Characteristics and Experiences of Adults With a Serious Mental Illness Who Were Involved in the Criminal Justice System
Arrest and incarceration in jails are common experiences for many adults with serious mental illnesses ( 1 , 2 , 3 ). The number of adults with serious mental illnesses booked into jails every year approaches one million ( 4 ). Individuals with a serious mental illness served by the public mental health system appear to be at particularly high risk ( 5 ). For example, criminal justice records indicated that 24% of those receiving services from the Los Angeles County public mental health system in the 1993–2001 period had experienced at least one arrest ( 6 ). Similarly, a cohort study of individuals receiving services from the Massachusetts state mental health agency in the 1991–1992 period showed that 28% were arrested at least once in the following ten years ( 7 ).
There is some evidence to suggest that individuals with mental illness remain in jail longer than inmates without mental illness with the same offenses ( 8 ). High rates of arrest and longer jail stays appear to have resulted in an increased prevalence of serious mental illness in jail populations ( 4 , 9 , 10 , 11 , 12 ). For example, a nationwide survey of U.S. prisons and jails found that 26% of jail inmates in 2002 had at least one previously diagnosed mental health condition before being incarcerated ( 13 ). In addition, in a sample of 822 inmates in two Maryland and three New York jails, use of the Structured Clinical Interview for DSM-IV revealed that 14.5% of male and 31.0% of female inmates had a current serious mental illness ( 14 ).
Individuals with serious mental illnesses present significant financial and management problems for many local jurisdictions and tend to cost significantly more than inmates without these disorders ( 15 , 16 , 17 ). Furthermore, few jails are equipped to provide comprehensive mental health services ( 1 , 18 ). Consequently, many inmates receive little treatment and are often released with inadequate discharge plans ( 18 , 19 ). Not surprisingly, rearrest rates are high ( 4 , 20 , 21 , 22 , 23 ).
Arrests and rearrests of adults with a serious mental illness have been associated with a number of demographic and clinical characteristics, including male gender ( 6 , 7 , 24 , 25 ), nonwhite race ( 7 , 23 ), younger age, homelessness ( 5 , 26 , 27 ), and a co-occurring substance use disorder diagnosis ( 18 , 28 , 29 , 30 , 31 ). Psychiatric diagnosis has not been consistently associated with arrests and rearrests ( 5 , 6 ). The purpose of the study presented here was to determine whether these associations are different for misdemeanor and felony arrests and for time spent in jail. Differences might suggest the existence of subgroups within the population of arrested adults with a serious mental illness that may require different policy and programmatic responses.
Methods
The study was reviewed and approved by the University of South Florida Institutional Review Board. Requirements for informed consent were waived because the study used only pooled administrative data. The study used a retrospective cohort design to identify and to follow over a four-year period individuals with a serious mental illness who were in the Pinellas County, Florida, jail between July 1, 2003, and June 30, 2004.
The study cohort was identified using the following steps. First, based on data in the Pinellas County Criminal Justice Information System (CJIS), a local arrest and jail use data set, we identified all adults between the ages of 18 and 64 years who were in the Pinellas County Jail for at least one day between July 1, 2003, and June 30, 2004. Because processing time would have been significant even if individuals were ultimately released within a 24-hour period, we assumed that all arrests resulted in at least one day in jail. There was no diagnostic information available in the CJIS, requiring additional steps to determine which of these arrestees had a serious mental illness.
Second, we searched all available service event data sets in which diagnostic information was available in order to identify all individuals who had been service recipients in Pinellas County and had been assigned a serious mental illness diagnosis at any time during the four-year period from July 1, 2002, to June 10, 2006. The diagnoses included in the definition of serious mental illness were schizophrenia, schizoaffective disorder, bipolar I disorder, major depressive disorder, other psychotic disorders, and other bipolar and mood disorders. If more than one diagnosis was found in these data sets, the one that appeared most frequently was used. The statewide data sets used included the Medicaid claims files, the service event data set maintained by the Florida Mental Health and Substance Abuse Authority, and an involuntary psychiatric evaluation data set that documents the occurrence of 72-hour involuntary evaluations under Florida's involuntary civil commitment statute ( 32 ). Diagnostic information was available in all three of these data sets and should have been assigned by a health care professional, although there is no way to confirm this using administrative data sets.
