Integrated Care for Co-occurring Disorders: Psychiatric Symptoms, Social Functioning, and Service Costs at 18 Months
Excessive consumption of alcohol and use of psychoactive substances among patients with severe mental illness are of increasing concern worldwide. Estimates from surveys of clinic populations in Britain suggest that as many as a third of patients with severe schizophrenia and other psychoses also abuse alcohol and that 16%–20% have problems with abuse of or dependency on illicit drugs ( 1 , 2 , 3 , 4 ). Patients with these comorbid conditions experience more severe symptoms of illness and higher rates of relapse ( 5 , 6 ), aggressive behavior ( 7 ), and suicidal thoughts and actions ( 8 ). Health care costs are among the highest for any psychiatric disorder ( 9 ).
Although there is widespread agreement that people with co-occurring disorders constitute a very needy population, there is also considerable pessimism about the efficacy of treatment. Typical programs that involve sequential or parallel efforts to manage the mental disorder and the substance use disorder are generally regarded as ineffective ( 10 ), leading to calls for integrated approaches in which management of both types of disorder is provided by a single service that brings together some of the techniques and skills of motivational interventions to reduce substance abuse with medical and psychological interventions for the management of psychotic symptoms ( 11 ). Some evidence has been found for the superiority of such integrated treatment compared with sequential or parallel approaches. However, this evidence is drawn from comparisons with "usual care" rather than by direct head-to-head comparison with either alternative implemented to a quality standard. A meta-analysis concluded that methodological weaknesses of existing studies mean that no firm conclusions can be drawn ( 12 ). Since this meta-analysis was published, three interventions involving treatment provided by expert therapists have been reported ( 13 , 14 , 15 ), although the generalizability of such intensive interventions to routine settings is yet to be determined.
In summary, there is at least a prime facie case for integrated treatment approaches, and these are, indeed, national policy in England ( 16 ). In the study presented here, we set out to investigate whether case managers on community mental health teams could be trained to deliver an effective intervention for patients with severe mental illness and a comorbid substance use disorder. In a previous article we reported that the intervention was no more effective than conventional community treatment, with both groups showing some reduction in substance use ( 17 ). This article reports the findings of the secondary study outcomes of psychiatric disorder, social functioning, quality of life, satisfaction with services, and service costs.
This study tested the hypotheses that compared with patients who received standard care, patients who received the intervention would report a reduction in the severity of psychiatric symptoms and improved social functioning, quality of life, and satisfaction with services. We also hypothesized that they would have lower service costs.
Methods
Study context and design
The study was conducted in community mental health services in the London boroughs of Southwark, Lewisham, Lambeth, and Croydon. These boroughs constitute a socially deprived and ethnically diverse inner-city area of London, with a population of some 1.5 million adults of working age. All mental health services for the boroughs are provided by a single organization, the South London and Maudsley National Health Service Trust. Community mental health services are provided through well-established multidisciplinary teams, each serving a geographically defined sector and providing assessment and continuing care to all adults with severe mental illness between the ages of 18 and 65 years. All British community mental health teams provide clinical care for severe mental illness through clinical case managers who come from a variety of professional backgrounds; most case managers are from the nursing field, but the group also includes social workers and occupational therapists. The case managers provide counseling, monitor mental state, supervise medication, and arrange and coordinate a variety of interventions, such as assistance with daily living tasks, housing, and finances. On average, there were seven case managers on each of the teams studied; the number varied according to the size of the patient population served by that team. All teams also include psychiatrists and access to clinical psychologists. Although many case managers have had some training in substance use disorders as part of their general professional education, the usual management of substance abuse at the time of the study was by referral to a separate substance dependency service, and there were no substance abuse specialists on the teams.
Approval for the study was obtained from the relevant research ethics committees. The study was carried out between 1999 and 2003. It employed a cluster-randomized controlled trial design with clinical case managers as the units of randomization. The process of recruitment was as follows: the clinical records of all patients known to case managers were first examined to identify patients with a clinical diagnosis of schizophrenia, schizoaffective disorder, or other nonaffective psychotic illness ( ICD-10 codes F20–F29) or bipolar affective disorder with psychotic symptoms (F31). These patients were then screened for substance use by using the Clinician Alcohol and Drug Use Scales ( 18 ). All patients who met both the ICD-10 diagnostic criteria and the screening criteria for abuse of or dependence on at least one substance were included in the trial. After research ethics approval was obtained for the study, case managers from each team were randomly allocated by an independent statistician to the experimental or control condition; patients with co-occurring disorders were automatically assigned to their case manager's group.
