Correlates of ADHD Among Children in Pediatric and Psychiatric Clinics
Abstract
OBJECTIVE: Conventional wisdom among pediatricians has been that children with attention-deficit hyperactivity disorder (ADHD) who receive their diagnosis and are managed in the primary care setting have fewer comorbid psychiatric disorders and milder impairments than those seen in psychiatric clinics. The authors sought to determine whether comorbidity and clinical correlates of ADHD differ among children in these two settings. METHODS: A case-control study design was used. Participants were 522 children and adolescents of both sexes, six to 18 years of age, with (N=280) and without (N=242) ADHD. Participants were drawn from pediatric and psychiatric clinics in a tertiary care hospital and a health maintenance organization in a large metropolitan area. Assessments were conducted with standardized measures of psychiatric, cognitive, social, academic, and family function. RESULTS: The number, type, clusters, and age at onset of ADHD symptoms were nearly identical for youths at pediatric and psychiatric ascertainment sources. Regardless of source, participants with ADHD were significantly more likely than controls to have a higher prevalence of mood disorders, other disruptive behavior, anxiety disorders, and substance use disorders. Significant impairments of intellectual, academic, interpersonal, and family functioning did not differ between ascertainment sources. CONCLUSIONS: Children with ADHD from both psychiatric and pediatric practices have prototypical symptoms of the disorder; high levels of comorbidity with mood, anxiety, and disruptive behavior disorders; and impairments in cognitive, interpersonal, and academic function that do not differ by ascertainment source. These findings suggest that children cared for in pediatric practice have similar levels of comorbidity and dysfunction as psychiatrically referred youth.
Attention-deficit hyperactivity disorder (ADHD) is a common childhood disorder that has been estimated to affect 3 to 5 percent of school-age children (1). Recent studies have shown that ADHD is associated with significant impairment in multiple domains of functioning, including a high frequency of psychiatric comorbidity with disruptive mood and anxiety disorders, poor educational attainment, lower IQ, and low occupational performance (2,3,4,5,6,7). ADHD is also associated with maladaptive interpersonal interactions and low self-esteem (8,9,10,11,12).
Although similar findings of comorbidity and dysfunction have been reported in large epidemiological studies of children (13,14,15,16,17,18), some pediatricians have suggested that children with ADHD who receive their diagnosis and are managed in the primary care setting have fewer comorbid psychiatric disorders and milder impairments than those seen in psychiatric clinics (19,20,21). The question of whether such ascertainment bias exists has important clinical, scientific, and public health implications, particularly considering that the majority of children with ADHD are treated by primary care physicians (20).
Among children with ADHD, the presence of comorbid psychiatric disorders predicts both the persistence of ADHD into adulthood and a more complicated course with poorer outcomes (3,7,22,23,24). If pediatric samples of children with ADHD were found to have rates of comorbid psychiatric disorders similar to those seen in psychiatric samples, the implication would be that pediatric patients with ADHD may have an equally high risk of experiencing a complicated course and compromised outcome. To our knowledge, this question has not been adequately examined.
We sought to determine whether comorbidity and other clinical correlates of ADHD would differ among children referred to pediatric and to psychiatric clinics. To this end, we compared rates of comorbidity and degree of dysfunction in a large sample of children with ADHD drawn from pediatric and psychiatric practices. On the basis of current notions in pediatric practice, we predicted that children with ADHD recruited from pediatric practices would have less comorbidity and less dysfunction than those recruited from a child psychiatry clinic.
Methods
Sample
The sample included 522 children and adolescents of both sexes, 6 to 18 years of age, with (N=280) and without (N=242) ADHD. Children were excluded from the study if they had been adopted; if the nuclear family was not available for study; or if they had major sensorimotor handicaps, such as paralysis, deafness, blindness, or psychosis, autism, inadequate command of the English language, or a full-scale IQ below 80. Each of the children with ADHD met DSM-III-R (25) criteria for a diagnosis of ADHD at the time of clinical referral, and at the time of recruitment, they all had active symptoms of the disorder. Written informed consent was obtained from each parent for his or her child, and children and adolescents provided written assent to participate. The study was approved by the institutional review board of Massachusetts General Hospital.
