Rates and Risk Factors for Homelessness After Successful Housing in a Sample of Formerly Homeless Veterans
Research suggests that housing combined with mental health services is an effective intervention for helping homeless persons with psychiatric disorders, addictive disorders, or both to access and maintain community housing ( 1 , 2 , 3 , 4 , 5 , 6 ). Once housed, a substantial proportion of these individuals maintain community housing for significant periods ( 7 , 8 , 9 ). In a five-year longitudinal study of 2,937 homeless persons with serious mental illness, Lipton and colleagues ( 9 ) found that 75% of their sample remained continuously housed at the one-year follow-up period and 50% remained housed at the five-year follow-up period. Although these figures are promising, far too many individuals return to homelessness after being housed.
Lipton and colleagues ( 9 ) found that the risk of subsequent homelessness was greatest in the first four months of being housed and for individuals placed in more structured, supervised settings. Substance abuse has also been identified as a major risk factor for returning to homelessness ( 7 , 8 , 9 ). Yet one study found that individuals with access to Section 8 housing were five times more likely than persons without such access to achieve stability in independent housing, regardless of substance abuse diagnosis ( 8 ).
In 2003 a report was published about an experimental evaluation of the collaborative Housing and Urban Development-Veterans Affairs Supported Housing (HUD-VASH) initiative that found that the combination of immediate access to rent subsidies through housing vouchers plus intensive case management significantly reduced days homeless by 36% over a three-year period, compared with intensive case management without vouchers and standard care ( 3 ). Data are limited, however, on the impact of such combined interventions on the risk of returning to homelessness after being housed.
In this study we further examined the longitudinal data from the HUD-VASH experimental trial to assess group differences in the risk of returning to homelessness after successful housing, identify sociodemographic and clinical factors associated with increased risk of returning to homelessness, and explore differential group effects that may be moderated by key participant characteristics.
Methods
HUD-VASH study
The study presented here was a secondary analysis of data from the evaluation of the HUD-VASH initiative ( 6 , 10 ). HUD-VASH began in 1992 with a memorandum of agreement between HUD and the Department of Veterans Affairs (VA) to provide permanent housing subsidies and case management to homeless veterans with psychiatric disorders, substance use disorders, or both. HUD provided over 1,000 Section 8 housing vouchers to participants, and the VA's Health Care for Homeless Veterans (HCHV) program provided intensive case management and outreach services to support these vouchers at 19 sites across the country. Case managers had a maximum caseload of 25 clients and, through use of a modified assertive community treatment model ( 9 ), encouraged weekly face-to-face contact, delivered community-based care, and provided linkages to VA services, including employment and substance abuse counseling ( 6 ). Retaining the apartment was not contingent upon involvement in VA treatment, although continued involvement was encouraged.
Criteria for inclusion in the HUD-VASH program included being eligible for VA services, living in a shelter or on the street for at least 30 days, and having a psychiatric disorder, substance use disorder, or both at the time of initial contact with the HCHV program. Recruitment for the study took place between June 1, 1992, and December 31, 1995. During this time 460 persons were enrolled in the experimental component of the HUD-VASH evaluation at four sites: San Francisco (N=107), San Diego (N=91), New Orleans (N=165), and Cleveland (N=97).
Sample and procedures
In addition to a brief intake assessment conducted with the sponsoring HCHV program, participants had a detailed baseline assessment at the time of enrollment into the study. Each veteran was assigned to one of three conditions: HUD-VASH (Section 8 voucher plus intensive case management); intensive case management only; and standard care, which consisted of short-term broker case management provided by HCHV program outreach workers. Case managers then assisted each client in obtaining his or her Section 8 voucher, locating an apartment, or both, depending on which group the client was randomly assigned to. An independent evaluation assistant conducted follow-up interviews with the clients every three months for up to five years. Because most of the questionnaires were self-report, no interrater reliability training or checks were performed. Evaluation assistants were able to find participants who left the program or lost their housing by contacting collateral sources and visiting local shelters and other community gathering places.
Of the 460 persons enrolled, 392 (85%) were housed at some point after the baseline interview (169 of 182 participants in the HUD-VASH group, or 93%; 76 of 90 participants in the group with intensive case management only, or 84%; and 147 of 188 participants in the standard care group, or 78%) ( χ2 =15.84, df=2, p<.001). Data from these housed participants were included in the analyses presented here. Of the 68 participants who were not included in the analyses, 41 (60%) were lost to follow-up after the baseline interview and 27 (40%) were not housed in the course of the study. Compared with participants who were not included, participants who were included had more diagnoses (mean±SD of 2.20±.78 versus .67±.58; F=11.68, df=1 and 384, p=.001), had more medical conditions (.43±.39 versus .23±.34; F=15.67, df=1 and 452, p<.001), and were more likely to have a diagnosis of alcohol abuse or dependence (N=282, or 72%, versus N=41, or 60%; χ2 =4.02, df=1, p=.05).
The number of participants remaining in the study at each of the following postbaseline time periods was 374 at one year (95%), 333 at two years (85%), 284 at three years (72%), 227 at four years (58%), and 150 at five years (38%). Participants in the HUD-VASH group and those in the group with only intensive case management remained in the study for approximately 200 more days than participants in the standard care group (F=6.20, df=2 and 389, p=.002).
