Public Opinion and the Mental Health Parity Debate: Lessons From the Survey Literature
Abstract
Research on public opinion has seldom been incorporated into the debate about appropriate coverage of mental health and substance abuse treatment services in health insurance plans. However, several surveys have been conducted to probe for voters' awareness of and attitudes toward persons with mental illness and insurance coverage of their treatment needs. Given the current debate over mandating parity for coverage of mental health and substance abuse treatment services, these data promise to be particularly useful to politicians and health policy analysts. The author reviews reports of survey research conducted between 1989 and 1994 to assess American voters' support for expansions of mental health and substance abuse treatment coverage, including their knowledge about the origins and implications of mental illness and their willingness to pay for more generous benefits. The results suggest widespread support for such benefit expansions, but voters express concern about potential increases in their taxes or in their health insurance premiums. To facilitate the passage of meaningful reforms for mental health and substance abuse treatment benefits, policy makers must present realistic estimates of the costs of such expansions and of the benefits to be delivered to those in need.
Research on public opinion was both conducted and applied throughout the debate on the Clinton administration's health care reform proposal in 1993-1994. However, findings from this research have seldom been incorporated into more targeted reform efforts such as the expansion of mental health and substance abuse treatment benefits. The recently passed Mental Health Parity Act of 1996 and several state-level efforts to achieve improvements in the quality and scope of mental health and substance abuse treatment benefits constitute promising policy developments. However, substantial inequities in coverage of these services remain. Thus the expansion of these benefits will likely continue to figure prominently on the health policy agenda in the near future.
Given the public stigmatization of mental illness, state and federal politicians' efforts to contain the rising costs of care, and employers' concerns about the potential abuse of generous mental health and substance abuse treatment benefits, assessing voters' attitudes will be particularly critical to the success of future proposals for reform. Although a substantial literature addresses public attitudes toward persons with mental illness and the prospect of expanding their benefits, the data gathered thus far have not figured prominently in the policy debate itself. Integrating these results into the public dialogue will be particularly helpful inasmuch as they clearly reflect the level of public support for expansion of benefits and voters' familiarity with the economic arguments for and against such reforms.
Four major messages have emerged from the literature reporting the findings of public opinion surveys. First, the public, although not thoroughly familiar with the causes and implications of mental health problems, generally supports attending to the health care needs of populations affected by mental illness, particularly by severe mental illness. Second, this support does not appear to extend to those with health care needs related to substance abuse. Third, despite a generally sympathetic attitude, the public is wary of the costs that might be incurred if mental health and substance abuse treatment benefits were expanded. And fourth, the public is therefore sensitive to the specific benefits that would be affected and the mechanisms by which overall expenditures would be controlled.
In sum, although survey respondents are willing to endorse more generous benefits for treatment of mental illness, they are unlikely to support proposals that would fold mental health and substance abuse treatment benefits into standard physical health benefits packages altogether.
Typical limits on mental health and substance abuse coverage are much more stringent than those imposed on coverage of somatic illnesses. As of 1993, only 14 percent of insured employees of medium-size and large firms had mental health coverage that was comparable to their general health benefits packages; this share reflected a marked decrease from 1988, when 27 percent of such employees had equal coverage (1,2). This difference also exists in the public sector, where Medicaid and Medicare are significantly more restrictive with their coverage of mental health and substance abuse services than of physical health services. Disparities in benefits generally consist of fewer covered inpatient days or outpatient visits, higher cost-sharing requirements, a higher ceiling on out-of-pocket expenditures, or the lack of limits on out-of-pocket costs.
In the past, improving coverage for mental health and substance abuse treatment services has proved a particular challenge due to the unique nature of mental illness and the health care needs of those affected by it. Some have cited the perceived ambiguity of certain mental health and substance abuse diagnoses and the questionable efficacy of treatments as cause for stricter limits on coverage. Such perspectives continue to be voiced today, as the push for parity dominates the political debate over the future of mental health and substance abuse benefits.