Our psychiatric sample was made up of consecutive referrals during the late 1980s and early 1990s to the pediatric psychopharmacology program at a large urban medical center. The children were referred by parents, pediatricians, and schools for psychiatric evaluation. Participants in the pediatric sample were consecutively recruited from several pediatric sites of a large health maintenance organization, including both inner-city and suburban locations, in the greater Boston area. Children who came for routine physical examination to the urban medical center and the pediatric sites of the health maintenance organization were recruited as control subjects for the psychiatric sample and pediatric sample, respectively. A detailed description of the selection process has been published elsewhere (26,27,28).
A three-stage ascertainment procedure was used in the selection of participants. For participants with ADHD, the first stage was the original referral to a psychiatric or a pediatric clinic that resulted in a diagnosis of ADHD. To minimize bias, since the diagnosis of ADHD was made by different clinicians using different clinical standards, a second systematic screening step was included: a telephone questionnaire consisting of the 14 DSM-III-R symptoms was administered to the mother of each child who had a diagnosis of ADHD. In the final step, eligible subjects who consented to participate in the study received a comprehensive assessment battery, including a structured diagnostic interview. Only those who received a diagnosis of ADHD at all three stages were included in the study.
Control subjects were also screened in three stages. First, patients referred for routine physical examination were recruited at each site. Second, the DSM-III-R telephone questionnaire was administered to the children's mothers. Eligible subjects who consented to participate received the same assessment battery as the ADHD sample. Only those for whom no diagnosis of ADHD was made at any of the three stages were included in the study.
Assessments
Participants were assessed with DSM-III-R structured clinical interviews, which were supplemented, when possible, with questions from the DSM-IV. In cases in which DSM-IV information was not collected, proxies for DSM-IV ADHD subtypes were constructed on the basis of DSM-III-R symptoms (1,25). Psychiatric assessments relied on the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Epidemiologic, version 4 (Kiddie-SADS-E) (29,30); for children 12 years old and under, this instrument was completed with the mother, and for children over 12, directly with the youth.
All assessment personnel were blinded to the participants' diagnosis and ascertainment source. Interviews were conducted by raters with undergraduate degrees in psychology who completed an intensive training program. The training program consisted of familiarization with psychiatric nosology and structured interviews, observation of interviews carried out by experienced raters and clinicians, and then supervised execution of interviews. Kappa coefficients of agreement were calculated between raters and board-certified child and adult psychiatrists listening to audio tapes made by the raters. For 173 interviews, the median kappa was .86, and the kappa was .99 for diagnosis of ADHD.
All diagnostic uncertainties were resolved by a committee of board-certified child and adult psychiatrists, chaired by the principal investigator (JB). The committee members were blind to the participant's initial site of diagnosis, ADHD status, and psychological tests. Psychiatric disorders were diagnosed only if the interview criteria were met unequivocally. The summary variable "two or more anxiety disorders" was used to define clinically meaningful anxiety disorders (31). For children over age 12, data from direct and indirect interviews were combined and considered positive when criteria were endorsed by either parent or child. In addition, a DSM-III-R Global Assessment of Function (GAF) was made. The GAF score summarizes a child's overall function on a scale ranging from 1, worst, to 90, best; it also gives a rating of a child's current function—that is, over the past month—and worst lifetime function (25).
Additional data were collected to assess social and academic functioning. Socioeconomic status (SES) was defined by the Hollingshead-Redlich Scale, which ranges from 1 to 5, with higher numbers corresponding to lower social classes (32). Family intactness was defined as a binary variable—parents married and the family living together, or parents divorced or separated and the family not living together. Family functioning was measured with the Family Environment Scale (FES) (33). The FES has high internal and test-retest reliability and availability of norms. It measures the quality of family relationships along three dimensions: cohesion—the degree of commitment, help, and support family members provide for one another, measured on a scale from 1 to 68; expressiveness—the extent to which family members are encouraged to act and express their feelings openly, on a scale of 15 to 73; and conflict—the amount of openly expressed anger, aggression, and conflict among family members, on a scale of 32 to 81.
Social functioning was evaluated with the Social Adjustment Inventory for Children and Adolescents (SAICA) (34), a semistructured interview schedule that assesses adaptive functioning. It consists of a series of 4-point scales that assess relationships with parents and peers, social activities, and interpersonal problems. Cognitive ability was assessed with the methods described by Sattler (35); full-scale IQ was estimated from the block design and vocabulary subtests of the Wechsler Intelligence Scale for Children-Revised (WISC-R) (36). Scores can range from 80 to 133, with higher scores indicating better performance. The Freedom From Distractibility Index, derived from the digit span, arithmetic, and coding subscales of the WISC-R, was also calculated; scores can range from 50 to 150, with higher scores indicating better performance.