Third, Link-King probabilistic-deterministic linking and unduplication software ( www.the-link-king.com ) was used to match the Pinellas County arrestee pool identified in step 1 with the pool of service recipients with serious mental illness identified in step 2. Individuals were included in the cohort if they were in the county jail anytime between July 1, 2003, and June 30, 2004, and had been assigned an included diagnosis in the context of a service encounter that occurred in Pinellas County anytime between July 1, 2002, and June 10, 2006.
Using the service-event data sets described above as well as three county-specific data sets, which documented the social services, homeless services, and emergency medical services that were paid for by the county, we identified for each individual in the cohort all social services; all mental health emergency, inpatient, and outpatient services; and all involuntary psychiatric evaluation contacts that occurred in the county during the study period, as well as the dates of each encounter. We also identified individuals in the cohort who had been assigned a substance abuse diagnosis and those who had reported in the county criminal justice or homeless data sets that they had no residential address or were living in a homeless shelter at some point during the study period.
The Florida Department of Law Enforcement statewide arrest data set and its matching routines were used to identify all arrests experienced by individuals in the cohort as well as the dates on which the arrests occurred during the four-year study period. Charges at arrest were organized into misdemeanor and felony categories. County data were used to determine the numbers of days spent in jail in Pinellas and adjoining Hillsborough County associated with each arrest for each individual. Jail time was not available for arrests that occurred in other counties. Because in Florida individuals are generally not retained in county jails for more than 365 days, we also accessed the Florida Department of Correction's information system to determine which individuals in our cohort were in prison during the study period and the associated dates of admission and release.
Anticipating that not all participants would be living in Pinellas County for the entire study period, we recorded criminal justice and mental health services and supports longitudinally across 16 periods ("quarters") that were 90 days long. The first period began on July 1, 2002, and the last ended on June 10, 2006. All mental health service encounters, arrests, and days in jail and prison for each individual were assigned to one of these quarters based on the dates the contacts occurred. The number of "eligible quarters" was determined for each individual by reviewing his or her longitudinal records of mental health and criminal justice contacts. If a Pinellas County specific contact was recorded during any of the four successive quarters over a year with the first period beginning on July 1, 2002, these four quarters were considered eligible for that individual. If no contacts were recorded during any one of the successive quarters, the four quarters of that year were considered ineligible, because it was assumed that the individual was not residing in Pinellas County at the time. Thus individuals could have had four, eight, 12, or 16 eligible quarters. On average, persons were eligible for a mean±SD of 13.8±3.1 quarters (range, four to 16 quarters). Fifty-nine percent (N= 2,224) of the sample was eligible for the entire study period, and 2% (N= 75) was eligible for only four quarters. Because the timing of homelessness incidents was not clear in our data sets, we defined it as a dichotomous variable, simply indicating whether or not each individual had been homeless at any time during the study period.
In the main analyses we used generalized estimating equations (GEEs) to estimate associations between baseline characteristics and service contact variables and associations between baseline and service characteristics and risks of a felony arrest, a misdemeanor arrest, and of additional days in jail. GEE was chosen because these models can account for repeated observations with the same individual (which can lead to artificially large effects) and are flexible with respect to the distribution of the outcome (both arrest and jail days were count data, which are not normally distributed) ( 33 ).
The analyses were conducted using SAS procedure GENMOD ( 34 ). We calculated empirical (robust) standard errors to account for repeated observations for the same participant across quarters by increasing the standard error of measurement. In analyses with arrests as the outcome, we used Poisson regression for count data. When jail days were the outcome, we used negative binomial regression because it yielded a superior model fit to Poisson regression.
