The Role of Social Network and Support in Mental Health Service Use: Findings From the Baltimore ECA Study
Mental health service use is low across countries, and rates of unmet needs in developed countries, including the United States, vary between 35% and 50% ( 1 ). Results from the Baltimore Epidemiologic Catchment Area (ECA) program show that use of general medical services for emotional problems increased from 11.7% in 1981 to 18.2% in 1996 ( 2 ). However, a large number of people with mental illness still fail to receive adequate care.
Researchers have posited factors associated with mental health service use. Andersen ( 3 , 4 ) outlined three core components: predisposing factors (for example, demographic factors, social structure, and health beliefs), enabling factors (for example, socioeconomic factors), and need (that is, perceived and evaluated need for health care services). More recently, Pescosolido and Boyer ( 5 ) developed a network episode model, in which four components work interactively to influence the decision to use or continue with mental health services. The components include episode-base of an individual, which consisted of sociodemographic variables, personal health background, nature of event, and organizational constraints to accessing care, such as finance and access; social support system, which included social network structure, content, and function; illness career, which included factors like sick role, recovery, compliance, and spacing of consultations; and treatment system, which included structure, content, and functions of treatment network .
A common factor across these models is social support. Cobb ( 6 ) defined social support in terms of information that "one is cared for and loved," one is "esteemed and valued," and one "belongs to a network of communication and mutual obligation." It has also been defined in terms of a "metaconstruct," which comprises support network resources, supportive behavior, and subjective appraisal of support ( 7 ). Social network is a more objective concept corresponding to the number and frequency of contacts with support networks, whereas social support is a more subjective concept of perceived support. Both network and support can act as coping resources. Researchers found that social support has a buffering effect on medical service use in stressful situations ( 8 ). Others did not find evidence to support the stress-buffering effect of social support on service use but found that the number of close friends or relatives reduced service use as a direct effect ( 9 ). Both main and buffering roles of social network and support have been studied in relation to mental disorders, stress, and mental health service use ( 5 , 10 , 11 ).
There has been considerably less research examining the role of social support in accessing mental health services among individuals not experiencing a significant life event or a particular stressful situation. A review of the literature on the effect of social support on mental health service use among patients with severe mental disorders concluded that a smaller social network and less social support were associated with more frequent hospital admissions ( 12 ). Most of the persons in this review were drawn from different hospitals. Among psychiatric outpatients, a less cohesive social structure was associated with a delay in accessing services because of a delay in recognizing psychological problems ( 13 ). Others also found among Medicaid beneficiaries that higher social network index scores, based on the number of contacts and frequency of interaction were associated with accessing more inpatient psychiatric care in local hospitals but less inpatient and outpatient services in state psychiatric hospitals ( 14 ).
Current research on social networks and social support in relation to mental health service use is restricted to psychiatric service use by people with serious mental health problems. There has been limited research on the association between specific sources of social network and social support and different types of mental health service use in population-based samples. The aim of the study presented here was to examine the association between specific elements of the social network and social support and four different types of mental health services in a population-based cohort sample. Our hypothesis was that the association would vary across friends, relatives, and spouse (or partner) and that increased social network and social support would be associated with decreased service use.
Methods
Sample
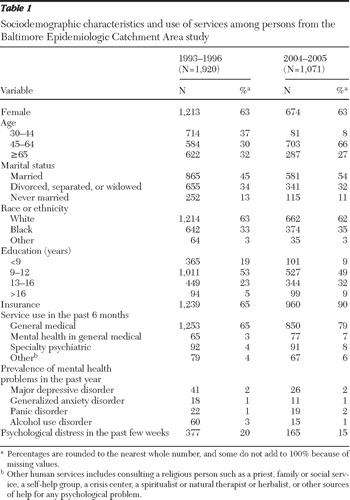
Data for this study came from the Baltimore cohort in the ECA study, which gathered population-based data on mental health across four time points: 1981, 1982, 1993–1996, and 2004–2005. In 1981, there were 3,481 participants, of whom 1,071 were reinterviewed in the last wave of data collection. Participants provided written informed consent. All data collection procedures in the ECA study were approved by the Johns Hopkins School of Public Health Institutional Review Board. For the study presented here, data from 1993–1996 and 2004–2005 were analyzed, because the survey questions were similar for those two time points. There were 1,920 participants in the 1993–1996 sample and 1,071 in the 2004–2005 sample. The demographic characteristics for the participants are provided in Table 1 .
 |
Measures
The interviews were carried out by trained lay interviewers and assessed the following constructs as detailed below.