The experimental intervention. The experimental intervention comprised training and supervision of case managers in the assessment and management of co-occurring disorders. The training was developed from a well-established course run at the Institute of Psychiatry based on a four-stage model—engagement, building motivation, active treatment, and relapse prevention—that draws upon elements of motivational interviewing and cognitive-behavioral strategies ( 19 , 20 ). The training for case managers covered basic drug and alcohol awareness (symptoms, signs, patterns of use, effects, and so forth), comprehensive assessment, motivational strategies, management of resistance, problem solving, active treatment options, and relapse prevention. Using role play, case managers worked through a series of motivational interviewing techniques and principles, including decisional balance, readiness to change, goals, and roadblocks. They were encouraged to consider the motivational states of their clients and tailor their therapeutic responses accordingly. These techniques were modified for use with people with severe mental illness by an emphasis on providing a simple and clear introduction to each therapy session in the form of an agenda, as well as an emphasis on the importance of repetition and paraphrasing, written records for the service user to keep, reminders about what had been discussed, and keeping the pace of therapy appropriate to the needs of the person. The trainees presented a current case in order to link the course content to practice and unite all the themes.
The training was delivered one day a week for five weeks. An instruction manual for therapy was provided that contained detailed descriptions of the interventions and further reading on each topic. After completing the course, case managers received an hour of supervision with the trainer each week for all 18 months of the study. Supervision was focused on each case manager's patients with co-occurring disorders and on reviewing ongoing therapy and rehearsing and monitoring interventions. The supervision provided both "top-up" training and a check on the implementation of the intervention.
The comparison intervention. The intervention group was compared with a group that received standard care with no specific support or supervision. Although case managers in the comparison arm of the study did not receive specialist training or supervision, they were all experienced clinicians and were not discouraged from following good practice guidelines or from setting goals involving patients' substance misuse. Precautions were taken to minimize contamination of information between experimental and control staff by asking them not to share details of the training and by avoiding the transfer of patients between case managers in the two arms of the trial.
Measures
Research staff who were independent of the intervention gathered data from hospital records, interviews with patients, and interviews with case managers.
Symptoms of mental illness were measured by using the extended version of the Brief Psychiatric Rating Scale (BPRS) ( 21 ). We report BPRS total scores and scores for subscales that were based on a factor analysis of the BPRS in a homeless dual-diagnosis population ( 22 ).
Drug and alcohol consumption and associated problems during the past month were assessed by use of the Maudsley Addiction Profile ( 23 ), the Alcohol Use Disorders Identification Test ( 24 ), and the Dartmouth Assessment of Lifestyle Instrument ( 25 ). Quality of life was assessed by the Manchester Short Assessment of Quality of Life ( 26 ). Service satisfaction was measured by the Client Satisfaction Questionnaire ( 27 ) and the Treatment Perceptions Questionnaire ( 28 ). Social functioning was measured with the Life Skills Profile ( 29 ). Need for care was assessed by use of the Camberwell Assessment of Need Short Assessment Schedule ( 30 ).
These measures were repeated at the 18-month follow-up. It was not feasible to conceal from research staff the group allocation of case managers and their patients.
The Client Service Receipt Inventory ( 31 ) was used to collect service use data for the six months before baseline and the 18-month follow-up period. Inpatient data were collected for the 18 months before both interviews. Service costs, including costs related to health care, criminal justice involvement, and incarceration, were calculated by combining the service use data with nationally applicable unit cost information where this was available. Total costs were calculated by multiplying six-month costs by three and adding this sum to the inpatient costs.