The results were adjusted for differential exposure across participants because of differences in the time in the study by including the number of eligible quarters and total days in the community (as opposed to days in jail or prison) in each quarter as offset variables. We did not adjust for community inpatient days because short lengths of stay did not substantially affect exposure to the possibility of arrests and days in jail. We included in the models age group (20 years or younger and 21–39, 40–50, and 51–64 years), gender, race, psychiatric diagnosis, substance use disorder diagnosis (yes or no), and homelessness (yes or no). In addition, we included mental health-related inpatient or emergency room contacts, mental health outpatient contacts, and involuntary psychiatric evaluations in each quarter as time-varying variables. We lagged these variables by one quarter to ensure that we were studying the potential effects of mental health services on criminal justice contacts rather than the impact of criminal justice involvements on the subsequent receipt of mental health services. We calculated standardized coefficients (betas) and then estimated odds ratios (ORs) and 95% confidence intervals (CIs) based on the coefficients and corresponding robust standard errors.
Results
The matching process utilizing the combined criminal justice and service utilization data set identified 3,769 individuals with a serious mental illness who were in the county jail between July 1, 2003, and June 30, 2004. This represented 10.1% of the 37,236 individuals who were in the jail at some time during that one-year period. On the basis of these data, 17.7% of females (N=1,545 of 8,737) and 7.8% of males (N=2,224 of 28,499) who were in the jail had a serious mental illness. The characteristics of these individuals are presented in Table 1 .
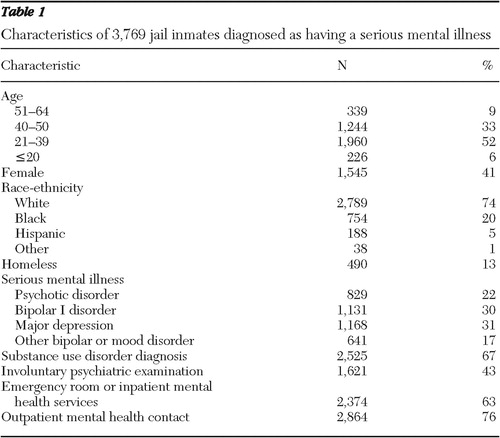 |
Persons included in the study were on average 36±10 years of age and predominantly male and white. The most common mental illness diagnoses were major depression (31%), bipolar I disorder (30%), and psychotic disorders (22%). Sixty-seven percent of the sample had a substance use disorder diagnosis, and 13% had been homeless at some point in the study period. Most individuals had at least one outpatient contact and one emergency room or inpatient contact for mental health services during the study period.
The criminal justice experiences of the sample are presented in Table 2 . Fifty-seven percent (N=2,148) of participants had at least one felony arrest, and 86% (N=3,241) had at least one misdemeanor arrest. Participants experienced a total of 17,463 arrests, with a mean of 4.6±3.9 arrests per individual. Persons spent an average of 151±175 days in jail (mean number of days in jail per arrest, 33±53 days) and 48±148 days in prison. Furthermore, they experienced about one arrest for every three eligible quarters and 11±24 days in jail for every eligible quarter.
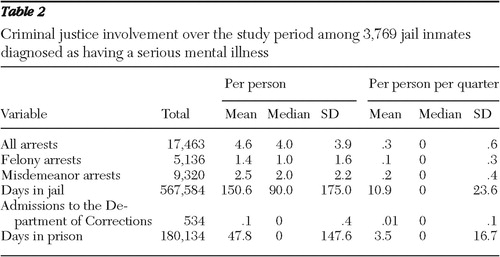 |
Table 3 presents the results of the fully adjusted GEE analysis of the associations between participant characteristics and experiences and the risk of each additional day spent in jail. Participants in all the younger age groups were likely to spend more days in jail than those aged 51–64. Men were likely to spend more days in jail than women. Being black or Hispanic, having been homeless, and having a substance use disorder diagnosis were associated with more jail days. Finally, an involuntary psychiatric examination in the previous quarter was associated with additional days in jail, whereas outpatient mental health contacts were associated with fewer days in jail.