Although parity has been loosely defined as the expansion of mental health and substance abuse treatment benefits to the standard level of coverage for physical health benefits, the term may be used and construed in a number of ways. For instance, proposals to reduce enrollees' cost-sharing burden or simply to expand annual or overall limits on utilization and spending are also being considered. How parity is ultimately defined will clearly have a direct impact on the extent to which reform will result in meaningful improvements. The somewhat casual current use of the term further justifies examination of precisely which reforms the public is willing to support. The strategic political packaging of such controversial proposals will be critical to their legislative success.
The range of arguments in favor of expanding or equalizing coverage spans the perspectives and priorities of the parties involved. Advocates and mental health professionals, for instance, argue on the grounds of general fairness, pointing out that mental illness is often as debilitating as physical illness and thus that current limits on mental health and substance abuse coverage should be relaxed or removed altogether.
Economists, on the other hand, come down on both sides of the debate. Some argue that the market is not serving the mental health community well, with adverse selection limiting access to those with the most severe and therefore most expensive mental health care needs. Others raise concerns about moral hazard, citing evidence about heightened demand in response to generous mental health and substance abuse treatment benefits (3). To employers and others who fear spiraling costs of care, many proponents of expanded benefits offer the "medical offset" argument. This argument holds that potential increases in mental health costs will be offset at least partly by reduced medical costs because fewer general health services will be provided to patients who were previously unable to obtain mental health treatment because of more stringent limits on coverage.
As in recent attempts to reform the general health care system, the political fate of legislation addressing parity of mental health and substance abuse treatment benefits will be determined as much by the appeal of these arguments as by the strength of the public's endorsement. In this light, survey research may serve as an effective tool for understanding voters' attitudes toward mental illness and assessing the prospects of expanding coverage for treatment services. This paper reviews reports of survey research in this area conducted between 1989 and 1994, discusses the results that have been gathered thus far, and proposes strategies for incorporating public opinion data into the debate about parity.
Methodological issues
To date, the relevant public opinion literature spans a range of issues addressing public perceptions of persons with mental illness and attitudes toward paying for their treatment. Given that the research presented below has been drawn from multiple sources with diverse policy goals, isolating a clear set of indicators of public support for mental health benefits remains a substantial challenge. Analyses of the type presented below, which attempt to synthesize the results of multiple studies, are further complicated by variation in survey design. Subtle differences in wording of questions or in sampling methods often have an impact on survey research results. However, assessing the precise effects of such variation is especially critical in studies of beliefs that are likely shaped by social stereotypes and stigmatization. Needless to say, attitudes toward mental illness fall within this category.
In surveys designed to assess public attitudes toward persons with mental illness, the impact of question wording is not so much a problem to be overcome as it is an issue worth special consideration in itself. Indeed, awareness of the public's sensitivities to terminology will be critical to the task of devising effective strategies for designing and "selling" various proposals for reform of mental health treatment benefits.
Several of the surveys discussed below address this issue through the use of split samples. This technique allows measurement of the effect of small changes in question wording by comparing responses to alternative versions of questions across subsamples within the overall sample. This technique is particularly useful for determining which terms are likely to engender the most sympathy among the public, as well as for identifying the specific policy components that voters will be most amenable to supporting.
Another methodological issue is the use of closed- versus open-ended questions in public opinion surveys. This distinction refers to whether participants are required to respond to the survey items by selecting from a list of response options or whether they must provide their own original responses.
In large-scale, nationwide surveys such as those detailed below, response options are typically provided to facilitate coding and the collection of statistically meaningful results. Not surprisingly, however, this technique has potential pitfalls because those who design the surveys—and thus decide which response options to offer—have a direct and significant impact on how respondents interpret and respond to the survey items. In policy-oriented surveys, this approach can be especially problematic because respondents are often not familiar with the subject matter and are thus highly suggestible as to what their responses "should be."