We assessed reading and arithmetic achievement with subtests of the Wide Range Achievement Test-Revised (WRAT-R) and the Gilmore Oral Reading Test (37,38). Scores on the two tests can range from 46 to 155 and from 60 to 140, respectively, with higher scores indicating better performance. The definition of learning disabilities under Public Law 94-142 requires a significant discrepancy between a child's potential and his or her achievement (39). We operationalized this definition with the procedure recommended by Reynolds that we have used elsewhere (40,41). This procedure yields two binary variables indicating the presence of learning disabilities in reading and in arithmetic.
Statistical analysis
Logistic and linear regression were used to evaluate the influence of a diagnosis of ADHD and the ascertainment source—psychiatric or pediatric—on the outcome variables. Each regression analysis modeled the outcome as a function of three predictors: ascertainment source of diagnosis—psychiatric versus pediatric; ADHD status of the participant—ADHD versus control; and the interaction of ADHD status and ascertainment source, which indicates whether the effects of ADHD status on outcome differ by ascertainment source. This approach provides two types of information about potential ascertainment biases. A significant difference between ascertainment sites would suggest that, regardless of the ADHD diagnosis, there were differences in outcome between sites. A significant interaction would mean that the effect of ADHD status on outcome differed between ascertainment sources.
All analyses were two-tailed, and the alpha level was set at .01 to minimize the risk of type I errors due to multiple statistical tests. For certain diagnostic outcomes, insufficient data prevented the fitting of a standard logistic regression model using maximum-likelihood inference. In these cases, we employed an alternative logistic model that uses conditional exact inference as implemented in LogXact (42). This method is designed to accommodate situations when the usual assumptions for likelihood ratio and Wald's tests do not hold because the data are insufficient.
Results
Table 1 summarizes the demographic and clinical characteristics of participants. There were no meaningful interaction effects for age, family intactness, or number of siblings between children with and without ADHD between ascertainment sources. However, because a small but statistically significant interaction for socioeconomic status was identified between pediatric and psychiatric ascertainment sources, this variable was controlled for in all analyses.
ADHD symptom profile
Table 2 presents the distribution of symptoms for the sample. The number of hyperactive, inattentive, and impulsive symptoms were nearly identical among children with ADHD from both ascertainment sources. Although for most individual symptoms we found no significant effects, we found significant interactions between ADHD status and ascertainment source for "loses things" and "interrupts or intrudes." Follow-up tests showed that children with ADHD at both sites had comparable rates of losing things (z=1.7, p=.085) but that the children with ADHD who were referred to a pediatric setting had lower rates of interrupting or intruding than those referred to a psychiatric clinic (z=-2.7, p=.008). Also, as indicated in Table 1, no differences were observed between the two ADHD groups in the distribution of DSM-IV subtype proxies or the age at onset of ADHD.
ADHD and comorbid psychiatric disorders
Children with ADHD from both ascertainment sources were significantly more likely than control subjects to have mood disorders, such as depression and bipolar disorder; other disruptive behavior disorders, such as conduct and oppositional defiant disorder; multiple anxiety disorders; substance use disorders; tic disorders; and enuresis and encopresis.
As Table 3 shows, the comorbid disorders were all equally prevalent among children with ADHD, regardless of ascertainment source. We observed no significant interactions between ADHD status and ascertainment source for any of these outcomes. Identical results were obtained when the total number of psychiatric disorders was summed for each participant and used as an outcome in the interaction model (interaction effect, t=1.19, p=.234; ADHD effect, t=9.89, p<.001; source effect, t=.25, p=.799).
Functioning measures
As Table 4 shows, statistically significant differences were found between children with and without ADHD on measures of intellectual function—full-scale IQ as measured by the WISC-R—and academic achievement—as measured by the reading and math achievement subtests of the WRAT-R. Children with ADHD were more likely than control subjects to have both lifetime and current impairments on the GAF. Children with ADHD were also more likely than control subjects to have significantly less family cohesion and higher levels of family conflict. Children with ADHD and comorbid psychiatric disorders had poorer social functioning overall than children without ADHD. Academic dysfunction was also seen more frequently among children with ADHD, as reflected in higher percentages of tutoring, repeated grades, and special class placement.