Analysis
The study design was a cluster-randomized controlled trial. The sample size was calculated on the basis of minimum clinically important changes in three outcomes using a 5% significance level and 80% power: first, a 30% reduction in bed-days based on a previously determined mean of 45±30 days; second, a reduction from 80% to 60% in the fraction of patients who were still abusing alcohol or drugs at follow-up; and third, an increase of .5±1.3 in the mean compliance score of patients receiving the intervention. (Possible scores on the compliance measure range from 1 to 7, with higher scores indicating better compliance.) The pre-post correlation was assumed to be .5, the intraclass correlation within case managers was assumed to be .02 (design effect of 1.08 for five patients per case manager), and the dropout rate was assumed to be 20%. On the basis of these measures, the largest sample size of 44 key workers and 220 patients was adopted. In practice, the number of patients recruited was 235, and they were associated with 79 case managers.
The analysis was carried out using Stata 8.0 ( 32 ). Estimates of intervention effects on all outcome scores were obtained by linear regression analyses by using the relevant baseline score as a covariate and robust standard errors to adjust for the effect of clustering on case managers (that is, to adjust for the fact that patients were "nested" within the case managers). For total service costs, the difference between the two groups was tested for significance with use of a bootstrapped regression model.
Results
A total of 79 case managers participated in the study. Two worked part-time and shared a single position, and they were randomly assigned to a condition as a single unit. Forty case managers were randomly assigned to the experimental group, and 39 were assigned to the comparison condition. Case managers in this study were typical of those found on most English community mental health teams. They came predominantly from a nursing background (50 of 79, or 63%). A third of the case managers held a degree-level qualification (that is, beyond the equivalent of a bachelor's degree). Half were women (39 case managers, or 49%), and 47 (59%) had been qualified for five years or more. All had experience working with patients with severe mental illness, and a third had received some previous training in managing substance use disorders.
Only 72 of the 128 patients in the intervention group (57%) and 72 of the 105 patients in the comparison group (68%) retained contact with the same case manager throughout the study. New case managers who replaced intervention staff were provided with the same training and joined existing trainees for ongoing supervision.
There were 1,560 patients on the case managers' caseloads, of whom 1,271 had a diagnosis of a psychotic illness and 236 met criteria for co-occurring disorders. Three patients were excluded at this stage because their care was shared by two case managers who had been randomly assigned to different groups, and one patient in the intervention group was excluded because he had been mistakenly identified as meeting the inclusion criteria. Of the remaining 232 patients, 127 were with case managers in the experimental condition and 105 patients were on the caseloads of case managers in the control group.
At the 18-month follow-up, two patients from the experimental group and one from the control group had died. Of the remaining patients, 84 in the experimental group and 75 in the control group were still in regular contact with the original team, 12 patients in the experimental group and ten in the control group had been transferred to another team, and 18 in the experimental group and 15 in the control group had been discharged. We were unable to trace the whereabouts of 16 patients (nine in the experimental group and seven in the control group). Follow-up outcome information from case notes was available for 113 patients in the experimental group (98%) and 98 patients in the control group (93%). Interview-based assessments, which constituted the bulk of data in this report, were available for 77 patients in the experimental group (62%) and 77 patients in the control group (74%).
Details of the classification and patterns of substance use have been published elsewhere ( 33 ). Most patients were men (110, or 87%, in the experimental group and 85, or 81%, in the control group). Most patients were single (109, or 86%, in the experimental group and 87, or 83%, in the control group), and most were unemployed (119, or 94%, in the experimental group and 97, or 93%, in the control group). Self-reported ethnicity of patients in the intervention group were white (United Kingdom or Ireland), 55 patients (43%); black (African, Caribbean, or British), 57 patients (45%); Asian (Indian, Pakistani, or Chinese), four patients (3%); and other, 11 patients (9%). For patients in the control group the figures were white, 64 patients (61%); black, 34 patients (32%); Asian, four patients (4%); and other, three patients (3%). A majority had a main diagnosis of schizophrenia, schizoaffective disorder, or delusional disorder (113, or 89%, in the experimental group and 95, or 90%, in the control group). Most also had a lengthy history of contact with mental health services; more than 70% of all patients had had contact for more than five years.