Social network. Separate questions were asked regarding the number of relatives and the number of friends that participants had kept in touch with. A second set of questions inquired about the frequency with which the respondent was in contact with friends or relatives, including physical meetings, e-mails, postal mail, or phone. All questions were asked in reference to the past six months.
Social support. Another set of questions asked about the perceived quality of support that the respondent felt that friends would provide. Separate questions were then asked about the perceived quality of support from relatives and the perceived quality of support from the spouse (or partner). Examples of the questions related to a spouse or partner were "How much does your (husband/wife/partner) really care about you?" "How much can you rely on your (husband/wife/partner) for help if you have a serious problem?" "How much can you relax and be yourself around your (husband/wife/partner)?" "How often does your (husband/wife/partner) make too many demands on you?" "How often does (he/she) let you down when you are counting on (him/her)?" "How often does (he/she) get on your nerves?" ( 15 , 16 ). All questions were asked in reference to the past six months. Possible summary scores range from 6 to 24, with higher scores indicating better quality of perceived support.
Mental health service use. A set of questions inquired about use of services during the past six months. On the basis of a previous algorithm ( 17 ), they were collapsed into the following four groups: general medical services (any care from a health professional), mental health services within the general medical system (use of a medical doctor or hospital emergency room or day hospital for emotional, mental health, or drug- or alcohol-related problems), specialty psychiatric services (use of a mental health specialist in either a family clinic or private practice, mental health center, psychiatric outpatient clinic in either a general or psychiatric hospital or Veterans Affairs hospital, drug clinic, or alcohol clinic), and other human services (consulting a religious person such as a priest, family or social service, a self-help group, a crisis center, a spiritualist or natural therapist or herbalist, or other sources of help for any psychological problem).
Mental health. Trained interviewers administered the Diagnostic Interview Schedule, which allowed a diagnosis to be made in accordance with DSM-III-R criteria ( 18 ). Any occurrence of the following four common mental disorders—major depressive disorder, generalized anxiety disorder, panic disorder, or alcohol use disorder (both abuse and dependence)—within the past year was adjusted for separately in the statistical models. More serious mental disorders, such as schizophrenia, were not included because of the low prevalence in the sample. The 20-item General Health Questionnaire ( 2 , 19 ) was also administered. A score of ≥4 was included in the statistical models to adjust for psychological distress within the past few weeks of the interview.
Demographic characteristics and health status. Information was collected on the sample regarding demographic characteristics. The following variables were included as covariates in the models: age (30–44 years, 45–64 years, or ≥65 years), sex, race or ethnicity (white, black, or other), marital status (married, previously married, or never married), years of education (<13 years or ≥13 years), presence of any form of health insurance, and presence of physical illnesses before 1993–1996 (for example, diabetes mellitus, heart trouble, hypertension, or arthritis).
Analysis
Descriptive analyses were first conducted, followed by longitudinal data analysis using generalized estimating equations (GEE) ( 20 ) with an exchangeable correlation matrix. Both bivariate and multivariate logistic regressions were done using GEE. All analyses were performed in Stata 9.0 ( 21 ).
The longitudinal analyses were first conducted using unweighted data. All models were adjusted for the demographic characteristics and health status covariates outlined above. In addition, the presence of any of the above four mental disorders before 1993–1996 and use of any of the above four groups of mental health services before 1993–1996 were included as covariates. Each model was separately tested by including specific measures of social network or social support and specific mental disorders or psychological distress. We did not test for interactions because we did not have any specific hypotheses regarding effect modification. All models showing significant results for the predictors of primary interest (social network and support) were refitted to determine the most parsimonious model on the basis of "quasi-likelihood under the independence model criteria" ( 22 , 23 ). Sex was included as a covariate in each multivariate model, even if the variable was not necessary for the final parsimonious model.