We found significant interactions between ADHD status and ascertainment source for full-scale IQ, freedom from distractibility, and the WRAT-R math achievement subtest. The latter two outcomes also showed significant main effects for ascertainment source. Follow-up tests comparing the three outcomes by ascertainment source for children with and without ADHD showed that for those with ADHD, scores for full-scale IQ, freedom from distractibility, and WRAT-R math achievement scores were not significantly different by ascertainment score. However, for children without ADHD, the scores for freedom from distractibility (z=-3.06, p=.002) and WRAT-R math achievement (z=-2.98, p=.003) were significantly lower for children from the psychiatric site.
Discussion
This is the largest case-control study to date of systematically assessed, referred children of both sexes with and without ADHD diagnosed in pediatric and psychiatric practices. Children with ADHD from the two settings had striking similarities in many nonoverlapping domains of functioning, including comorbid psychiatric disorders and measures of interpersonal, cognitive, academic, and family functioning. These similarities are striking, particularly given our comprehensive assessment procedures and methodologically sound sampling strategy (43) and the adequacy of the statistical power our study had to detect clinically meaningful differences. Despite a higher prevalence of two ADHD symptoms among the children with ADHD from the psychiatric setting, these findings challenge the idea that children with ADHD treated in the primary care setting are less impaired and suggest that studies of children with ADHD from psychiatric settings are not compromised by referral bias.
Despite methodological differences, our findings are highly consistent with results reported for community samples (12,13,14,15,16,17,44,45,46,47). For example, community samples in Puerto Rico, New Zealand, Canada, and the United States identified patterns of comorbidity among children with ADHD that are consistent with our findings in a referred sample (12,13,14,15,16,17,44,45,48,49,50). Recent extensive literature reviews (46,47) concluded that co-occurring disorders are common among persons with ADHD. In a study of 8,000 children by Wolraich and colleagues (51), 29 percent of children with ADHD had comorbid anxiety or depression, and 29 percent had comorbid conduct disorder. These findings are consistent with those from our pediatric and psychiatric samples.
Wasserman and associates (21) surveyed pediatric primary care pro-viders on the behavioral problems of 21,000 children seen in primary care practices. In this nonreferred sample, 9.2 percent of the children were identified as having clinically significant inattention or hyperactivity. Of these, about 40 percent had conduct problems and 19 percent showed anxiety or sadness. The similarities between these findings and ours are remarkable considering that only 37 percent of clinicians in the study by Wasserman and associates used standardized questionnaires.
Our results, which show that ADHD is frequently associated with comorbid psychiatric disorders in primary care settings, are difficult to reconcile with the results of other studies (20,21,48,49,50). Yet the implications for primary care clinicians are substantial. Conventional wisdom about the absence of comorbid disorders among children with ADHD may result from the underdiagnosis of behavioral disorders in the primary care setting. The discrepancy between our findings and clinical lore suggests that the identification of ADHD and comorbid disorders in research studies differs from their identification in pediatric practice. Research studies use systematic efforts to elicit information from parents and clinicians (12,13,14,15,16,17,18,48). In clinical practice, primary care practitioners may not routinely collect behavioral information (21,51,52,53,54,55,56,57). Thus a large number of youths with impairing psychiatric disorders are undiagnosed and untreated (52,53,54,55,56,57,58,59). If parents are reluctant to discuss their children's emotional problems with clinicians, and pediatricians have a low index of suspicion for the presence of ADHD and other mental disorders in youths, these conditions may not be identified without the systematic collection of information (21,53,54,55,56).
Since comorbid psychiatric disorders among children with ADHD are associated with a more compromised outcome, and considering that the vast majority of children with ADHD are treated in the primary care setting, our findings call for improved methods of identifying comorbid emotional and behavioral disorders that place some children with ADHD at very high risk of compromised outcomes (4,6,7,8,9,10,58,59). Moreover, since many comorbid conditions can be successfully treated, their identification in pediatric practice is of very high clinical relevance. Undiagnosed and untreated psychiatric disorders impair educational and occupational achievement and psychosocial functioning. Such impairments in turn lead to greater use of health care and government resources (52,58,59).
Our study must be interpreted in light of its methodological limitations. Given that children with ADHD were selected on the basis of DSM-III-R criteria, our findings may not generalize to DSM-IV. However, because more than 90 percent of our sample met criteria for at least one DSM-IV subtype, it is likely that our results can be extrapolated to DSM-IV. Because the sample was largely Caucasian, our results may not generalize to minority groups.
Another threat to generalizability stems from our exclusion of subjects who had been adopted or whose nuclear family was not available. However, the generalizability of our findings is limited only to the extent that the pattern of results reported here would differ if we had selected a sample that included adopted children and children whose nuclear family was not available and the proportion of these children differed across the two referral sources. Given that these children are uncommon relative to the children we studied, the rate of referral of this subgroup would have to differ substantially between the pediatric and psychiatric clinics to threaten the conclusions derived from our findings.