Similarly, there is cause for skepticism when interpreting responses to items that ask respondents to rank their preferences according to a list of alternatives provided. Although this design helps standardize responses, it essentially precludes the possibility of alternative responses provided independently by the respondents. Thus to varying degrees, the results are likely to be artifacts of the survey design. Numerous additional issues in design of public opinion surveys could be examined, but further technical discussion is beyond the scope of this paper. The data that follow should be considered with both an awareness of the concerns outlined above and an appreciation for the complexities of conducting meaningful and informative public opinion research.
Public opinion findings
A surprisingly broad range of research on public attitudes toward mental illness has been conducted. To lend structure to the discussion below, the data are classified into the following three categories: what Americans know about the etiology, prevalence, and implications of mental illness and substance abuse conditions; what Americans know about current policies toward mental health and substance abuse treatment benefits and the ongoing debate over expanding these benefits; and the overall level of public support for various types of benefit expansions, with an emphasis on how this support varies according to the services and special populations that would be affected.
Although data in all three categories are important in the broad context of the debate, the discussion that follows focuses on the third category. It is preceded by a brief review of the data from the first two categories, the public's knowledge about mental health and substance abuse conditions and its knowledge about treatment coverage.
Knowledge about mental health conditions and treatment coverage
Respondents' answers to survey items about knowledge of mental health and substance abuse conditions reflect the extent to which common misperceptions and stereotypes about mental illness detract from the public's willingness to support legislation expanding treatment coverage. A substantial portion of the data in this category was gathered as part of a nationwide study sponsored by the Robert Wood Johnson (RWJ) Foundation Program on Chronic Mental Illness (4). This study included a telephone survey in which 1,300 randomly selected adults were interviewed about their attitudes toward persons with chronic mental illness.
One-quarter of the respondents described themselves as very well informed about mental illness, yet added that they should know a great deal more about it. This proportion was quite small relative to those claiming to be very well informed about other illnesses mentioned in the survey, including alcoholism (47 percent), cancer (43 percent), drug abuse (35 percent), heart disease (37 percent), and AIDS (30 percent). Perhaps more important was the finding that, regardless of their current knowledge base, 60 percent of the sample responded that they should know more about mental illness.
When respondents were asked to name the chief cause of mental illness, a plurality cited either a chemical imbalance (27 percent) or the stress of daily life (27 percent). Twenty percent of the sample named alcohol and drug abuse, and 13 percent cited "inherited genes." Regardless of respondents' perceptions about the causes of mental illness, nearly nine of ten respondents (89 percent) described mental illness as a serious problem in society.
Clearly, one of the chief purposes of survey research should be to identify gaps in public knowledge and assist in developing appropriate means of filling them. Survey items that probe for respondents' primary sources of information about mental illness are thus particularly important because they may help target educational messages about mental illness to the public at large. In the RWJ survey, mass media were identified as a source of knowledge about mental illness, with 87 percent of respondents citing television news and programs, 76 percent citing newspapers, 74 percent citing magazines, and 73 percent citing radio news and programs. Non-media-related sources of information were less frequently acknowledged, with family and friends mentioned by 51 percent of the sample population, mental health professionals by 31 percent, and doctors by only 29 percent.
The large portion of the public receiving information from the media is especially problematic given that only 34 percent of the surveyed sample rated television, radio, and newspaper stories as very believable or extremely believable in their coverage of mental health issues. Sixty-one percent described such media as somewhat believable in their coverage of mental illness.
The second type of survey data—on Americans' knowledge about policies toward mental health and substance abuse treatment benefits and about the debate on expanding these benefits—addresses the concern that the conceptual isolation of mental health and substance abuse treatment services from physical health care has resulted in a lack of public interest in the current mechanisms for insuring persons with mental illness. This suspicion is supported by the fact that questions that probe for respondents' awareness of current policies addressing mental health treatment are relatively underrepresented in general health care surveys.
