Datapoints: Costs of Employee Behavioral Health Care by Diagnosis
Much attention has been focused on behavioral health benefits offered by employers, but little is known about either the types of disorders for which employees themselves receive treatment or the direct medical costs of those disorders to employers. In this column, we present information on adult employees who were enrolled in similar health plans at 46 large self-insured companies in the United States during 1996.
Out of approximately 150,000 covered employees with an average age of 43.4 years, 11,689 (8 percent) filed 87,557 behavioral health claims in 1996. Information on gender was not available. Depression was the most frequent diagnosis, followed by adjustment disorder, anxiety, bipolar disorder, chemical dependencies, impotence, and attention-deficit hyperactivity disorder.
Given that the covered individuals were employed, it is not surprising that diagnoses associated with severe functional impairment such as schizophrenia were rare. In only .0005 percent of employee claims was schizophrenia the primary diagnosis.
Figure 1 shows the average insurance payment per claim in 1996 by diagnostic category for the ten most frequent diagnoses. Figure 2 presents the average 1996 insurance payment per covered employee for six of the diagnostic categories; in four of the categories the average payment did not exceed $1.
The data reported here pertain only to employees of the 46 firms who were enrolled in the health care plans examined; we do not know what percentage of the total firms' workforce this sample represents. However, alcohol dependency, drug dependency, and bipolar disorder were the most expensive diagnostic categories per individual, with average yearly expenditures of $2,017, $1,826, and $1,194, respectively. These expenditure levels are attributable to high rates of inpatient admissions.
Depression was by far the most costly diagnostic category per covered employee ($22.35), not because the average costs per patient were particularly high ($685) but because of the large number of employees receiving treatment. Three percent of all covered employees had a diagnosis of depression.
Acknowledgment
The authors gratefully acknowledge the support of the National Institute of Mental Health.
The authors are associated with the Graduate School of Public Health at the University of Pittsburgh. Dr. Scholle and Dr. Kelleher are also with the department of psychiatry at the University of Pittsburgh Medical Center, where Dr. Kelleher is affiliated with the department of pediatrics. Address correspondence to Dr. Peele at 130 DeSoto Street, Room A649, University of Pittsburgh, Pittsburgh, Pennsylvania 15261 (e-mail, [email protected]). Harold Alan Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
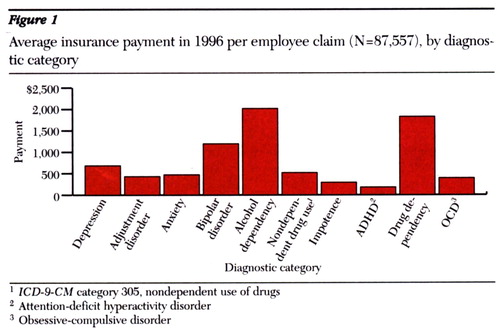
Figure 1. Average insurance payment in 1996 per employee claim (N=87,557), by diagnostic category
1ICD-9CMcategory 305, nondependent use of drugs
2 Attention-deficit hyperactivity disorder
3 Obsessive-compulsive disorder
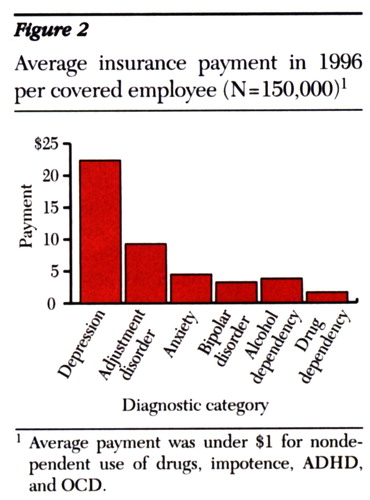
Figure 2. Average insurance payment in 1996 per covered employee (N=150,000)1
1 Average payment was under $1 for nondependent use of drugs, impotence,ADHD and OCD