Another potential source of bias arises from the lack of direct interviews with children younger than 12 years of age, which may have resulted in underestimation of the prevalence of some disorders. Also, mothers may have a tendency not to report more than one disorder for their children—referred to as the halo effect (60). These methodological limitations are minimized by the adequate statistical power of our study, the similar numbers of children ascertained in pediatric and psychiatric settings and the adequate gender representation in our sample, and the comprehensive assessment battery we used (51,52,53).
Conclusion
Children with ADHD from psychiatric and pediatric practices show similar levels of ADHD symptoms, comorbidity with mood, anxiety, and disruptive behavior disorders, and impairment in cognitive, interpersonal, and academic function. These findings underscore the importance of the role of pediatricians and primary care providers in recognizing comorbid disorders and dysfunctions among children with ADHD. Physicians who treat children and adolescents with ADHD should be aware that the recognition of comorbid disorders and dysfunctions among these patients and appropriate intervention could have a substantial impact on the future of millions of affected children and their families.
Acknowledgments
This research was supported in part by grants R01-MH-50657-07 and R01-HD36317-02 to Dr. Beiderman from the National Institute of Mental Health.
Dr. Busch is affiliated with the department of pediatrics of the Tufts University School of Medicine in Boston. Her coauthors are affiliated with the pediatric psychopharmacology unit of Massachusetts General Hospital in Boston, except Dr. Zallen, who is with Harvard Pilgrim Health Care in Boston. Dr. Biederman, Dr. Cohen, Dr. Mick, and Dr. Faraone are also with the department of psychiatry at Massachusetts General Hospital. Send correspondence to Dr. Biederman, Pediatric Psychopharmacology Unit, WACC 725, Massachusetts General Hospital, 15 Parkman Street, Boston, Massachusetts 02114 (e-mail, [email protected]). This research was presented in part at the conference "Advancing Children's Health 2000" of the Pediatric Academic Societies and the American Academy of Pediatrics Meeting held May 12-16, 2000, in Boston.
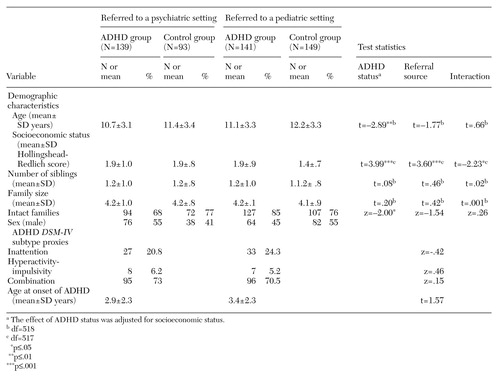 |
Table 1. Demographic and clinical characteristics of a sample of 522 children with and without attention-deficit hyperactivity disorder (ADHD) diagnosed after referral to psychiatric and pediatric settings
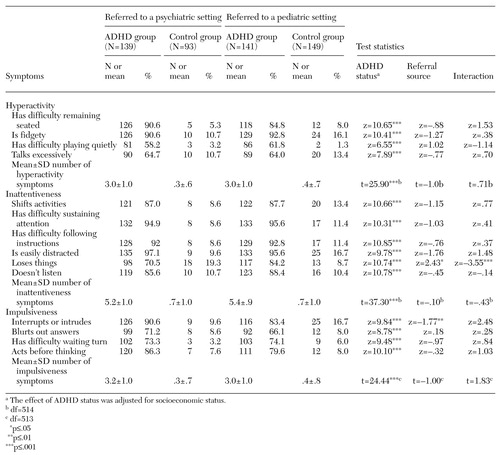 |
Table 2. Symptoms of attention-deficit hyperactivity disorder (ADHD) among 522 children with and without the disorder diagnosed after referral to psychiatric and pediatric settings
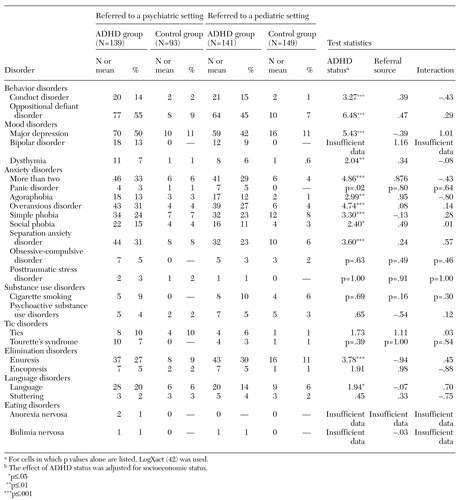 |
Table 3. Lifetime prevalence of psychiatric disorders among 522 children with and without attention-deficit hyperactivity disorder (ADHD) diagnosed after referral to psychiatric and pediatric settings
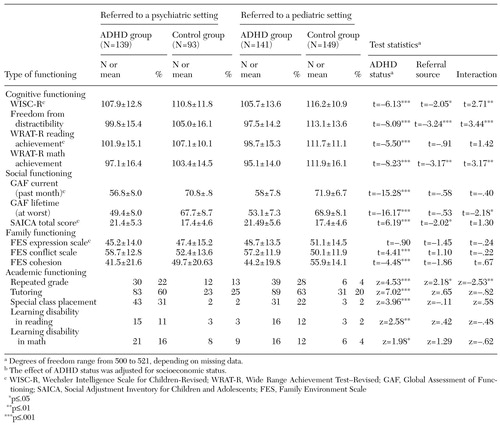 |
Table 4. Measures of functioning among 522 children with and without attention-deficit hyperactivity disorder (ADHD) diagnosed after referral to psychiatric and pediatric settings
1. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
2. Biederman J, Newcorn J, Sprich S: Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. American Journal of Psychiatry 148:564-577, 1991Link, Google Scholar
3. Jensen PS, Martin D, Cantwell DP: Comorbidity in ADHD: implications for research, practice, and DSM-V. Journal of the American Academy of Child and Adolescent Psychiatry 36:1065-1079, 1997Crossref, Medline, Google Scholar
4. Pliszka SR: Comorbidity of attention-deficit/hyperactivity disorder with psychiatric disorder: an overview. Journal of Clinical Psychiatry 59:50-58, 1998Medline, Google Scholar