However, some data that reflect voters' interest in the ongoing debate over expanding coverage do exist. For instance, in a 1993 telephone survey sponsored by the Harvard School of Public Health and the Henry J. Kaiser Family Foundation and conducted by Princeton Survey Research Associates, respondents were asked about the degree to which they were familiar with various health care reform proposals (5). When asked if they knew whether mental health coverage was included in congressional Republicans' various legislative proposals, 31 percent responded that such a benefit was included, 20 percent that it was not, and 49 percent that they understood the Republican proposals not too well or not at all or that they did not know the answer to the question. These data do not show whether respondents' lack of familiarity with the proposals' mental health components differs from their level of knowledge about the proposals' other components—for example, whether they included pharmacy or dental benefits. However, the data do provide some context for responses to other, more detailed mental health survey items.
A separate item on the same survey revealed a greater level of familiarity with the Clinton administration's proposal. Only 30 percent of the respondents claimed that they were not at all or not too familiar with the Clinton plan or that they did not know the answer to the question. Of the remaining 70 percent of respondents, 58 percent answered accurately that the President's plan did include mental health coverage, while 12 percent replied that the plan did not.
Public support for expanded benefits
As noted, this discussion organizes the survey data such that the data from the first two categories inform the results from the third, which covers respondents' support for specific mental health and substance abuse benefit reforms. This progression makes sense insofar as a direct relationship exists between respondents' familiarity with mental illness and the relevant policy debate and their base of support for expanding mental health and substance abuse treatment benefits.
Regardless of whether such a link exists, the survey items that address the details of potential policies for treatment benefits bear most directly on the political debate over parity for these services. These surveys include questions designed to assess the public's impressions of a range of proposals for future reform, including whether and how mental illness should be considered distinct from physical illness, whether the two should be programmatically integrated into a single system of coverage, and whether and how much respondents would be willing to pay toward that end. The findings from these survey items are most useful for the parity debate because they reflect the public's concerns about improving and equalizing coverage of mental health and substance abuse benefits and thus indicate the extent of political risk for state and federal legislators who endorse such reforms.
Survey items that assess the appeal of parity for mental health benefits are certainly well represented in the literature (6,7,8,9,10,11). As the data presented in Table 1 imply, a substantial share of objective support for mental health and substance abuse treatment benefits is evident across surveys. However, some evidence suggests that this support is relatively soft in that it deteriorates rapidly if the potential for personal financial sacrifice is acknowledged. For instance, support for a guaranteed mental health benefit dropped from 69 percent of respondents to 34 percent when the survey questions indicated that higher taxes or premiums would be involved (11).
Not surprisingly, when respondents were asked to prioritize the benefits that are most important to them, support for mental health and substance abuse treatment benefits dropped off rapidly as well. For instance, in two separate questions on a Gallup survey, respondents were asked to consider which of five benefits they felt to be the most important and the second most important to guarantee as part of a federal health care reform bill (7). Mental health and substance abuse services did not fare very well on either question, with 8 percent of respondents identifying them as the most important and 15 percent as second most important. One could argue that these benefits were not considered important because only a small proportion of respondents perceived themselves as likely to need them. However, dental care received even less support in the survey, suggesting that the perceived importance of a given service was not necessarily correlated with the likelihood of using it.
A similar question was raised in a 1994 NBC News telephone survey conducted by Blum and Weprin Associates (12). Respondents were presented with a list of benefits and asked to name the one that they most wanted covered by a new health plan, in addition to the costs of physician care and hospital stays. This item in effect asked respondents to identify their third most important benefit. Once again, mental health care did not fare so well; only 3 percent of respondents selected it. In contrast, long-term care was favored by 46 percent of respondents, most of whom were unlikely to be insured for these services; preventive care by 27 percent; and prescription drugs by 19 percent. The remaining 6 percent responded that they were not sure. This distribution of responses may be partly a function of the responses that were offered by the list, particularly because an "other" option was not included.