To explore whether nonresponse to items and attrition had an influence on the pattern of findings, we reran all the longitudinal analyses using weights to account for item nonresponse and attrition across the two time points. The inverse probability weights were generated using multiple imputations, and details are provided in previous publications ( 24 ). Weighted analyses were done by using three methods. The first two methods were consistent with the National Longitudinal Survey on Youth ( 25 , 26 ). The first involved using all respondents from interviews across different time points in a selected sample population, regardless of attrition, and using the weight corresponding to the initial year of that sample (that is, 1993–1996 weights in the study presented here). The second method involved including only the respondents who completed both of the interviews and using the weight of the past year (that is, 2004–2005 weights in the study presented here). Finally, analyses were done using the weights corresponding to 1993–1996 and 2004–2005 for each observation from the two time points. However, in such cases the correlation structure between repeated measures had to be ignored because time-varying weights could not be computed in our models while using correlated observations. Results were compared for consistent patterns across all analyses: unweighted analyses and analyses weighted in three different ways.
The point estimates were similar for both unweighted and weighted analyses. Because using only completers can lead to selection bias ( 27 ) and because using the final method of time-varying weights ignores the correlation between repeated measures, the tables report the bivariate and multivariate analyses using data weighted by the attrition weights of 1993–1996. However, 112 observations from 1993–1996 had to be dropped because these persons did not respond to survey questions that were used to calculate the weights. Therefore, a weight could not be calculated for these persons. Thus the weighted sample had 1,808 individuals in 1993–1996.
Because our primary aim was to examine the association between each social network and social support measure and each type of service across four different mental disorders and psychological distress, we applied a two-tailed Bonferroni correction (p≤.01) to adjust for multiple tests. We also indicate estimates with p values less than .05 for the bivariate and multivariate analyses, even though such estimates have not been adjusted for Bonferroni correction. Parsimonious models were tested, and the estimates were reevaluated to determine if there were any major changes in the parameter estimates.
Results
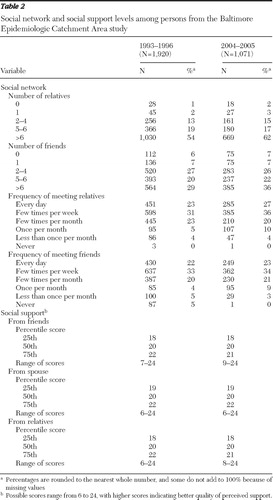
Across both time points, more than half had regular contact with more than six relatives, and about one-third had regular contact with more than six friends ( Table 2 ). About one-third of the population met with their relatives or friends a few times per week. The participants had a median perceived social support score of 20 for friends, relatives, and spouse ( Table 2 ). The prevalence of general medical service use was between 65% and 79% across both time points, whereas use of mental health services, either within general medical practices, specialty psychiatric services, or other human services was low (3% to 8% across both time points) ( Table 1 ).
 |
Among the different types of services, only general medical service use in 1993–1996 was significantly associated with attrition between 1993–1996 and 2004–2005 ( χ2 =9.35, df=1, p=.002). General medical service use was higher among those lost to follow-up than in the rest of the 1993–1996 sample. Death was the most prevalent cause for loss to follow-up. Those who died were more likely to use general medical services because they were elderly and physically ill. However, general medical service use was still higher in 2004–2005 than in 1993–1996 because of the increasing age of the cohort.
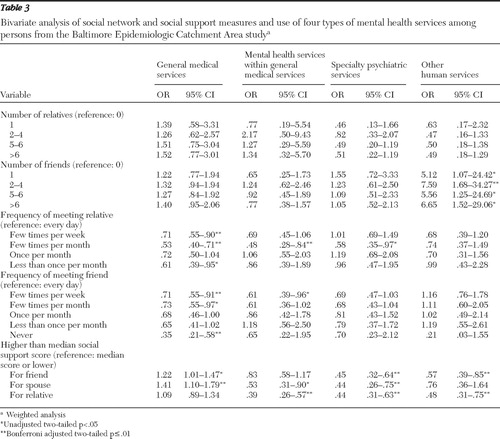
We first examined the unadjusted trends in the regression models ( Table 3 ). These analyses indicated that reduced frequency of meeting friends or relatives was generally associated with a reduced odds of accessing general medical services, whereas increased social support of friends or spouse was associated with increased odds of general medical service use. A visit to a general medical practitioner to seek help for emotional problems was 47% and 61% less likely when there was increased social support from the spouse and relatives, respectively. Use of specialty psychiatric services and other human services was also reduced by about 24% to 56% when there were higher levels of social support from friends, the spouse, and relatives. However, having more than six friends was associated with an almost sevenfold increase in the odds of using other human services.