5. Spencer T, Biederman J, Wilens T: Attention-deficit/hyperactivity disorder and comorbidity. Pediatric Clinics of North America 46:915-927, 1999Crossref, Medline, Google Scholar
6. Faraone SV, Biederman J, Krifcher Lehman B, et al: Intellectual performance and school failure in children with attention deficit hyperactivity disorder and in their siblings. Journal of Abnormal Psychology 102:616-623, 1993Crossref, Medline, Google Scholar
7. Mannuzza S, Klein RG, Bessler A, et al: Educational and occupational outcome of hyperactive boys grown up. Journal of the American Academy of Child and Adolescent Psychiatry 36:1222-1227, 1997Crossref, Medline, Google Scholar
8. Wilson J, Marcotte A: Psychosocial adjustment and educational outcome in adolescents with a childhood diagnosis of attention deficit disorder. Journal of the American Academy of Child and Adolescent Psychiatry 35:579-588, 1996Crossref, Medline, Google Scholar
9. Greene R, Biederman J, Faraone S, et al: Adolescent outcome of boys with attention-deficit/ hyperactivity disorder and social disability: results from a 4-year longitudinal follow-up study. Journal of Consulting and Clinical Psychology 65:758-767, 1997Crossref, Medline, Google Scholar
10. Fischer M, Barkley RA, Fletcher KE, et al: The adolescent outcome of hyperactive children: predictors of psychiatric, academic, social, and emotional adjustment. Journal of the American Academy of Child and Adolescent Psychiatry 32:324-332, 1993Crossref, Medline, Google Scholar
11. Slomkowski C, Klein R, Mannuzza S: Is self-esteem an important outcome in hyperactive children? Journal of Abnormal Child Psychology 23:303-315, 1995Google Scholar
12. Fergusson D, Lynskey M, Horwood J: Attentional difficulties in middle childhood and psychosocial outcomes in young adulthood. Journal of Child Psychology and Psychiatry 38:633-644, 1997Crossref, Medline, Google Scholar
13. Anderson JC, Williams S, McGee R, et al: DSM-III disorders in preadolescent children: prevalence in a large sample from the general population. Archives of General Psychiatry 44:69-76, 1987Crossref, Medline, Google Scholar
14. Szatmari P, Offord DR, Boyle MH: Correlates, associated impairments, and patterns of service utilization of children with attention deficit disorder: findings from the Ontario Child Health Study. Journal of Child Psychology and Psychiatry 30:205-217, 1989Crossref, Medline, Google Scholar
15. Bird HR, Gould MS, Staghezza BM: Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child and Adolescent Psychiatry 32:361-368, 1993Crossref, Medline, Google Scholar
16. Cohen P, Cohen J, Kasen S, et al: An epidemiological study of disorders in late childhood and adolescence: I. age- and gender-specific prevalence. Journal of Child Psychology and Psychiatry 34:851-867, 1993Crossref, Medline, Google Scholar
17. Fergusson D, Horwood L, Lynskey M: Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15-year-olds. Journal of the American Academy of Child and Adolescent Psychiatry 32:1127-1135, 1993Crossref, Medline, Google Scholar
18. Scahill L, Schwab-Stone M, Merikangas KR, et al: Psychosocial and clinical correlates of ADHD in a community sample of school-age children. Journal of the American Academy of Child and Adolescent Psychiatry 38:976-984, 1999Crossref, Medline, Google Scholar
19. Epstein MA, Shawitz SE, Shaywitz BA, et al: The boundries of attention deficit disorder. Journal of Learning Disabilities 24:78-86, 1991Crossref, Medline, Google Scholar
20. Wolraich M: Current assessment and treatment practices: Consensus Development Conference Statement: Diagnosis and Treatment of Attention Deficit Hyperactivity Disorder (ADHD). Bethesda, Md, National Institutes of Health, 1998Google Scholar
