Involuntary Admission of Emergency Psychiatric Patients: Report From the Amsterdam Study of Acute Psychiatry
In European countries such as the Netherlands, the number of compulsory (involuntary) psychiatric admissions has been rising since the 1990s ( 1 ). The increase in the Netherlands included both involuntary admissions in emergency situations, ordered by the mayor upon advice from a psychiatrist (emergency compulsory admissions), and involuntary admissions after recourse to the courts (court orders) ( 2 ).
In the Amsterdam area, the number of emergency compulsory admissions rose by 319%, to 86 per 100,000 in the period between 1979 and 2004 ( 3 ). These developments suggest that patients with severe mental illnesses more often progress to stages in which acute, coercive treatment is warranted. It is clear that this is an undesirable trend, resulting in negative experiences for the patients and a reduction of patient autonomy. This observation should be viewed in the context of the fact that data about potential long-term effects of compulsory admission are still scarce ( 4 ).
In this first part of our Amsterdam Study of Acute Psychiatry (ASAP-I) study ( 5 ), our goal was to determine which factors are associated with emergency compulsory admissions. On the basis of previous research, we expected emergency compulsory admissions to be predicted by critical combinations of schizophrenia ( DSM-IV-TR ) or another psychotic disorder and a previous compulsory admission on the one hand and severity of psychiatric symptoms, lack of motivation for treatment, and being a danger to oneself or others on the other hand. We also expected that police involvement in referring persons to emergency services, in contrast to referral by primary health care, indicates a high risk of emergency compulsory admission.
Methods
This study was part of a prospective cohort study consisting of all consecutive emergency consultations from the Psychiatric Emergency Service Amsterdam (PESA) between September 15, 2004, and September 15, 2006 ( 5 ). PESA covers a catchment area of 743,000 inhabitants and provides a citywide, 24-hour psychiatric emergency service seven days a week. Patients are referred by family physicians, the police, emergency departments of general hospitals, and mental health care workers. Persons who come into contact with the police are first screened by a community mental health nurse from the City Health Service. Patients needing psychiatric consultation are taken to the PESA premises by the police. They were classified as "referred by the police." If patients are referred to the PESA by primary health care providers such as family physicians or emergency doctors, they are often seen in their homes or at the referring hospital. In general, consultations are on work days between 9 a.m. and 10 p.m., with resident physicians working with community mental health nurses. Psychiatrists work in the emergency room, either as supervisors or by seeing patients themselves. At other times, residents and nurses work together, with psychiatrists as telephone back-up. The PESA uses electronic patient files.
From the cohort of consultations that took place during the study period, we selected the first consultation of every patient. Only patients with a fixed abode in Amsterdam were studied, because reliable and comparable data on psychiatric history can be derived from the Amsterdam Mental Health Care Registration Database used by the mental health care services in the Amsterdam catchment area. Our study of the consultations was based exclusively on a completed form using the Severity of Psychiatric Illness rating scale (SPI) ( 6 ).
We found 3,247 first consultations during the study period. We excluded tourists (N=188, 6%), people living elsewhere in the Netherlands (N=339, 10%), people with no known place of residence (N=227, 8%), patients who already had a court order for involuntary admission at the time of the consultation (N=41, 1%), consultations with a missing outcome decision (N=83, 3%), and consultations without a completed SPI form (N=399, 19%), leaving a study cohort of 1,970 consultations. Of the 399 consultations for which no SPI form was completed, this omission occurred in 95% of these consultations (N=379) because the emergency officers conducting the consultation had not yet completed SPI training. New staff workers at the PESA were not always able to complete SPI training immediately after being appointed and sometimes completed training only after conducting a number of consultations.
We divided the variables into two groups. The first group included patient characteristics, contextual characteristics, previous health care use, and diagnostic category, which were classified as independent variables. The second group consisted of SPI scores, which reflect the considerations of the clinician during the emergency consultation. These were considered intermediating variables because they were closely connected with the outcome measure.