 |
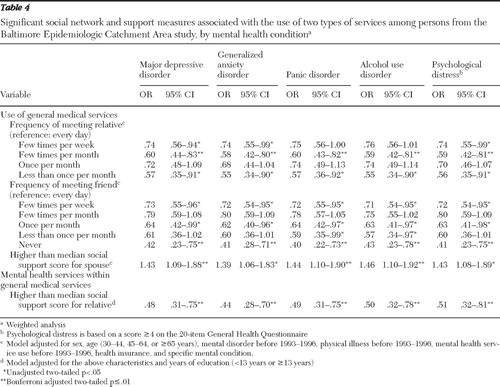
The effect of social network and social support on general medical service use indicated that a reduced frequency of contact with either friends or relatives was associated with reduced odds of accessing services across different mental health conditions ( Table 4 ). Meeting a relative a few times per month was associated with a 40% reduction in the odds of using general medical services, compared with meeting every day. Compared with meeting a friend every day, never meeting a friend was associated with a 60% reduction in the odds of using general medical services. In contrast, a higher than median level of spousal support was associated with a 43% to 46% increase in the odds of using general medical services when the person had major depressive disorder, panic disorder, or alcohol use disorder. A higher than median level of social support from a relative was associated with almost 50% reduction in the use of general health services for mental health problems.
 |
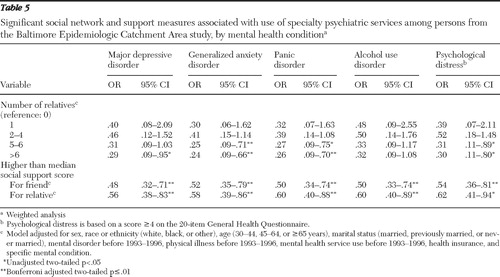
Some social network and social support measures were significantly (p≤.01) associated with specialty psychiatric service use ( Table 5 ), but none were associated with use of other human services. The findings indicate that having contact with more than six relatives was associated with almost 75% decreased use of specialty psychiatric services when the person had generalized anxiety disorder and panic disorder, and having a higher than median level of social support from a friend or relative reduced use by almost 40% to 50% across all mental health conditions. Regular contact with more than six friends was associated with almost a five- to sixfold increased use of other human services across different mental health conditions (p<.05) (results not shown).
 |
Discussion
Most of the extant research examining the link between social support, social networks, and mental health service use has focused on clinical samples and is limited to either psychiatric inpatient or outpatient services. This population-based study highlighted the association between social network and social support and use of different types of mental health services across different mental health conditions. It supported our hypotheses that the association between service use and social network and social support varied across friends, relatives, and spouse, but the association differed in that increased social network and social support was not uniformly associated with decreased use of services. However, this was not surprising because of the variation in existing evidence. There were similar patterns of service use across different mental health conditions, which suggest that one's social network or social support was largely unrelated to the diagnosis.
Specifically, these findings indicated that for general medical service use, social network measures (for example, frequency of meeting friends or relatives) were directly related to service use, such that less frequent contact was associated with reduced odds of accessing services. In contrast, increased social support from the spouse was associated with increased service use. These findings contradict those in a literature review ( 12 ), which found that less social network or social support was generally associated with more service use. However, our findings support more recent research that indicated that higher scores on a composite social network index (especially for contacts with relatives and friends) were associated with use of inpatient psychiatric services in local hospitals ( 14 ).
It is important to note that we examined the effect of number and frequency of contacts separately. It is possible that for general medical services one's social networks and social support are more likely to suggest early consultation because it carries less stigma than formal psychiatric services ( 28 ). Also, when symptoms first appear, the cause of illness is often unclear and one typically assumes physical rather than psychological factors as the causal agent. However, once the cause is identified as related to mental health, the use of even general medical services to discuss the problem is reduced if one has good social support from relatives. We hypothesize that this might be a reflection of the stigma associated with more formal mental health services and mental health in general ( 29 ).