21. Wasserman RC, Kelleher KJ, Bocian A, et al: Identification of attentional and hyperactivity problems in primary care: a report from pediatric research in office settings and the ambulatory sentinel practice network. Pediatrics 103:E38, 1999Google Scholar
22. Biederman J, Faraone SV, Milberger S, et al: Predictors of persistence and remission of ADHD: results from a four-year prospective follow-up study of ADHD children. Journal of the American Academy of Child and Adolescent Psychiatry 35:343-351, 1996Crossref, Medline, Google Scholar
23. Angold A, Costello EJ: Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. American Journal of Psychiatry 150:1779-1791, 1993Link, Google Scholar
24. Biederman J, Faraone S, Milberger S, et al: A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Archives of General Psychiatry 53:437-446, 1996Crossref, Medline, Google Scholar
25. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, revised. Washington, DC, American Psychiatric Association, 1987Google Scholar
26. Biederman J, Faraone SV, Keenan K, et al: Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder: patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Archives of General Psychiatry 49:728-738, 1992Crossref, Medline, Google Scholar
27. Seidman L, Biederman J, Faraone S, et al: A pilot study of neuropsychological function in ADHD girls. Journal of the American Academy of Child and Adolescent Psychiatry 36:366-373, 1997Crossref, Medline, Google Scholar
28. Biederman J, Faraone S, Mick E, et al: Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry 38:966-975, 1999Crossref, Medline, Google Scholar
29. Orvaschel H: Psychiatric interviews suitable for use in research with children and adolescents. Psychopharmacology Bulletin 21:737-745, 1985Medline, Google Scholar
30. Spitzer RL, Williams JB, Gibbon M, et al: Structured Clinical Interview for DSM-III-R: Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
31. Biederman J, Rosenbaum JF, Hirshfeld DR, et al: Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Archives of General Psychiatry 47:21-26, 1990Crossref, Medline, Google Scholar
32. Hollingshead AB: Four Factor Index of Social Status. New Haven, Yale University Press, 1975Google Scholar
33. Moos RH, Moos BS: Manual for the Family Environment Scale. Palo Alto, Calif, Consulting Psychologists Press, 1974Google Scholar
34. Orvaschel H, Walsh G: Assessment of Adaptive Functioning in Children: A Review of Existing Measures Suitable for Epidemiologic and Clinical Services Research. Washington, DC, Department of Health and Human Services, National Institute of Mental Health, Division of Biometry and Epidemiology, 1980Google Scholar
35. Sattler JM: Assessment of Children's Intelligence. San Diego, JM Sattler, 1988Google Scholar
36. Wechsler D: Manual for the Wechsler Intelligence Scale for Children-Revised. New York, Psychological Corporation, 1974Google Scholar
37. Gilmore JV, Gilmore EC: Gilmore oral reading test. New York, Harcourt, Brace & World, 1968Google Scholar
38. Jastak JF, Jastak S: The Wide Range Achievement Test-Revised. Wilmington, Del, Jastak Associates, 1985Google Scholar
39. Federal Register: Assistance to States for Education for Handicapped Children: Procedures for Evaluating Specific Learning Disabilities. Bethesda, Md, US Department of Health, Education, and Welfare, 1977Google Scholar
40. Reynolds CR: Critical measurement issues in learning disabilities. Journal of Special Education 18:451-476, 1984Crossref, Google Scholar
41. Faraone S, Biederman J, Krifcher Lehman B, et al: Evidence for the independent familial transmission of attention deficit hyperactivity disorder and learning disabilities: results from a family genetic study. American Journal of Psychiatry 150:891-895, 1993Link, Google Scholar
