Datapoints: Use of Mood Stabilizers Among Patients With Schizophrenia, 1994-2001
A previous study on the use of mood stabilizers and anticonvulsants among all patients with schizophrenia hospitalized in psychiatric centers operated by the New York State Office of Mental Health found an increase in use between 1994 and 1998 (1). Data were obtained retrospectively by querying a centralized database containing pharmacy prescription information. In the study reported here all inpatients with a DSM-IV diagnosis of schizophrenia who received at least one dose of any mood stabilizer during each calendar year from 1994 to 2001 were identified. Patients with schizoaffective disorder were not included.
Use of these agents has increased (Figure 1). In 1994, 2,201 of 8,405 inpatients diagnosed as having schizophrenia (26.2 percent) received a mood stabilizer, with lithium the most commonly prescribed (1,109 patients, or 13.2 percent). In 2001, 1,950 of 4,139 (47.1 percent) received a mood stabilizer, with valproate the most commonly prescribed (1,445 patients, or 34.9 percent). In comparison, among patients hospitalized in 2001 with any diagnosis, 5,641 of 9,551 (59.1 percent) received a mood stabilizer.
Some trends emerged between 1994 and 2001: use of valproate reached a plateau of 35 percent; lithium utilization decreased steadily, albeit at a slow rate; and use of carbamazepine decreased at a more rapid rate. Newer anticonvulsants were introduced. Gabapentin use peaked in 2000 and exceeded lithium use. Use of topiramate and oxcarbazepine now exceeds that of carbamazepine.
Although the Expert Consensus Guidelines for the Treatment of Schizophrenia (2) recommend the use of lithium and anticonvulsants as adjunctive agents, little empirical evidence supports this recommendation.
The data presented here are representative of a large state hospital system and may not be generalizable to other practice settings. Further issues related to interpreting these data are discussed elsewhere (1). Whether prescribing these agents for patients with schizophrenia is good or bad is impossible to answer without outcome data. Research is lagging behind clinical practice. The results reported here indicate an urgent need for controlled clinical trials to test the efficacy of the adjunctive use of mood stabilizers and anticonvulsants for patients with schizophrenia.
Acknowledgments
Partial support for the maintenance of the integrated research database is currently provided by a grant from Eli Lilly and Co. and in past years was provided by Eli Lilly and Co., the Janssen Research Foundation, and Pfizer, Inc.
The authors are affiliated with the Nathan S. Kline Institute for Psychiatric Research, 140 Old Orangeburg Road Orangeburg, New York 10962 (e-mail, [email protected]). Harold A. Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
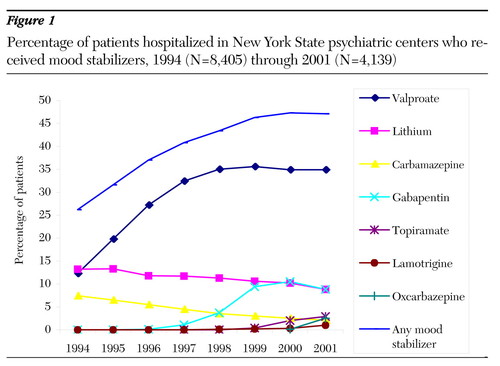
Figure 1. Percentage of patients hospitalized in New York State psychiatric centers who received mood stabilizers, 1994 (N=8,405) through 2001 (N=4,139)
1. Citrome L, Levine J, Allingham B: Changes in use of valproate and other mood stabilizers for patients with schizophrenia from 1994 to 1998. Psychiatric Services 51:634-638, 2000Link, Google Scholar
2. McEvoy JP, Scheifler PL, Frances A: The Expert Consensus Guideline Series, Treatment of Schizophrenia. Journal of Clinical Psychiatry 60(suppl 11):43, 1999Google Scholar