Using a slightly different approach to question wording, the Los Angeles Times conducted a nationwide telephone survey that asked about the services respondents would be most willing to give up in a health care reform plan (13). This item in effect addressed voters' lowest health care priorities. Mental health coverage received the second largest share (28 percent) of responses. Surprisingly, choice of doctor was the one benefit that a larger number of respondents were willing to do without, with a 40 percent share expressing their willingness to sacrifice this benefit.
As suggested above, one of the likely barriers to consistently strong and widespread support of mental health care coverage is that relatively few people use mental health and substance abuse services—approximately 5 to 10 percent of the privately insured population. Some respondents presumably fear they will be paying for services they will not be using and that they will thus be subsidizing the care of others.
In summary, voters may be less likely to support reform if they do not know how it will affect them personally—for example, how much it will cost them and how they themselves will benefit. These results clearly demonstrate the political importance of devising reliable cost estimates of various policy options for mental health and substance abuse treatment benefits.
Lessons for the policy debate
Reviewing the data on public opinion about mental health and substance abuse treatment benefits is useful because these data reflect voters' views on the future coverage of these services. However, applying the results directly to the policy debate remains a larger challenge. To this end, survey items that address the appeal of very specific options for reform will be necessary, both for assessing the types of expansions that the public is willing to support and for packaging the plan strategically for political purposes. The RWJ survey (4) and a telephone survey of 800 voters that was conducted by Mellman-Lazarus-Lake, Inc. (10) include a wealth of practical data on the way parity should be defined, the specific benefit expansions to be offered, and the speed with which such changes should be implemented.
Services covered
Given that the potential impact on future costs of across-the-board expansion of mental health and substance abuse treatment benefits is still unclear, one of the chief policy objectives should be to identify the services that merit most urgent reform. For example, through the use of split samples, the Mellman-Lazarus-Lake survey sought data on one of the more divisive issues in the current debate—whether substance abuse services should be included in benefit expansions for mental health services (10). As the data in Table 2 illustrate, responses varied dramatically across relatively similar survey items, demonstrating the importance of question wording and survey design.
Respondents were on average essentially indifferent to the idea of including substance abuse services in plans for general health benefit reforms; 31 percent were more likely and another 31 percent were less likely to support such coverage. However, the differential was quite dramatic among the sample who were asked about inclusion of mental health services in benefit reform plans; 39 percent supported such coverage, and 16 percent did not.
Another set of items from the same survey illustrated how indifference to the inclusion of substance abuse benefits disappears when the survey question is designed somewhat differently. Responses to a round of questions asked of four split samples suggested that the public was quite sensitive to the manner in which the specific services to be included in the basic health insurance package under national health care reform were presented. When asked about their support for the inclusion of different benefits, only 16 percent strongly favored "substance abuse coverage," compared with 29 percent who favored "mental health care coverage," 24 percent who favored "coverage for mental illness," and 26 percent who favored "coverage for mental disabilities."
This distinction was even more dramatic when the strength of opposition was examined. For example, 20 percent of respondents voiced strong opposition to the inclusion of a substance abuse benefit, and 42 percent either opposed or strongly opposed such a benefit. In contrast, the shares of strong opposition to "mental health care coverage" (6 percent), "coverage for mental illness" (7 percent), and "coverage for mental disabilities" (6 percent) were much smaller.
The same split samples were asked a separate but similar item on how important it was that the benefit be included in a basic benefits package. In response, 27 percent suggested that substance abuse coverage was not at all important, compared with the much smaller shares of respondents who expressed a lack of support for "mental health care coverage" (7 percent), "coverage of mental illness" (8 percent), and "coverage for mental disabilities" (9 percent).