The two groups of patients were very closely balanced in terms of these demographic criteria, with the exception that fewer participants in the experimental group were from a white ethnic background. Among these 232 patients with co-occurring disorders, the most commonly used substances of abuse were alcohol and cannabis (alcohol only, 77 patients, or 33%; cannabis only, 52 patients, or 22%; both, 29 patients, or 13%; stimulants, 55 patients, or 24%; all other drugs, 19 patients, or 8%).
Adverse events
Violent and severe threatening behavior to others (defined as threatening with a weapon or making repeated threats to kill or severely harm) were reported by a quarter of the patients. Acts of violence were sufficiently severe for the victims to require hospital inpatient care in one case in the control group and two cases in the experimental group.
At the follow-up assessment, four patients in the control group and three in the experimental group reported that they had harmed themselves since the initial assessment. Two participants in the control group made an attempt of sufficient severity for them to require general hospital admission.
Rates of homelessness in each group were substantial; 23 patients (22%) in the intervention group and 14 patients (14%) in the control group had at least one episode of homelessness lasting a month or longer.
Clinical outcomes, satisfaction, and health service costs
Alcohol consumption fell from a mean±SD of 4.8±7.2 units a day at baseline to 3.5±5.6 units a day at follow-up in the experimental group and from 7.2±16.6 to 4.4±7.4 units a day in the control group. However, the reductions in alcohol use were not statistically significant. For cannabis and other drugs, data on amounts consumed were collected and converted to a total monetary value on the basis of current street values of each drug in South London at the time of the study, as estimated by a local drug treatment service. Differences between the two groups in cannabis use were not statistically significant. Monthly costs for drugs other than cannabis fell from £144±1,023 to £33±154 in the experimental group and rose from £110±333 to £124±470 in the control group, but these differences between groups in monthly costs were not statistically significant.
Although the reduction in substance use was not significant at follow-up, patients in the experimental group had significantly lower BPRS scores at follow-up than did participants in the comparison group ( Table 1 ). The significant difference was observed for psychotic symptoms and for symptoms of anxiety and depression, and the difference remained statistically significant after the analysis adjusted for baseline values. As noted, the ethnic background of the two patient groups differed at baseline; however, including this as a further covariate in the regression model made little difference in the results. Even in this analysis, the intervention group continued to have significantly lower symptom scores than the comparison group ( β =-3.7, 95% confidence interval [CI]=-6.8 to -.65).
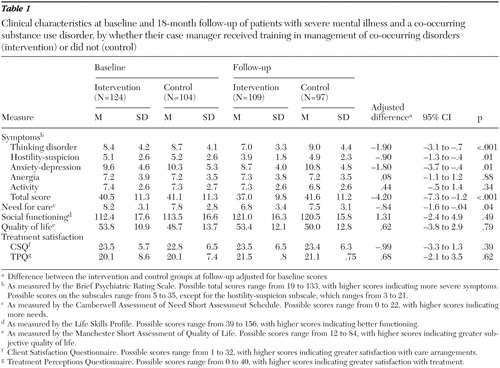 |
Although patients in the intervention group reported fewer unmet needs for care at follow-up, no differences between groups were found in terms of case managers' assessments of social functioning. In both groups most patients reported moderate satisfaction with care.
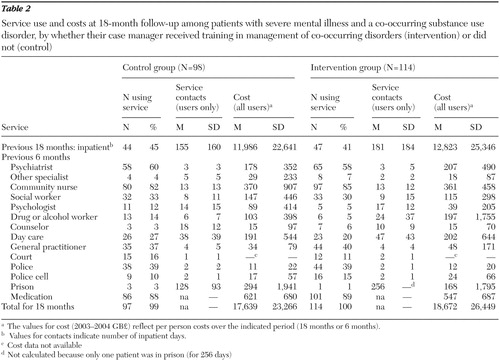
No major differences were found in the proportion of patients in each group who used specific services ( Table 2 ). Around four-fifths of patients had contacts with community mental heath nurses, and similar proportions were using medication for their symptoms. More than half the patients had seen a psychiatrist in the preceding six months, around a third had seen a social worker, and a third had contact with a general practitioner. A relatively large proportion of patients in both groups had contact with police. Inpatient psychiatric care was used by more than 40% of patients overall. The 18-month costs, which were dominated by inpatient care, did not differ significantly between the two groups. Per-person costs were £1,033 higher for the intervention group (bootstrapped 95% CI=-£5,568 to £6,734).
 |
To explore trends toward greater effectiveness of the intervention among those who had received it as intended, these analyses were repeated including only patients who received the integrated co-occurring disorders treatment from the 33 case managers who had fully completed training and the 85 persons in the "true" control group—that is, who remained with the same control group case manager throughout the study. However, the results of these analyses did not change any of the outcomes discussed in this article.
