Population-Based Service Planning for Implementation of MBCT: Linking Epidemiologic Data to Practice
Mindfulness-based cognitive therapy (MBCT) is a group-based intervention designed to reduce rates of relapse of major depressive disorder. Preliminary evidence for the efficacy of MBCT derives from two randomized controlled trials ( 1 , 2 ), but the evidence is most convincing for people having had three or more episodes. If we take this as a restriction on eligibility for MBCT, then estimating the proportion of the population who could benefit from the treatment would be valuable for planning purposes.
For this study we used epidemiologic data and a simulation model to estimate the proportion of a population that could benefit from MBCT and to determine the practicality of implementing the treatment in populations of various sizes, such as catchment areas or health regions. We also explored the role of acceptability of this treatment as a determinant of human resource needs.
Methods
We used the Public Use Microdata File from the Canadian Community Health Survey, Mental Health and Wellbeing (CCHS 1.2). The survey has been described in detail elsewhere ( 3 ). In brief, the CCHS 1.2 was a national survey conducted in Canada in 2002. The target population consisted of persons aged 15 or older living in private dwellings (98% of the population). One eligible resident was randomly selected from sampled households. The overall response rate was 77%, which yielded a sample of 36,984 respondents.
The CCHS 1.2 used a Canadian adaptation of the World Mental Health Composite International Diagnostic Interview ( 4 ). Trained lay interviewers administered the survey. Data collection by telephone was authorized only when travel costs were prohibitive or the respondent refused to conduct the interview in person. Ultimately, 14% of interviews were completed by telephone.
Sampling weights were used to adjust for design effects, and confidence intervals (CIs) were calculated from approximate coefficient of variation tables provided by Statistics Canada. Because the estimates are weighted, the estimated proportions reported here may differ slightly from direct frequency calculations. Eligibility for MBCT—defined as the occurrence of three or more past episodes of major depression—was directly estimated from the survey data.
In general, incidence estimates cannot be calculated from cross-sectional data. To establish an approximate value for this parameter, we used a simulation model. The modeling used a discrete-event simulation approach and was carried out in Arena, version 10 ( 5 ). [A detailed description of this model and its development is available as an online supplement to this brief report at ps.psychiatryonline.org .]
Results
The CCHS sample included 16,773 men (45.4%) and 20,211 women (54.6%). There were 4,713 respondents (12.7%; weighted frequency, 12.2%) with a lifetime major depressive episode. Of these, 539 (11.4%) reported a lifetime manic episode. Exclusion of the latter respondents led to a weighted lifetime prevalence estimate of 11.0% (95% CI=10.4%–11.5%), 13.8% for women and 8.1% for men. The weighted frequency distributions of past episodes were as follows: one episode, 43.8%; two episodes, 15.9%; three episodes, 11.0%; four episodes, 5.8%; five or more episodes, 23.5%.
Among the 4,174 respondents with past episodes, 1,628 reported three or more episodes (weighted percentage, 40.3%; 95% CI=37.8%–42.9%). These respondents represented 4.2% (95% CI=3.9%–4.5%) of the Canadian population. The weighted proportions were similar among men (38.2%; 95% CI=33.9%–42.4%) and women (41.6%; 95% CI=38.7%–44.5%). Slightly more than half of the respondents with three or more episodes reported an episode during the preceding year (2.3% of the population).
The simulation model was able to reproduce the observed pattern of current and lifetime prevalence, as well as the pattern of episode duration and number of reported episodes. [Data from the model are available in the online supplement available at ps.psychiatryonline.org .] With the simulation model running in a steady-state situation, we collected data on the number of individuals in remission after a second episode who would experience a third episode, reflecting the rate at which new candidates for MBCT would emerge in the population. According to the model this rate was 13 per 10,000 per year.
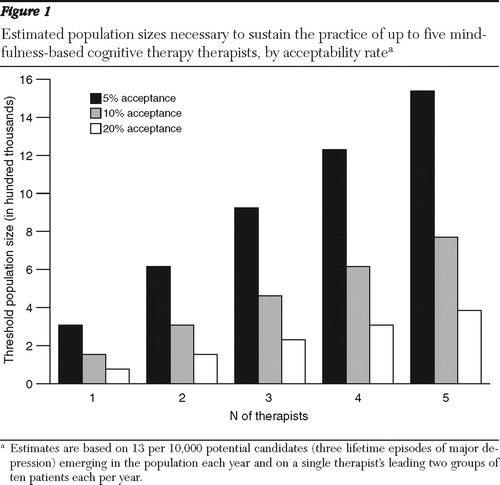
Clinical experience with MBCT suggests that a practitioner needs to lead at least two groups a year to maintain an adequate level of skill. An MBCT group typically includes ten participants. Therefore, approximately 20 patients per year are needed to sustain the activities of a therapist. Figure 1 presents threshold population sizes expected to generate 20 or more clients per therapist on the basis of 13 newly eligible individuals per 10,000 per year. Estimates were made for up to five therapists and for three rates of acceptability of this treatment to eligible persons (5%, 10%, and 20%). A catchment area of 200,000 could support two therapists if at least 20% of eligible individuals accepted MBCT; however, at a 5% acceptance rate, the same population could not support one therapist.