In another split-sample item from the survey, respondents were asked to rate the importance of covering mental health and substance abuse problems to the same extent as physical health problems. This question directly addressed the level of support for a parity-type benefit. Once again, there were significant differences in support for the prospect of coverage of mental health versus substance abuse problems. Seventy-eight percent of respondents indicated that coverage for mental health problems is more important than (10 percent) or just as important as (68 percent) coverage for physical health problems. Fifty-four percent of respondents expressed the corresponding levels of support for coverage of substance abuse problems; 7 percent thought it was more important than coverage of physical health problems, and 47 percent thought it was just as important. Although 41 percent of the split sample responded that covering services for substance abuse problems was not as important as covering services for physical health problems, only 19 percent expressed that attitude toward coverage of mental health services.
In addition to assessing the public's views about different types of benefit packages, the Mellman-Lazarus-Lake survey explored the manner in which public opinion varies across types of mental illness, once again using split-sample questions (10). Responses to these items confirmed the aforementioned skepticism toward including benefits for substance abuse treatment.
For instance, in response to a question about the importance of covering services for individuals with particular diagnoses, 85 percent indicated that covering services for a "child with a mental health problem" was either one of the most important things to cover or very important, 66 percent assigned that level of importance to services to "someone with a mental disability," 55 percent to "someone with schizophrenia," and 52 percent to "someone with manic depression." The categories given the lowest ratings were services for "someone addicted to drugs" and for "someone addicted to alcohol," each of which was considered most important or very important by 41 percent of respondents.
Financing, phase-ins, and limits on coverage
Even though survey respondents may be willing to support the expansion of mental health and substance abuse treatment benefits in principle, survey results suggest they are anxious about what expanded benefits will cost them in higher premiums or taxes. Survey items that address the financial and structural details of reform are designed to explore the roots of these concerns. For instance, the Mellman-Lazarus-Lake survey probed for respondents' reactions to the idea of a 50 percent copayment (10). Although 31 percent of respondents claimed that they either favored (26 percent) or strongly favored (5 percent) this level of cost sharing, a substantially larger share (58 percent) was either opposed (40 percent) or strongly opposed (18 percent) to the idea. However, these respondents were not asked whether they felt the 50 percent copayment was too high or too low.
As for speed of implementation, the key question is whether new benefits should be phased in gradually or implemented immediately. The idea of a phase-in addresses fears about the rise in costs of care that may accompany expansions in mental health and substance abuse treatment benefits. The results of the Mellman-Lazarus-Lake survey suggest that the public is mildly in favor of the gradual approach, with 48 percent of the respondents either strongly favoring (6 percent) or favoring (42 percent) a phase-in, and 41 percent either opposed (31 percent) or strongly opposed (10 percent) to the idea. When respondents were asked about the possibility of unlimited children's benefits, however, the idea of immediate implementation proved overwhelmingly popular. The proposal to implement full coverage for children under 18 without any phase-in or limits but to maintain a more gradual and limited approach to covering adults was favored by 62 percent of the overall sample. Items that address implementation issues are particularly useful as indicators of the degree to which people are skeptical of dramatic, large-scale changes within a cost-conscious system. These findings highlight the need for further public opinion research about the benefits to be included in specific models for reform of coverage for mental health and substance abuse treatment.
Survey items about benefit design are particularly useful if they present the proposed changes as occurring within the current managed care environment. For instance, a large share of the public supports reviewing the appropriateness of treatment as an alternative to imposing limits on treatment days, with 75 percent of respondents claiming that they either favor or strongly favor the imposition of such utilization review techniques (10).
Nevertheless, the public seems slightly less averse to the idea of imposing annual limits on outpatient days than it is to applying similar limits on hospital coverage. This distinction suggests an underlying level of support for coverage of catastrophic mental health care needs and a degree of concern about moral hazard and higher utilization of outpatient services. Although 53 percent of respondents were opposed or strongly opposed to limiting coverage of outpatient mental health care services to 30 days, 63 percent expressed the same degree of resistance to the prospect of a 30-day limit on hospital care (10). Respondents were slightly less opposed to placing limits on both inpatient and outpatient treatment for substance abuse services, with 48 percent opposing limits on outpatient services and 50 percent opposing limits on inpatient services.