Discussion
This study investigated the effectiveness of a pragmatic intervention aimed at providing an integrated intervention for persons with severe mental illness who had a co-occurring substance use disorder. The study was conducted in a routine clinical setting typical of inner-city mental health services in England. It tested an intervention that had the potential to be widely disseminated, in line with current policy recommendations ( 16 ). Although the study did not find that the intervention had a significant impact on substance use at the 18-month follow-up, a modest effect was found on the co-occurring psychiatric disorder. BPRS scores at follow-up indicated greater improvement in the intervention group compared with the control group. The difference in improvement in psychiatric symptoms among participants in an intervention targeting both mental illness and substance use was also observed in the Manchester study ( 13 ) and in an integrated intervention that combined medication monitoring and cognitive-behavioral treatment for patients with bipolar disorder ( 34 ).
The improvement in symptoms may well reflect a genuine therapeutic effect; trained case managers reported greater therapeutic optimism and may have been more persistent in their efforts, as reflected in the greater reduction in unmet need for care. Furthermore, although we did not find a statistically significant difference between groups in substance use, confidence intervals were wide and thus included the possibility of an effect in either direction. This observation echoes the findings of several other evaluations of integrated treatment for co-occurring disorders that also failed to demonstrate a consistently clear benefit ( 35 , 36 ). Finally, in the only other British study to examine the effectiveness of training an entire team in an integrated intervention for co-occurring disorders, Graham and colleagues ( 37 ) used a nonrandomized longitudinal design to compare patient outcomes before and after team-based training. Training was provided for three teams immediately and replicated in two other teams after an 18-month delay. Patient outcomes were modest, and improvements were equal for patients of the intervention teams and those in the comparison group in which teams received delayed training.
Although our study has the advantage of testing an intervention that could be readily applied in routine health care settings, a number of limitations deserve special mention. First, although the investigators were independent of the training or clinical service, they were not blind to patients' intervention or control group status at follow-up and thus it is possible that the positive outcomes that were dependent on observer judgment could be attributed to bias. Second, there was substantial attrition of patients at follow-up, although no significant differences in demographic or baseline scores were found between completers and noncompleters. There were several practical challenges to the delivery of the intervention. Although training produced immediate gains in knowledge, some difficulties maintaining the interventions were encountered. Fewer than half of the case managers in the intervention group attended all training sessions, and supervision was occasionally disrupted by clinical service demands. By the end of the study, a third of the patients were no longer seeing the same case manager with whom they started. In the absence of ongoing formal assessments of fidelity, we cannot be certain that the intervention was consistently delivered. Finally, we cannot be certain that there was not some contamination between the intervention and comparison groups because participants in the comparison group were working alongside others who had received training.
These service delivery problems are not likely to be unique to the area of London in which the study was carried out. The high levels of turnover of qualified staff in inner-city services is well recognized, as are the pressures of routine work that often interrupts training and supervision. Taken together with the fact that the intervention was delivered in the context of routine work, it seems quite likely that the intervention was simply not an effective form of substance abuse treatment or that its duration was insufficient to achieve changes in substance use; however, compared with standard care, the intervention appears to have produced improvement in symptoms and level of unmet need at no additional cost.