Consistent with previous research ( 9 , 12 , 30 , 31 ), increased social network (that is, contact with more relatives and greater social support from friends and relatives) was associated with less use of specialty psychiatric services. Unadjusted results showed that increased levels of social support were associated with reduced use of other human services, a result similar to that found in use of other mental health services and probably reflective of stigma (because other human services were used for mental illness). On the other hand, having contact with more than one friend was associated with increased use of other human services. This was evident even in the adjusted analysis. Increased use of other human services when in contact with more than six friends is an indication that a large number of casual contacts constitutes a less dense network than that found with relatives or spouse. The network of a large number of friends is less dense because of less intimacy, emotional intensity, and lower social support; however, such a large number of contacts tends to provide more information about available services, thus encouraging help seeking ( 32 ). A network of casual contacts has been defined as constituting weak ties ( 33 ), a concept based on the strength and quality of interactions within one's network, where weak ties result in sharing of general information about multiple services and strong ties result in sharing of detailed information about fewer specific services. Increased social support could be indicative of such strong ties, thus being associated with reduced use of other human services, as seen in the unadjusted results. Others also found evidence to support the concept of weak ties, especially for nonformal care ( 34 ).
It is important to consider some limitations when interpreting these findings. There was a relatively large loss to follow-up between 1993–1996 and 2004–2005, the majority of whom had died. Weighted analyses accounted for attrition and reduced biases resulting from attrition, but residual biases are possible. However, the pattern of results was quite similar across all the sets of analyses, and this provides more evidence to the robustness of the findings. The social support measures were developed specifically for the ECA program and were not a standardized social support scale. Moreover, they were self-reports and could not be corroborated by another source. The findings may have varied if a different measurement strategy had been employed. Barriers to care and stigma were also not tested and could be explored in future research. It might be difficult to generalize these findings to other populations across different countries or cultures. Moreover, for the purpose of these analyses, some of the more severe mental disorders, such as schizophrenia, were not included because of low prevalence.
Conclusions
This study is one of the first to examine the association between social network and social support and use of different types of mental health services in a population-based cohort. We differentiated between general medical services, more formal mental health services, and nonformal other human services. Our results indicated that for general medical service use, increased social network or support was associated with increased service use, but increased social support from relatives and friends or higher number of relatives was associated with reduced use of more formal mental health or specialty psychiatric services. In contrast, use of nonformal care may be influenced by having a less dense network of informants.
These findings corroborate existing theories and suggest a need for further investigation of social support and outcomes. More research is needed on the impact of attitudes and knowledge regarding mental health, stigma, access to services, and religious beliefs, in combination with social support measures, to better understand the complex set of factors that influence service use. Although we adjusted for a number of factors, future research should also examine the buffering effect of factors such as gender, age, and insurance on service use.
From a broader public health perspective, information on available social networks can be used to develop or reinforce networks within communities and provide them with accurate information about different mental health conditions, the availability of services, and the benefits of such services. On an individual level, an enhanced knowledge of social support and service use could help case managers to formulate and plan treatment for individuals with psychiatric problems.
Acknowledgments and disclosures
The Baltimore Epidemiologic Catchment Area program was funded by grant MH47447 from the National Institute of Mental Health.
The authors report no competing interests.
1. Demyttenaere K, Bruffaerts R, Posada-Villa J, et al: Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291:2581–2590, 2004Google Scholar
2. Cooper-Patrick L, Gallo JJ, Powe NR, et al: Mental health service utilization by African Americans and whites: the Baltimore Epidemiologic Catchment Area Follow-Up. Medical Care 37:1034–1045, 1999Google Scholar
3. Andersen R: A Behavioral Model of Families' Use of Health Services. Chicago, University of Chicago, Center for Health Administration Studies, 1968Google Scholar
