein R: Pathological gambling among high school students. Addictive Behaviors 12:129-135, 1987Crossref, Medline, Google Scholar
11. Shaffer HJ, Hall MN: Updating and refining prevalence estimates of disordered gambling behaviour in the United States and Canada. Canadian Journal of Public Health 92:168-172, 2001Crossref, Medline, Google Scholar
12. Shaffer HJ, Hall MN, Vander Bilt J: Estimating the prevalence of disordered gambling behavior in the United States and Canada: a research synthesis. American Journal of Public Health 89:1369-1376, 1999Crossref, Medline, Google Scholar
13. Shaffer HJ, Hall MN, Vander Bilt J: Estimating the Prevalence of Disordered Gambling Behavior in the United States and Canada: A Meta-Analysis. Boston, Presidents and Fellows of Harvard College, 1997Google Scholar
14. National Research Council: Pathological Gambling: A Critical Review. Washington, DC, National Academy Press, 1999Google Scholar
15. Korn D, Shaffer HJ: Gambling and the health of the public: adopting a public health perspective. Journal of Gambling Studies 15:289-365, 1999Crossref, Medline, Google Scholar
16. Sebastian JG: Homelessness: a state of vulnerability. Family and Community Health 8:11-24, 1985Google Scholar
17. Sumerlin JR: Discriminant analyses of willingness to talk with a counselor and most difficult issues in the experience of unsheltered homeless men: self-actualization, loneliness, and depression. Psychological Reports 78:659-672, 1996Crossref, Medline, Google Scholar
18. Adkins CB, Fields J: Health care values of homeless women and their children. Family and Community Health 15:20-29, 1992Crossref, Google Scholar
19. Lopes LL: Between hope and fear: the psychology of risk, in Advances in Experimental Social Psychology, vol 20. Edited by Berkowitz L. San Diego, Calif, Academic Press, 1987Google Scholar
20. Clotfelter CT, Cook PJ: Selling Hope: State Lotteries in America. Cambridge, Mass, Harvard University Press, 1989Google Scholar
21. Shaffer HJ, LaBrie R, Scanlan KM, et al: Pathological gambling among adolescents: Massachusetts Gambling Screen (MAGS). Journal of Gambling Studies 10:339-362, 1994Crossref, Medline, Google Scholar
22. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
23. Norusis MJ, SPSS Inc: SPSS for Windows: Professional Statistics, version 6.0. Chicago, SPSS Inc, 1993Google Scholar
24. Shaffer HJ, Hall MN: Estimating the prevalence of adolescent gambling disorders: a quantitative synthesis and guide toward standard gambling nomenclature. Journal of Gambling Studies 12:193-214, 1996Crossref, Medline, Google Scholar
25. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC, American Psychiatric Association, 1980Google Scholar
26. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, revised. Washington, DC, American Psychiatric Association, 1987Google Scholar
27. Skinner BF: Contingencies of Reinforcement: A Theoretical Analysis. Englewood Cliffs, NJ, Prentice-Hall, 1969Google Scholar
28. Shaffer HJ, LaSalvia TA, Stein JP: Comparing Hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Alternative Therapies in Health and Medicine 3:57-66, 1997Google Scholar
29. Shaffer HJ, Eber GB: Temporal progression of cocaine dependence symptoms in the US National Comorbidity Survey. Addiction 97:543-554, 2002Crossref, Medline, Google Scholar
30. Crockford DN, el-Guebaly N: Psychiatric comorbidity in pathological gambling: a critical review. Canadian Journal of Psychiatry 43:43-50, 1998Crossref, Medline, Google Scholar