The problems we encountered delivering and maintaining a high-quality intervention in routine care are not unique to integrated treatment for co-occurring disorders. The problems reflect a core dilemma in regard to achieving a balance between spreading skills broadly across teams or relying mostly on a highly skilled (and costly) dedicated psychological therapist. For example, even though the evidence for efficacy has been well established in research trials, the roll-out to routine care is often unsatisfactory, with patchy effectiveness and poor maintenance ( 38 ). Perhaps the biggest obstacle to effective implementation of this intervention is the assumption that case managers can take on new roles in addition to the services that they are already expected to provide without any adjustment to caseload or recognition that provision of a psychological therapy might require dedicated time built into the case manager's schedule. An alternative strategy might therefore be the creation on each team of a single position dedicated to the delivery of psychological therapy, with time set aside to deliver therapy and supervise a broadly trained workforce. This is also a reasonable next step for research to pursue, because such studies could test the efficacy of a more potent mix of motivational interviewing and cognitive-behavioral therapy in a design in which treatment "dose" could be more tightly controlled and fidelity to a treatment model more easily monitored.
Conclusions
Compared with standard care, integrated treatment for co-occurring disorders led to significant improvements in psychiatric symptoms and levels of met need but not in substance use or quality of life.
Acknowledgments and disclosures
This study was supported by the Bethlem and Maudsley National Health Service Trust.
The authors report no competing interests.
1. Duke PJ, Pantellis C, McPhillips MA, et al: Comorbid non-alcohol substance misuse among people with schizophrenia: epidemiological study in central London. British Journal of Psychiatry 179:509–513, 2001Google Scholar
2. Menezes PR, Johnson S, Thornicroft G, et al: Drug and alcohol problems among individuals with severe mental illnesses in south London. British Journal of Psychiatry 168:612–619, 1996Google Scholar
3. Wright S, Gournay K, Glorney E, et al: Dual diagnosis in the suburbs: prevalence, need and in-patient service use. Social Psychiatry and Psychiatric Epidemiology 35:297–304, 2000Google Scholar
4. Weaver T, Madden P, Charles V, et al: Comorbidity of substance misuse and mental illness in community mental health and substance misuse services British Journal of Psychiatry 183:304–313, 2003Google Scholar
5. Drake RE, Osher FC, Wallach MA: Alcohol use and abuse in schizophrenia: a prospective community study. Journal of Nervous and Mental Disease 177:408–414, 1989Google Scholar
6. Swofford C, Kasckow J, Scheller-Gilkey G, et al: Substance use: a powerful predictor of relapse in schizophrenia. Schizophrenia Research 20:145–151, 1996Google Scholar
7. Scott H, Johnson S, Menezes P, et al: Substance misuse and risk of aggression and offending among the severely mentally ill. British Journal of Psychiatry 172:345–350, 1998Google Scholar
8. Kamali M, Kelly L, Gervin M, et al: The prevalence of comorbid substance misuse and its influence on suicidal ideation among in-patients with schizophrenia. Acta Psychiatrica Scandinavica 101:452–456, 2000Google Scholar
9. McCrone P, Menezes PR, Johnson S, et al: Service use and costs of people with dual diagnosis in South London. Acta Psychiatrica Scandinavica 101:464–472, 2000Google Scholar
10. Drake RE, Mercer-McFadden C, Mueser KT, et al: Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophrenia Bulletin 24:589–608, 1998Google Scholar
11. Drake RE, Essock SM, Shaner A, et al: Implementing dual diagnosis services for clients with severe mental illness. Psychiatric Services 52:469–476, 2001Google Scholar
12. Ley A, Jeffery DP, McLaren S, et al: Treatment programmes for people with both severe mental illness and substance misuse. Cochrane Library, update software, 2001Google Scholar
13. Barrowclough C, Haddock G, Tarrier N, et al: Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry 158:1706–1713, 2001Google Scholar
14. Bellack A, Bennett M, Gearon J, et al: A randomized clinical trial of a new behavioral intervention for drug abuse in people with severe and persistent mental illness. Archives of General Psychiatry 63:426–432, 2006Google Scholar