The patient characteristics we collected were age, gender, and domestic (living) situation. We registered each patient's referring professional and the DSM-IV-TR ( 7 ) psychiatric diagnosis, which was placed in one of four main categories: schizophrenia and other psychotic disorders (psychotic disorder), manic state, depressive disorder, and other or no disorders. The last category contained a vast group of diagnostic categories and psychosocial problems without a DSM axis I disorder.
For recording the severity of the psychopathology, we used the SPI, which includes 14 items scored on a 4-point scale. In our analysis we used the following five items: suicide risk, danger to others, severity of psychiatric symptoms, lack of motivation for treatment, and awareness of illness. We chose these five items because other Dutch studies have indicated that these SPI items predicted compulsory admission ( 8 ). The instrument has been validated in several studies ( 6 ). Behavioral descriptors in the SPI manual anchor the ratings. The PESA personnel were trained to use the SPI according to the manual ( 9 ).
Information about psychiatric history was obtained from the Amsterdam Mental Health Care database. We recorded the number, type, and duration of inpatient treatments and outpatient contacts over five years, one year, and one month preceding emergency consultation. We used SPSS, version 17.0 ( 10 ), to allocate the consultations on the basis of the number of outpatient contacts to groups with the same size or as close as possible. This resulted, for the contacts during the year before the emergency consultation (excluding the last month), in three values: no contacts, one to 14 contacts, and >14 contacts. For the contacts in the month before the emergency consultation, the values were no contacts, one to three contacts, and more than three contacts.
We divided the study cohort into three groups according to the intervention resulting from the consultation: compulsory admission, voluntary admission to a psychiatric hospital or a crisis center, and no admission.
This study was endorsed by the Medical Ethics Committee for Mental Health Care Institutions ( 5 ). All data were obtained from the electronic patient files of the PESA and from the Amsterdam Mental Health Care database. Bivariate analyses with chi squares and analyses of variance with t tests were used to examine differences in demographic, clinical, and contextual variables and in SPI scores between the three groups of patients. Because we expected the patients with no admissions to contain a high percentage of patients from the diagnostic category "other or no disorder," we decided to conduct the multivariate logistic regression analyses only for the cohort of admitted patients. The multivariate analysis examined the association between the independent variables and the outcome variable (step 1) and between the independent variables and SPI scores and the outcome variable (step 2). We entered into the multivariate analysis only the variables that showed a significant difference in the univariate analyses (not shown).
Results
The study cohort of 1,970 consultations was compared with 399 consultations done without the SPI. Variables included gender, average age, domestic situation, source of referral, psychiatric diagnosis, psychiatric history, and outcome of the consultation. There were no significant differences in demographic variables, diagnostic category, or average number of outpatient contacts in the year before the consultation; the average numbers of voluntary and compulsory admissions in the previous five years; and outcome of the consultation.
Of the 1,970 patients, 352 (18%) were admitted compulsorily and 408 (21%) were admitted voluntarily (univariate analyses not shown). Ambulatory treatment or no treatment at all was prescribed for 1,205 patients (61%). The mean±SD age of the voluntarily admitted group was 43.5±14.3 and that of the compulsorily admitted group was 41.8±15.9, a nonsignificant difference. Men were more often compulsorily admitted than women (214 of 1,054, or 21%, and 138 of 920, or 15%, respectively; p≤.01). Men also were referred with a psychotic disorder significantly more frequently than were women (482 of 1,054, or 46%, and 301 of 920, or 32%, respectively, p≤.001) and were more often referred by the police (515 of 1,054, or 49%, and 346 of 920, or 38%, respectively, p≤.001).
According to our Mental Health Care database, 45% (N=887) of the patients had had no treatment contact in the previous year, whether outpatient or inpatient. This was true for 38% (N=134) of the compulsorily admitted group. A group of 467 patients (24%) had had more than 14 outpatient contacts that year (excluding the last month), with a mean frequency of 39±35 contacts. A total of 74 (21%) of the involuntary admitted group had had one or more involuntary admissions within the five previous years, as opposed to 29 of 401 persons (7%) in the voluntarily admitted group (p≤.001).