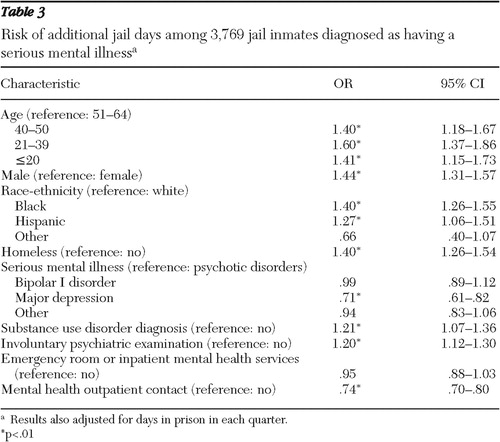 |
Table 4 presents fully adjusted results from the GEE analysis for the risks of all types of arrests. The overall risk of arrest was greater among younger persons and decreased at successively higher ages. The risk of arrest also increased for men, homeless individuals, those with a substance abuse diagnosis, and those who had an involuntary psychiatric examination in the previous quarter. Being black or of other race or ethnicity (as opposed to white) was associated with lower risk of arrests. Having an inpatient or emergency room contact increased the risk of arrest, whereas an outpatient contact was associated with reduced risk of arrest in the next quarter.
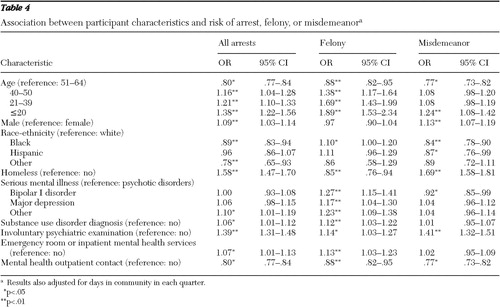 |
Somewhat different results emerged when we analyzed the risk of a felony and misdemeanor arrest as opposed to total arrests in separate, fully adjusted models. The associations between younger age group and a greater risk of arrest appeared substantially stronger when felony arrests were the outcome. With respect to race-ethnicity, results for the risk of misdemeanor arrest were consistent with those for all arrests, including the finding that being black was associated with lower risk of misdemeanor arrest. In addition, the association between being Hispanic (as opposed to white) and lower risk of misdemeanor arrest was statistically significant. For felonies, blacks tended to have higher risk of arrest than whites. Furthermore, homelessness was associated with a reduced risk of a felony arrest but with an increased risk of total arrests and of a misdemeanor arrest. The risk of a felony arrest was higher for those with a nonpsychotic disorder. Bipolar I disorder was also associated with a slightly lower risk of misdemeanor arrest. There was an association between a substance use disorder diagnosis and felony arrest but not misdemeanor arrest. Finally, involuntary psychiatric examinations in the previous quarter increased the risk of all types of arrests, whereas outpatient contacts had the opposite effect. In both cases the associations were stronger for misdemeanors than for felonies.
Discussion
The findings of this study confirm that many individuals with a serious mental illness spend time in jail and are frequently rearrested. The characteristics of individuals who have elevated risks of misdemeanor arrests and of spending time in jail associated with these arrests are somewhat different than those of individuals who have elevated risks of felony arrests. Being male, being homeless, having an involuntary psychiatric evaluation, and not having outpatient mental health treatment in the previous quarter independently increased the odds of subsequent misdemeanor arrests and of additional days in jail. On the other hand, being black, being in a younger age group, having a nonpsychotic diagnosis, and having a co-occurring substance use disorder diagnosis were all independently associated with felony arrests. An involuntary psychiatric evaluation and the lack of outpatient mental health services in the previous quarter also increased the odds of a felony arrest, but the associations were not nearly as strong as they were for misdemeanor arrests. Because felonies typically result in longer incarcerations, it is not surprising that, with the exception of psychiatric diagnosis, all variables that increased the risk of felony arrest also increased the risk of additional days in jail.
Although different methods and definitions make comparisons imprecise, our estimate that 10.1% of all individuals who spent time in jail during our index year had a serious mental illness was in the range reported elsewhere ( 4 , 9 , 19 , 27 ). However, our estimate of 17.7% of females may be low in view of a recent finding that 31% of women had a serious mental illness around the time of jail admission ( 14 ).
The differences in the characteristics of individuals with elevated risks of misdemeanor and felony arrests suggest the existence of subgroups within the cohort of individuals with a serious mental illness who become involved in the criminal justice system. Individuals who are frequently arrested for misdemeanors and who spend significant amounts of time in jail are of particular interest because they place heavy demands on the criminal justice system and their behaviors do not generally present a public safety risk (although they may have a significant impact on the person's quality of life).