Discussion
The goal of this study was not to determine the efficacy or effectiveness of MBCT or to advocate for its implementation. The purpose was to explore planning issues that arise with implementation of new interventions by using MBCT as a case in point. The idea that the treatment is efficacious for an identifiable subset of the population was taken as a starting point for our analyses.
Our estimates indicate that a large segment of the Canadian population—4.2%—is eligible for MBCT on the basis of having experienced three or more lifetime episodes of major depressive disorder. It may be more realistic to consider a subset of this group as initially eligible—those who have had an episode during the past year (2.3%). A population health strategy designed to deliver MBCT would therefore initially encounter a large number of potentially eligible individuals. Theoretically, if 100% of eligible individuals found MBCT acceptable, then even a small population of 500 people could support one therapist for one year (.042×500=21). Over time, as the extent of the eligible and accepting population pool diminishes, the demand for the treatment would be more closely related to the rate of emerging eligibility in the population—approximately 13 per 10,000 per year.
MBCT requires a substantial degree of commitment, including regular meditation. Plainly it will not appeal to all eligible candidates, but we have no systematic estimates of its acceptability. The analyses presented here indicate that estimating the acceptability rate is a key question for planning purposes. If the acceptability rate is low, then only clinics or programs with large catchment areas would be able to support delivery. The results suggest that MBCT may more readily be implemented in the established group format within metropolitan areas, outside of which guided work with self-help materials ( 6 ) or other delivery options may be needed.
Limitations of this study include reliance on a simulation model rather than direct estimation from longitudinal data. Also, the results may be biased by nonresponse or survey participants' failure to recall past episodes of major depressive disorder. These two limitations are not separate from one another. If the frequency of past episodes is underestimated in cross-sectional surveys, which is plausible ( 7 ), the simulated recurrence rates may be too low. In this case, smaller populations than those identified in Figure 1 may be able to sustain MBCT therapists. A related issue concerns persistence of clients in therapy. Although MBCT is a time-limited therapy, some clients may be offered supplemental sessions or repeat courses over longer periods. For this reason, a population of a given size may sustain more therapists than our results suggest. In addition, results of MBCT trials may not be generalizable to the general population. Randomized controlled trials apply exclusion criteria that may result in selection of trial participants' having a more favorable prognosis. It is possible that the real-world effectiveness of MBCT is limited to a subset of apparently eligible candidates within the population. Implementation of MBCT would in such circumstances require larger catchment areas or higher rates of acceptability. Finally, because our estimates are based on a Canadian survey that found a prevalence lower than those of the National Comorbidity Survey Replication ( 8 ), the results cannot necessarily be generalized to the U.S. population.
With advances in therapeutics, it is reasonable to expect that recurrence patterns of major depression will change, which would result in diminished prevalence over time. Therefore, epidemiologic estimates and model parameters may change. Ongoing epidemiologic surveillance is needed to inform estimates and models. A simulation model such as the one presented here provides a framework that can be updated with new epidemiologic data.
Conclusions
Epidemiologic data and simulation results indicate that the number of MBCT therapists needed in a population strongly depends on whether the treatment is introduced for an existing pool of eligible respondents or targeted to newly emerging candidates. The acceptability of MBCT is also a critical issue. The study presents techniques that may be broadly useful for linking service planning to epidemiologic data.
Acknowledgments and disclosures
The analysis was based on data from a survey conducted by Statistics Canada. However, the results do not represent the opinions of Statistics Canada.
The authors report no competing interests.
1. Teasdale JD, Segal ZV, Williams JM, et al: Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology 68:615–623, 2000Google Scholar
2. Ma SH, Teasdale JD: Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology 72:31–40, 2004Google Scholar
3. Gravel R, Béland Y: The Canadian Community Health Survey: mental health and well-being. Canadian Journal of Psychiatry 50:573–579, 2005Google Scholar
4. Kessler RC, Ustun TB: The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research 13:83–121, 2004Google Scholar
5. Arena, Version 10. Sewickley, Penn, Rockwell Software, 2006Google Scholar
6. Williams M, Teasdale J, Segal Z, et al: The Mindful Way Through Depression: Freeing Yourself From Chronic Unhappiness. New York, Guilford, 2007Google Scholar
7. Andrews G, Anstey K, Brodaty H, et al: Recall of depressive episode 25 years previously. Psychological Medicine 29:787–791, 1999Google Scholar
8. Kessler RC, Berglund P, Demler O, et al: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289:3095–3105, 2003Google Scholar