Most voters are aware that reform of mental health and substance abuse treatment benefits may bring higher out-of-pocket costs. Survey research in this area can explore the types of expenditure increases to which voters would be most and least averse. For instance, assessing whether voters respond more positively or less negatively to the idea of a percentage increase versus a flat dollar amount may help policy makers ascertain the specific concerns associated with health benefit expansions in general.
Once again using split samples, the Mellman-Lazarus-Lake survey asked respondents whether they would be willing to cover full mental health benefits if the change cost the individual $100 more per year versus a 5 percent increase in annual costs. Among the group told that unlimited coverage would increase respondents' costs by $100 per year, 60 percent were at least in favor of the expansion. The increase of 5 percent per person per year garnered the support of 54 percent of the respondents. Although these results imply that respondents are slightly more willing to support such expansions if they are presented with the actual dollar amount by which their premiums will increase, these results do not appear strong enough to warrant any definitive conclusions.
Many public opinion data are equivocal about respondents' level of support for mandating expansions of mental health and substance abuse treatment coverage. However, this uncertainty is likely due largely to variations in the wording of survey questions and other survey design effects. Regardless of the extent to which the survey literature is incorporated into the policy debate, however, the successful reconciliation of these numbers may offer a valuable lesson about how various proposals for reform may be packaged most effectively.
Looking ahead
The data gathered thus far in survey research on reform of mental health and substance abuse treatment benefits suggest that the voting public is amenable to the idea of improving health care coverage for persons with mental illness, provided such reforms impose some constraints on the types of benefits involved and the costs to be incurred. Key findings include the fact that respondents support the need for limits on outpatient visits, but that they are more protective of inpatient care—presumably reflecting concern about persons who have catastrophic mental health care needs.
Similarly, the strength of public support does not necessarily extend to benefit expansions for substance abuse treatment services, which may be perceived as serving persons whose conditions have resulted from their own behavioral choices. As for the mechanisms that will be used to control future increases in health care expenditures, survey participants respond more favorably to the utilization of managed care techniques than to the continued use of strict limits on benefits.
Synthesizing the public opinion research findings will be critically relevant to the debate about mental health benefit expansions because of the unique clinical and societal aspects of mental illness and the system that currently serves the treatment needs of those affected by it. The current mental health system is characterized by unusual institutional and organizational features, such as federal, state, and local governments' joint responsibility for financial and administrative oversight of the system. From a political perspective, it will be important to assess public perceptions of the current system of coverage and treatment for persons with mental illness and to determine how well these perceptions coincide with the public's ideas about how the system should be run.
Several empirical studies on expanding mental health care coverage in an environment dominated by managed care are in progress. However, these studies have not yet produced conclusive results about the likely impact of parity on utilization and expenditures. Realistically, successful passage of legislation that mandates more generous mental health and substance abuse treatment benefits will hinge on some degree of certainty that such changes will not produce large increases in overall costs of care. Regardless of the research outcomes, however, politicians will not be eager to endorse significant reforms unless their constituents view them favorably. Public opinion research is a necessary tool for gauging where the public stands today and illustrating what needs to be done to minimize the political costs of backing fair and effective coverage for persons affected by mental illness.
Acknowledgments
This research was supported by a National Institute of Mental Health training grant. The author thanks Karen Donelan and Chris Koyanagi for their assistance in the preparation of this paper and Bob Blendon and Richard Frank for their helpful comments.
Ms. Hanson is a doctoral candidate in the health policy program in the Graduate School of Arts and Sciences at Harvard University, 180 Longwood Avenue, Boston, Massachusetts 02115. This paper is one of several in this issue on mental health services research conducted by new investigators.