Individuals in this subgroup were more likely to have been male and homeless and to have received an involuntary psychiatric evaluation but no outpatient services in the previous quarter. These same characteristics and experiences also increased the risk of additional days in jail.
Although the association between male gender and criminal justice involvement is not a new finding ( 5 , 6 , 7 , 24 , 25 ), its differential association with misdemeanor and felony arrests may be. Male gender increased the risk of a misdemeanor but not a felony arrest. The associations between age and arrests were also different for misdemeanor and felony arrests. Consistent with previous research, felony arrest rates in our study continually declined as the age of individuals increased ( 6 , 7 ). This was not the case for misdemeanor arrests. Individuals in the 21–39 and 40–50 age groups were no more likely to be arrested for a misdemeanor than were individuals in the 50–64 age group. The relationships between being black and risk of arrests require further study related to the specific behaviors that produced different kinds of arrests among black individuals and white individuals. For example, was the higher risk of felony arrests among blacks related to different kinds of criminal behavior or to differences in how law enforcement responds to the same or similar behavior exhibited by blacks and nonblacks?
The importance of homelessness, defined as having no residential address or living in a homeless shelter, requires special comment. Although somewhat crudely measured, homelessness had the strongest independent association with both misdemeanor arrests and additional days in jail. Homelessness actually reduced the risks of a felony arrest. There are several possible explanations for these associations. First, homeless individuals with a serious mental illness are extremely poor and therefore frequently commit survival crimes, like petty theft or shoplifting ( 26 , 35 ). Second, homeless individuals are living on the streets where these survival crimes, as well as nuisance crimes like trespassing, disorderly conduct, and public intoxication, are more readily observable to law enforcement ( 17 , 36 ). Third, although many of their crimes are misdemeanors, homeless individuals tend to offend repeatedly ( 37 ), which increases the probability of arrest and incarceration ( 27 ). Finally, because they lack financial resources and a permanent address, homeless individuals are less likely to make bail or to be released on their own recognizance ( 27 ).
The distinction between misdemeanors and felonies was also important when we looked at the effect of diagnosis. All serious mental illness categories had elevated risks of a felony arrest, compared with psychotic disorders. There were no associations with misdemeanor arrests except that persons with major depression were less likely than those with psychotic disorders to experience such an arrest.
The relationship between a co-occurring substance use disorder diagnosis and arrests has been well established ( 24 , 29 , 38 ). Our findings suggest this may not be the case for all types of arrests. A substance use disorder diagnosis increased the risk of felony arrests and additional days in jail. It was not independently associated with misdemeanor arrests.
Consistent with previous work, our study found that inpatient contacts increased the odds of subsequent arrests ( 38 ). However, in our study this was only the case for felony arrests. On the other hand, the experience of an involuntary psychiatric evaluation (which usually occurs in an inpatient setting) in the previous quarter increased the odds of a misdemeanor far more than a felony arrest in the subsequent quarter. (OR=1.41 versus 1.14). This experience also increased the odds of additional days in jail in the following quarter. In Florida involuntary psychiatric evaluations are usually a response to a crisis and are most often initiated by law enforcement. Even when they are not, law enforcement is generally involved in the delivery of the individual to a receiving facility for evaluation. Observing repeated minor law violations of individuals who had previously been transported to such a facility may lead to subsequent misdemeanor arrests based on the conclusion that, for whatever reason, treatment did not work ( 36 ). It is not clear why emergency or inpatient care increased the odds of a felony but not a misdemeanor arrest. The answer may lie in the reasons for the previous inpatient contact, which may have included medical problems associated with substance abuse or injuries resulting from physical confrontations in the community.
Although the presence of an involuntary psychiatric evaluation in the previous quarter increased the risks of misdemeanor arrests and additional days in jail, we found that the absence of outpatient mental health services produced the same effects. The association between outpatient service utilization and arrests has been observed by others ( 4 , 21 , 22 ). In our study individuals who did not receive these services in the previous quarter were 23% more likely to be arrested for a misdemeanor, 12% more likely to be arrested for a felony, and 26% more likely to spend additional days in jail in the following quarter.