The two-step logistic regression analysis of the cohort with voluntary and compulsory admissions (N=763) showed that gender and age had no independent influence on the risk of compulsory admission ( Table 1 ). However, living with parents raised the risk more than threefold. This link persisted when analyses controlled for the SPI scores (step 2). Police referral and referral by mental health care raised this risk significantly, even when step 2 controlled for the SPI scores. Patients with more than 14 outpatient contacts in the previous year were found to have a lower risk of compulsory admission. Involuntary admission within the five previous years raised the risk almost fourfold when step 2 controlled for the SPI scores. The strongest predictors were the SPI scores for the items on danger to others and lack of motivation for treatment. The items on suicide risk, severity of symptoms, and lack of awareness of illness did not show significant associations with involuntary admission.
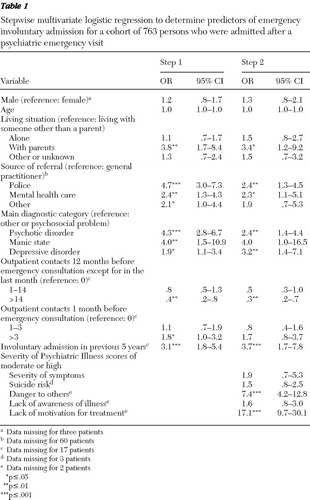 |
In this step 2 prediction model, Cox and Snell R 2 was .502, accounting for 50% of the variance.
Discussion
Other studies have shown that previous compulsory admissions are associated with an almost fourfold increase in the risk of compulsory admissions ( 11 ). However, a striking finding of our study is that this increased risk was independent of the clinician's appraisal of the severity of the disorder, the risk of danger to self or others, and treatment compliance at the time of emergency consultation (SPI scores). It would appear that, all other things being equal, physicians were more inclined to decide on compulsory admission for patients with a history of compulsory admission than for those without. Moreover, again all other things being equal, patients who received more intensive outpatient treatment in the year before the consultation were less likely to have an emergency compulsory admission. This finding may indicate a viable avenue to curb the rising levels of compulsory admission and prevent the harm done to fruitful long-term working alliances with these often hard-to-treat patients. However, we cannot completely rule out that, apart from health service characteristics, patient factors may have also played a role in the success of outpatient interventions in an earlier phase of illness.
The finding that referral by a general practitioner was linked to the lowest likelihood of a compulsory admission compared with referral by the police concurs with previous research in the United Kingdom ( 12 ). Of course, the calmer and more cooperative patients are more likely to be selectively referred through first-line facilities. It was already known that police referrals often precede compulsory admissions ( 13 ). The increased risk associated with referral by the police or mental health care was independent of the SPI scores. Patients with equally high SPI scores were more likely to be compulsorily admitted after a mental health care or police referral. The emergency physician apparently saw these referral routes as an independent and additional reason to decide to proceed with a compulsory admission. It may be more difficult for them to turn down a request from the police or their colleagues in mental health care to intervene in a situation and thus compulsorily admit the patient. We suspect that an additional factor here is that patients referred by family physicians are often examined at home, where the prevention of danger by calling in social support has a greater chance of success.
When analyses controlled for the SPI scores, specific diagnostic categories (psychotic disorder and depressive disorder) had an effect on the likelihood of compulsory admission. However, as expected, the effect of a psychotic disorder was mediated by SPI scores, indicating that severity of the disorder and imminent danger accompanying the psychosis were the most important drivers of compulsory admission. Corroborating this was the fact that high scores for the SPI variables danger to others and lack of motivation for treatment were the strongest predictors of compulsory admission. These variables correspond to the five conditions set out by the legal requirements for emergency compulsory admissions in the Netherlands: a diagnosed psychiatric disorder, imminent danger to self or to others, a causal link between the disorder and the danger, refusal of treatment, and the compulsory admission is a last-resort measure to fend off the danger the person poses. In other words, although diagnosis and previous history make a unique contribution to decision making, the emergency physicians make a decision in accordance with the statutory provisions.