42. Cytel: LogXact for Windows: Logistic Regression Software Featuring Exact Methods User Manual. Cambridge, Mass, Cytel Software Corporation, 1996Google Scholar
43. Faraone S, Tsuang MT: Methods in Psychiatric Genetics, in Textbook in Psychiatric Epidemiology. Edited by Tohen M,Tsuang MT, Zahner EP. New York, Wiley, 1999Google Scholar
44. Costello J, Angold A, Burns B, et al: The Great Smoky Mountains study of youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry 53:1129-1136, 1996Crossref, Medline, Google Scholar
45. Costello J, Angold A, Burns B, et al: The Great Smoky Mountains study of youth: functional impairment and serious emotional disturbance. Archives of General Psychiatry 53:1137-1143, 1996Crossref, Medline, Google Scholar
46. Brown RT, Freeman WS, Perrin JM, et al: Prevalence and assessment of attention-deficit/hyperactivity disorder in primary care settings. Pediatrics 107:E43, 2001Google Scholar
47. Green M, Wong M, Atkins D, et al: Diagnosis of Attention Deficit/Hyperactivity Disorder. Technical Review No 3. Rock-ville, Md, Agency for Health Care Policy and Research, 1999Google Scholar
48. McConaughy S, Achenbach T: Comorbidity of empirically based syndromes in matched general population and clinical samples. Journal of Child Psychology and Psychiatry 35:1141-1157, 1994Crossref, Medline, Google Scholar
49. Angold A, Costello J, Erkanli A: Comorbidity. Journal of Child Psychology and Psychiatry 40:57-87, 1999Crossref, Medline, Google Scholar
50. Goodman SH, Lahey BB, Fielding B, et al: Representativeness of clinical samples of youths with mental disorders: a preliminary population-based study. Journal of Abnormal Psychology 106:3-14, 1997Crossref, Medline, Google Scholar
51. Wolraich M, Hannah J, Pinnock T, et al: Comparison of diagnostic criteria for attention-deficit hyperactivity disorder in a county-wide sample. Journal of the American Academy of Child and Adolescent Psychiatry 35:319-324, 1996Crossref, Medline, Google Scholar
52. Kessler R, McGonagle K, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
53. Lavigne JV, Binns HJ, Christoffel KK, et al: Behavioral and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians' recognition. Pediatric Practice Research Group. Pediatrics 91:649-655, 1993Medline, Google Scholar
54. Kelleher KJ, Childs GE, Wasserman RC, et al: Insurance status and recognition of psychosocial problems: a report from the Pediatric Research in Office Settings and the Ambulatory Sentinel Practice Networks. Archives of Pediatric and Adolescent Medicine 151:1109-1115, 1997Crossref, Medline, Google Scholar
55. Horwitz SM, Leaf PJ, Leventhal JM, et al: Identification and management of psychosocial and developmental problems in community-based, primary care pediatric practices. Pediatrics 89:480-485, 1992Medline, Google Scholar
56. Horwitz SM, Leaf PJ, Leventhal JM: Identification of psychosocial problems in pediatric primary care: do family attitudes make a difference? Archives of Pediatric and Adolescent Medicine 152:367-371, 1998Google Scholar
57. Copeland L, Wolraich M, Lindgren S, et al: Pediatricians' reported practices in the assessment and treatment of attention deficit disorders. Journal of Developmental and Behavioral Pediatrics 8:191-197, 1987Crossref, Medline, Google Scholar
58. Angold A, Costello J, Farmer E, et al: Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry 38:129-137, 1999Crossref, Medline, Google Scholar
59. Costello J, Angold A, Keeler G: Adolescent outcomes of childhood disorders: the consequences of severity and impairment. Journal of the American Academy of Child and Adolescent Psychiatry 38:121-128, 1999Crossref, Medline, Google Scholar
60. Achenbach TM, McConaughy SH, and Howell CT: Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin 101:213-232, 1987Crossref, Medline, Google Scholar