The results of this study should be interpreted with caution for several reasons. First, we focused on only one county in Florida, but treatment and criminal justice systems vary considerably among local jurisdictions in the state and nation. Second, we relied exclusively on administrative data, which may lack the richness and detail sometimes necessary to understand the phenomena under study. Third, diagnosis was not validated, and we relied on a frequency approach to assigning diagnosis when more than one appeared in the data sets. Finally, our identification of individuals with a serious mental illness relied on individuals having contact with the publicly supported treatment system in Pinellas County. It therefore fails to include persons who were treated in the public system in other counties or other states, persons who were treated in a private system, and persons who may have had an undiagnosed mental illness.
Conclusions
This study examined the associations between individual characteristics and experiences and the risks of arrests for misdemeanors and felonies and additional days in jail. The finding that the characteristics associated with the risks of misdemeanor and felony arrests were somewhat different suggests the existence of subgroups within the population of adults with a serious mental illness and criminal justice involvement that may have different needs. A special focus on the group with elevated risks of misdemeanor but not felony arrests and of additional days in jail could help policy makers reduce the pressure on local criminal justice and judicial systems and facilitate the recovery of the consumers involved.
Acknowledgments and disclosures
This project was funded by Ortho-McNeil Janssen Scientific Affairs.
Dr. Howe owns stock in Johnson & Johnson (Ortho-McNeil Janssen Scientific Affairs is part of the Johnson & Johnson family of companies). The other authors report no competing interests.
1. Lamb HR, Weinberger LE: The shift of psychiatric inpatient care from hospitals to jails and prisons. Journal of the American Academy of Psychiatry and the Law 33:529–534, 2005Google Scholar
2. Draine J, Solomon P, Meyerson A: Predictors of reincarceration among patients who received psychiatric services in jail. Hospital and Community Psychiatry 45:163–167, 1994Google Scholar
3. McGuire JF, Rosenheck RA: Criminal history as a prognostic indicator in the treatment of homeless people with severe mental illness. Psychiatric Services 55:42–48, 2004Google Scholar
4. Morrissey JP, Cuddeback GS, Cuellar AE, et al: The role of Medicaid enrollment and outpatient service use in jail recidivism among persons with severe mental illness. Psychiatric Services 58:794–801, 2007Google Scholar
5. Theriot MT, Segal SP: Involvement with the criminal justice system among new clients at outpatient mental health agencies. Psychiatric Services 56:179–185, 2005Google Scholar
6. Cuellar AE, Snowden LM, Ewing T: Criminal records of persons served in the public mental health system. Psychiatric Services 58:114–120, 2007Google Scholar
7. Fisher WH, Roy-Bujnowski KM, Grudzinskas AJ, et al: Patterns and prevalence of arrest in a statewide cohort of mental health care consumers. Psychiatric Services 57:1623–1628, 2006Google Scholar
8. McPherson W: Managing the mental health population at the Broward Sheriff's Office. Corrections Today 70:62–67, 2008Google Scholar
9. Teplin LA: The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. American Journal of Public Health 80:663–669, 1990Google Scholar
10. Teplin LA, Abram KM, McClelland GM: Prevalence of psychiatric disorders among incarcerated women: pretrial jail detainees. Archives of General Psychiatry 53:505–512, 1996Google Scholar
11. James DJ, Glaze LE: Mental Health Problems of Prison and Jail Inmates: Bureau of Justice Statistics Special Report. Washington, DC, Bureau of Justice Statistics, 2006Google Scholar
12. Ditton PM: Mental Health and Treatment of Inmates and Probationers: Bureau of Justice Statistics Special Report. Washington, DC, Bureau of Justice Statistics, 1999Google Scholar
13. Wilper AP, Woolhandler S, Boyd JW, et al: The health and health care of US prisoners: results of a nationwide survey. American Journal of Public Health 99:666–672, 2009Google Scholar