15. James W, Preston NJ, Koh G, et al: A group intervention which assists patients with dual diagnosis reduce their drug use: a randomized controlled trial. Psychological Medicine 34:983–990, 2004Google Scholar
16. Mental Health Policy Implementation Guide: Dual Diagnosis Good Practice Guide. London, Department of Health, 2002Google Scholar
17. Johnson S, Thornicroft G, Afuwape S, et al: Effects of training community staff in interventions for substance misuse in dual diagnosis patients with psychosis (COMO study). British Journal of Psychiatry 191:451–453, 2007Google Scholar
18. Drake RE, Mueser KT, McHugo GJ: Clinician Rating Scales: Alcohol Use Scale, Drug Use Scale and Substance Abuse Treatment Scale, in Outcomes Assessment in Clinical Practice. Edited by Sederer LI, Dickey B. Baltimore, Williams and Wilkins, 1996Google Scholar
19. Swanson AJ, Pantalon MV, Cohen KR: Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. Journal of Nervous and Mental Disease 187:630–635, 1999Google Scholar
20. Van Horn DH, Bux DA: A pilot test of motivational interviewing groups for dually diagnosed inpatients. Journal of Substance Abuse Treatment 20:191–195, 2001Google Scholar
21. Lukoff D, Liberman RP, Neuchterlein KH: Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophrenia Bulletin 12:578–593, 1986Google Scholar
22. Burger GK, Yonker RD, Calsyn RJ, et al: A confirmatory factor analysis of the Brief Psychiatric Rating Scale in a homeless sample. International Journal of Methods in Psychiatric Research 12:192–196, 2003Google Scholar
23. Marsden J, Gossop M, Stewart D, et al: The Maudsley Addiction Profile (MAP): a brief instrument for assessing treatment outcome. Addiction 93:1857–1867, 1998Google Scholar
24. Saunders JB, Aasland OG, Babor TF, et al: Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction 88:791–804, 1993Google Scholar
25. Rosenberg SD, Drake RE, Wolford GL, et al: Dartmouth Assessment of Lifestyle Instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155:232–238, 1998Google Scholar
26. Priebe S, Huxley P, Knight S, et al: Application and results of the Manchester Short Assessment of Quality of Life (MANSA). International Journal of Social Psychiatry 45:7–12, 1999Google Scholar
27. Atkisson C, Zwick R: The Client Satisfaction Questionnaire: Psychometric Properties and Correlation With Service Utilisation and Psychotherapy Outcome. New York, Pergamon, 1982Google Scholar
28. Marsden J, Steward D, Gossop M: Assessing client satisfaction with treatment for substance use problems and the development of the Treatment Perceptions Questionnaire. Addiction Research 8:455–470, 2000Google Scholar
29. Rosen A, Hadzi-Pavlovic D, Parker G: The Life Skills Profile: a measure assessing function and disability in schizophrenia. Schizophrenia Bulletin 15:325–337, 1989Google Scholar
30. Slade M, Thornicroft G, Loftus L, et al: The Camberwell Assessment of Need. London, Gaskell, Royal College of Psychiatrists, 1999Google Scholar
31. Beecham J, Knapp M: Costing psychiatric interventions, in Measuring Mental Health Needs, 2nd ed. Edited by Thornicroft G. London, Gaskell, 2001Google Scholar
32. Stata Statistical Software, Release 8.0. College Station, Tex, Stata Corp, 2003Google Scholar
33. Miles H, Johnson S, Amponsah-Afuwape S, et al: Characteristics of subgroups of individuals with psychotic illness and a comorbid substance use disorder. Psychiatric Services 54:554–561, 2003Google Scholar
34. Schmitz JM, Averill P, Sayre S, et al: Cognitive-behavioral treatment of bipolar disorder and substance abuse: a preliminary randomized study. Addictive Disorders and Their Treatment 1:17–24, 2002Google Scholar
35. Drake RE, McHugo GJ, Clark RE, et al: Assertive community treatment for patients with co-occurring severe mental illness and substance use disorder: a clinical trial. American Journal of Orthopsychiatry 68:201–205, 1998Google Scholar
36. Lehman AF, Herron JD, Schwartz RP, et al: Rehabilitation for adults with severe mental illness and substance use disorders: a clinical trial. Journal of Nervous and Mental Disease 181:86–90, 1993Google Scholar
37. Graham H, Copello A, Birchwood M, et al: A preliminary evaluation of integrated treatment for co-existing substance use and severe mental health problems: impact on teams and service users. Journal of Mental Health 15:577–591, 2006Google Scholar
38. Fadden G: Implementation of family interventions in routine clinical practice following staff training programs: a major cause for concern. Journal of Mental Health 6:599–612, 1997Google Scholar