This study has several limitations. We did not use a standardized assessment instrument for generating a psychiatric diagnosis; the diagnosis was based on a clinical interview as performed in day-to-day practice. The emergency setting precluded the use of a standardized assessment tool. Another limitation was the fact that the SPI questionnaire was filled out by the clinician. This generates some unreliability, especially if one considers the possibility that the emergency physician may have completed the SPI form after making the decision to commit the patient. The strengths of this study in comparison with other studies are its setting (actual emergency psychiatry), the large study cohort, the duration of the observation period, the prospective design, and the use of a large mental health care database for psychiatric history data.
Conclusions
Given the steadily rising rates of compulsory admission and the damage this may do in terms of negative experiences for the patients and a reduction of patient autonomy, it is perhaps comforting to see that the complex decision involved in emergency compulsory admission is largely driven by the right incentives. However, specific diagnostic groups, origin of referral, and previous involuntary admission made independent contributions to the likelihood of compulsory admission. More important with respect to opportunities to curb involuntary admission is the finding that more intensive psychiatric treatment preceding an emergency consultation was significantly associated with a lower risk of compulsory admission. To test the hypothesis that outpatient treatment indeed has a preventive effect on compulsory admission, intervention studies are a necessary next step.
Acknowledgments and disclosures
The authors thank ARKIN Mental Health Care, Amsterdam, the Netherlands, for financial support, and the emergency psychiatric clinicians of PESA for their participation in the study.
The authors report no competing interests.
1. De Stefano A, Ducci G: Involuntary admission and compulsory treatment in Europe. International Journal of Mental Health 37:10–21, 2008Google Scholar
2. Mulder CL, Broer J, Uitenbroek D, et al: Accelerated increase in the number of involuntary admissions following the implementation of the Dutch Act on Compulsory Admission to Psychiatric Hospitals (BOPZ) [in Dutch]. Nederland Tijdschrift voor Geneeskunde 150:319–322, 2006Google Scholar
3. BOPZIS: BOPZ registratiesysteem (data file). Utrecht, Netherlands, Inspectie Geestelijke Gezondheidszorg, 2006Google Scholar
4. Kallert TW, Glockner M, Schutzwohl M: Involuntary vs voluntary hospital admission. European Archives of Psychiatry and Clinical Neurosciences 258:195–209, 2008Google Scholar
5. Post LVD, Schoevers R, Koppelmans V, et al: The Amsterdam Studies of Acute Psychiatry I (ASAP-I): a prospective cohort study of determinants and outcome of coercive versus voluntary treatment interventions in a metropolitan area. BMC Psychiatry 8:35, 2008Google Scholar
6. Lyons JS, Colletta J, Devens M, et al: Validity of the Severity of Psychiatric Illness rating scale in a sample of inpatients on a psychogeriatric unit. International Journal of Psychogeriatrics 7:407–416, 1995Google Scholar
7. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision. Washington DC, American Psychiatric Association, 2000Google Scholar
8. Mulder CL, Koopmans G, Lyons JS: Determinants of indicated versus actual level of care in mobile psychiatric emergency services. Psychiatric Services 56:452–457, 2005Google Scholar
9. Lyons JS: The Severity and Acuity of Psychiatric Illness Scales: An Outcomes Management and Decision Support System. Adult Version. Manual. San Antonio, Tex, Harcourt Brace, 1998Google Scholar
10. SPSS, version 17.0. Chicago, SPSS, 2008Google Scholar
11. Fennig S, Rabinowitz J, Fennig S: Involuntary first admission of patients with schizophrenia as a predictor of future admissions. Psychiatric Services 50:1049–1052, 1999Google Scholar
12. Szmukler GI: Compulsory admissions in a London borough: II. circumstances surrounding admission: service implications. Psychological Medicine 11:825–838, 1981Google Scholar
13. Cougnard A, Kalmi E, Desage A, et al: Pathways to care of first-admitted subjects with psychosis in south-western France. Social Psychiatry and Psychiatric Epidemiology 39:804–809, 2004Google Scholar