14. Steadman HJ, Osher FC, Clark P, et al: Prevalence of serious mental illness among jail inmates. Psychiatric Services 60:761–765, 2009Google Scholar
15. Domino ME, Norton EC, Morrissey JP, et al: Cost shifting to jails after a change to managed mental health care. Health Services Research 39:1379–1401, 2004Google Scholar
16. Clark RE, Ricketts SK, McHugo GJ: Legal system involvement and costs for persons in treatment for severe mental illness and substance use disorders. Psychiatric Services 50:641–647, 1999Google Scholar
17. Lamberti JS, Weisman R: Persons with severe mental disorders in the criminal justice system: challenges and opportunities. Psychiatric Quarterly 75:151–164, 2004Google Scholar
18. Veysey BM, Steadman HJ, Morrissey JP, et al: In search of the missing linkages: continuity of care in US jails. Behavioral Sciences and the Law 15:383–397, 1997Google Scholar
19. Teplin LA, Abram KM, McClelland GM: Mentally disordered women in jail: who receives services? American Journal of Public Health 87:604–609, 1997Google Scholar
20. Harris V, Koepsell TD: Criminal recidivism in mentally ill offenders: a pilot study. Bulletin of the American Academy of Psychiatry and Law 24:177–186, 1996Google Scholar
21. Solomon P, Draine J, Marcus SC: Predicting incarceration of clients of a psychiatric probation and parole service. Psychiatric Services 53:50–56, 2002Google Scholar
22. Herinckx HA, Swart SC, Ama SM, et al: Re-arrest and linkage to mental health services among clients of the Clark County Mental Health Court Program. Psychiatric Services 56:853–857, 2005Google Scholar
23. Prince JD: Incarceration and hospital care. Journal of Nervous and Mental Disease 194:34–39, 2006Google Scholar
24. Quanbeck CD, Stone DC, McDermott BE, et al: Relationship between criminal arrest and community treatment history among patients with bipolar disorder. Psychiatric Services 56:847–852, 2005Google Scholar
25. Cox JF, Morschauser PC, Banks S, et al: A five-year population study of persons involved in the mental health and local correctional systems: implications for service planning. Journal of Behavioral Health Services and Research 28:177–187, 2001Google Scholar
26. Greenberg GA, Rosenheck RA: Jail incarceration, homelessness, and mental health: a national study. Psychiatric Services 59:170–177, 2008Google Scholar
27. McNiel DE, Binder RL, Robinson JC: Incarceration associated with homelessness, mental disorder, and co-occurring substance abuse. Psychiatric Services 56:840–846, 2005Google Scholar
28. Osher FC: Integrated mental health/substance abuse responses to justice involved persons with co-occurring disorders. Presented at Evidence-Based Practice for Justice Involved Individuals: Integrated Mental Health/Substance Abuse Expert Panel Meeting, Bethesda, Md, Nov 29, 2005Google Scholar
29. White MD, Goldkamp JS, Campbell SP: Co-occurring mental illness and substance abuse in the criminal justice system. Prison Journal 86:301–325, 2006Google Scholar
30. Abram KM, Teplin LA: Co-occurring disorders among mentally ill jail detainees. American Psychologist 46:1036–1045, 1991Google Scholar
31. Swartz JA, Lurigio AJ: Serious mental illness and arrest. Crime and Delinquency 53:581–604, 2007Google Scholar
32. Part I Florida Mental Health Act (Baker Act). Sec 394.451 (2008)Google Scholar
33. Hanley JA, Negassa A, Edwardes MD, et al: Statistical analysis of correlated data using general estimating equations: an orientation. American Journal of Epidemiology 157:364–375, 2003Google Scholar
34. SAS System for Microsoft Windows. Cary, NC, SAS Institute, 2003Google Scholar
35. Hiday AV, Wales HW: Civil commitment and arrests. Forensic Psychiatry 16:575–580, 2003Google Scholar
36. Lamb HR, Weinberger LE, Gross BH: Mentally ill persons in the criminal justice system: some perspectives. Psychiatric Quarterly 75:107–126, 2004Google Scholar
37. Baillargeon J, Binswanger IA, Penn JV, et al: Psychiatric disorders and repeat incarcerations: the revolving prison door. American Journal of Psychiatry 116:103–109, 2009Google Scholar
38. Prince JD, Akincigil A, Bromet E: Incarceration rates of persons with first-admission psychosis. Psychiatric Services 58:1173–1180, 2007Google Scholar