4. Andersen R: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1–10, 1995Google Scholar
5. Pescosolido BA, Boyer CA: How do people come to use mental health services? Current knowledge and changing perspectives; in A Handbook for the Study of Mental Health: Social Context, Theories, and Systems. Edited by Horowitz AV, Scheid TL. Cambridge, United Kingdom, Cambridge University Press, 1999Google Scholar
6. Cobb S: Social support as a moderator of life stress. Psychosomatic Medicine 38:300–314, 1976Google Scholar
7. Vaux A: Social Support: Theory, Research, and Intervention. New York, Praeger, 1988Google Scholar
8. Pilisuk M, Boylan R, Acredolo C: Social support, life stress, and subsequent medical care utilization. Health Psychology 6:273–288, 1987Google Scholar
9. Sherbourne CD: The role of social support and life stress events in use of mental health services. Social Science and Medicine 27:1393–1400, 1988Google Scholar
10. Thoits PA: Self, identity, stress, and mental health; in Handbook of the Sociology of Mental Health. Edited by Aneshensel CS, Phelan JC. New York, Kluwer Academic/Plenum, 1999Google Scholar
11. Turner RJ, Turner JB: Social integration and support; in Handbook of Sociology of Mental Health. Edited by Aneshensel CS, Phelan JC. New York, Kluwer Academic/Plenum, 1999Google Scholar
12. Albert M, Becker T, McCrone P, et al: Social networks and mental health service utilization—a literature review. International Journal of Social Psychiatry 44:248–266, 1998Google Scholar
13. Carpentier N, White D: Cohesion of the primary social network and sustained service use before the first psychiatric hospitalization. Journal of Behavioral Health Services and Research 29:404–418, 2002Google Scholar
14. Kang SH, Wallace NT, Hyun JK, et al: Social networks and their relationship to mental health service use and expenditures among Medicaid beneficiaries. Psychiatric Services 58:689–695, 2007Google Scholar
15. Baltimore Health and Mental Health Survey. Baltimore, Johns Hopkins School of Public Health, Department of Mental Health, 1993Google Scholar
16. Baltimore Health and Mental Health Survey. Baltimore, Johns Hopkins School of Public Health, Department of Mental Health, 2004Google Scholar
17. Shapiro S, Skinner EA, Kessler LG, et al: Utilization of health and mental health services: three Epidemiologic Catchment Area sites. Archives of General Psychiatry 41:971–978, 1984Google Scholar
18. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, rev. Washington DC, American Psychiatric Association, 1987Google Scholar
19. Goldberg DP, Cooper B, Eastwood MR, et al: A standardized psychiatric interview for use in community surveys. British Journal of Preventive and Social Medicine 24:18–23, 1970Google Scholar
20. Liang K-Y, Zeger S: Longitudinal data analysis using generalized linear models. Biometrika 73:13–22, 1986Google Scholar
21. Stata Statistical Software, Release 9.0. Texas, Stata Corp, 2005Google Scholar
22. Pan W: Akaike's information criterion in generalized estimating equations. Biometrics 57:120–125, 2001Google Scholar
23. Cui J, Qian G: Selection of Working Correlation Structure and Best Model in GEE Analyses of Longitudinal Data. Communications in Statistics—Simulation and Computation 36:987–996, 2007Google Scholar
24. Eaton WW, Kalaydjian A, Scharfstein DO, et al: Prevalence and incidence of depressive disorder: the Baltimore ECA follow-up, 1981–2004. Acta Psychiatrica Scandinavica 116:182–188, 2007Google Scholar
25. MaCurdy T, Mroz T, Gritz M: An evaluation of the National Longitudinal Survey on Youth. Journal of Human Resources 33:345–436, 1998Google Scholar
26. National Longitudinal Survey: NLS of Mature Women Cohort User's Guide. Washington, DC, US Department of Labor, 2003. Available at. www.nlsinfo.org/women/docs/gdetext/mw/mch2pt3.htm#twoeight Google Scholar
27. Diggle PJ, Haegerty PJ, Liang K-Y, et al: Missing values in longitudinal data; in Analysis of Longitudinal Data. Edited by Diggle PJ, Haegerty PJ, Liang K-Y, et al. New York, Oxford University Press, 2002Google Scholar
28. Rosenfield S: Labeling mental illness: the effects of received services and perceived stigma on life satisfaction. American Sociological Review 62:660–672, 1997Google Scholar
29. Link B, Castille DM, Stuber J: Stigma and coercion in the context of outpatient treatment for people with mental illnesses. Social Science and Medicine 67:409–419, 2008Google Scholar
30. Golding JM, Wells KB: Social support and use of mental health services by Mexican Americans and non-Hispanic whites. Basic and Applied Social Psychology 11:443–458, 1990Google Scholar
31. Pescosolido BA, Wright ER, Alegría M, et al: Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Medical Care 36:1057–1072, 1998Google Scholar
32. Vogel DL, Wade NG, Wester SR, et al: Seeking help from a mental health professional: the influence of one's social network. Journal of Clinical Psychology 63:233–245, 2007Google Scholar
33. Granovetter MS: The strength of weak ties. American Journal of Sociology 78:1360–1380, 1973Google Scholar
34. Birkel RC, Reppucci ND: Social networks, information-seeking, and the utilization of services. American Journal of Community Psychology 11:185–205, 1983Google Scholar