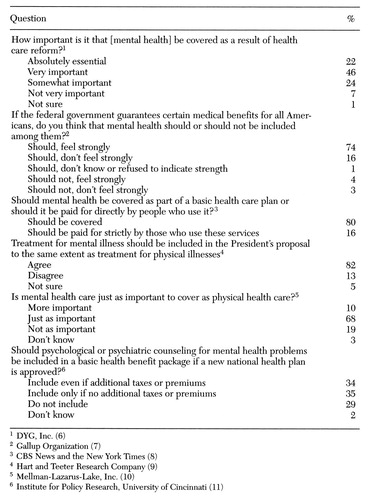 |
Table 1. Responses to selected questions in public opinion surveys reflecting attitudes toward mental health care in policy reform
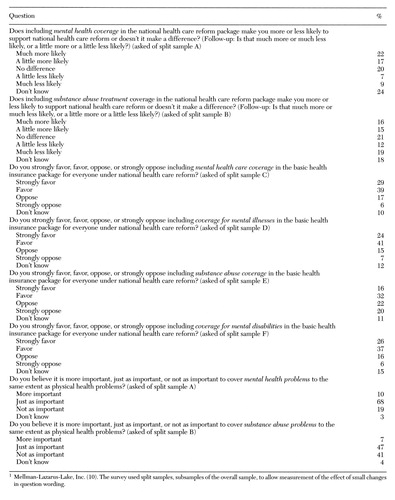 |
Table 2. Responses to variously worded questions about health plan benefit design in a public opinion survey using split samples1
1. US Department of Labor, Bureau of Labor Statistics: Employee Benefits in Medium and Large Firms, 1993. Bulletin no 2456. Washington, DC, Government Printing Office, Nov 1994Google Scholar
2. US Department of Labor, Bureau of Labor Statistics: Employee Benefits in Medium and Large Firms, 1988. Bulletin no 2336. Washington, DC, Government Printing Office, Aug 1989Google Scholar
3. Newhouse JP, Insurance Experiment Group: Free for All? Lessons From the RAND Health Insurance Experiment. Cambridge, Mass, Harvard University Press, 1993Google Scholar
4. Borinstein AB: Public attitudes toward persons with mental illness. Health Affairs 11(3):186-196, 1992Google Scholar
5. Princeton Survey Research Associates: national telephone survey of 1,200 adults conducted for the Harvard School of Public Health and the Henry J Kaiser Family Foundation, Sept 30-Oct 5, 1993Google Scholar
6. DYG, Inc: National telephone survey of 1,346 adults conducted for the Robert Wood Johnson Program on Chronic Mental Illness, Dec 1-11, 1989Google Scholar
7. Gallup Organization: National telephone survey of 1,001 adults conducted for Cable News Network and USA Today, Jul 15-17, 1994Google Scholar
8. CBS News and the New York Times: National telephone survey of 1,368 adults, Mar 28-31, 1993Google Scholar
9. Hart and Teeter Research Company: National telephone survey of 1,006 adults conducted for NBC News and the Wall Street Journal, Sept 10-13, 1993Google Scholar
10. Mellman-Lazarus-Lake, Inc: National survey of 800 registered voters conducted for the Bazelon Center for Mental Health Law, Feb 22-24, 1994Google Scholar
11. Institute for Policy Research, University of Cincinnati: National telephone survey of 1,341 adults conducted for the Institute for Health Policy and Health Services, University of Cincinnati, Jan 7-28, 1994Google Scholar
12. Blum and Weprin Associates: National telephone survey of 1,502 adults conducted for NBC News, Jun 5-8, 1994Google Scholar
13. Los Angeles Times: National telephone survey of 1,682 adults, Apr 16-19, 1994 (published in the Los Angeles Times, Apr 22, 1994)Google Scholar