Participants provided written informed consent, and the protocol was approved by the Human Investigations Committees at each VA medical center. Participants were paid $20 after each interview.
Measures
Demographic and clinical characteristics. The HCHV outreach intake assessment included information on demographic characteristics, drug and alcohol use, medical problems, psychiatric problems, employment, and mode of first contact with the VA.
The baseline and follow-up interviews assessed demographic characteristics, childhood history, number of nights of the previous 90 spent in each of 11 different types of residence, duration of current episode of homelessness, psychiatric symptoms, alcohol and drug use, employment, social support, and quality of life.
Composite scores from the Addiction Severity Index (ASI) ( 11 ) were used to assess alcohol, drug, medical, legal, employment, and psychiatric status. Possible scores on the ASI subscale range from 0 to 1, with higher scores indicating more serious problems. Internal consistency estimates range from .64 to .89 for the subscales ( 12 ).
Quality of life was evaluated with selected subscales from the Lehman Quality of Life Interview ( 13 ). Possible scores on each subscale range from 1 to 7, with higher scores indicating better quality of life. Internal consistency estimates range from .79 to .88 ( 14 ). Employment was also assessed by the number of days employed out of the last 30 days.
Social support was measured by the number of people in nine different categories to whom the participant reported feeling close, an index of the total frequency of contacts with these people, and the average number of types of people who would help with a loan, transportation, or help in an emotional crisis ( 15 , 16 ).
Analysis
The end point for the analysis presented here was the date of the first interview after at least one day of documented homelessness following successful housing, the date of the last interview (if it occurred within five years after baseline), or the date equivalent to five years postbaseline, whichever came first. Data were analyzed at four additional observation periods—intake, baseline, the first interview when housed, and the interview just before the end-point interview.
A series of independent analyses of variance and chi square analyses were conducted to identify variables that significantly differentiated groups at the four observation interviews. A categorical site variable and variables that significantly differentiated groups at intake, baseline, or time of housing were entered as covariates in subsequent analyses.
Two survival analyses were conducted with Cox regression models to predict subsequent housing tenure as a function of initial group treatment assignment, after controlling for site and partially confounding characteristics, and as a function of all possible predictors of housing tenure from intake, baseline, and the interview when first housed (using a forward stepwise procedure) and treatment condition. Participants who remained continuously housed throughout the study after initially being housed were classified as "continuous." "Failure" was defined as the first interview at which the client was homeless for at least one day out of the previous 90. Observations for clients who were continuously housed at the last observation point before five years postbaseline were treated as censored observations in the analysis.
Fifty-five percent of the participants (N=217) had no missing data on any of the variables across all the observation periods, and 38% (N=147) were missing data on one to five variables. Missing values were replaced by the mean of all participant scores for variables for which less than 5% of participants had missing values (N=20). Variables for which more than 5% of participants had missing values were excluded from the analyses.
Analyses were conducted using SPSS, version 14.0 ( 17 ).
Results
Sample characteristics
Participants were primarily male (N=373, or 95%), as one would expect in a sample of veterans. Most were either divorced or had never married (N=296, or 76%), and the mean±SD age at intake was 42.0±7.7 years. Forty-three percent of the participants (N=170) had been homeless between one and six months before the time of the outreach intake assessment, and 27% (N=105) had been homeless for two years or more.
At intake, participants in the group with only intensive case management were more likely than those in the other groups to be female. Participants in the HUD-VASH group were less likely than the comparison groups to have reported serious thoughts of suicide in the 30 days before intake, and they had significantly fewer psychiatric diagnoses ( Table 1 ).
 |
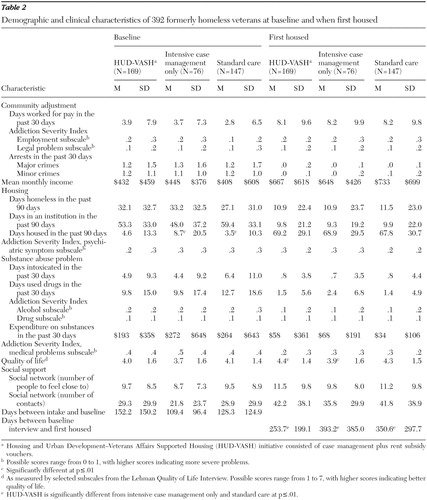
Table 2 displays community adjustment, housing, and clinical information for participants at baseline and the interview when first housed. At baseline, participants in the group with only intensive case management were housed significantly more days out of the previous 90 days, compared with participants in the standard care group. At the time of housing, participants in the group with only intensive case management had significantly lower scores on quality of life, compared with those in the HUD-VASH group. Participants in the HUD-VASH group were housed an average of 140 days before participants in the group with only intensive case management and 100 days before participants in the standard care group.
 |
At the interview just before loss of housing, the end of the study, or censorship, participants in the HUD-VASH group had significantly lower scores on the alcohol and drug subscales of the ASI, spent less on substances, and reported higher quality of life compared with participants in the group with intensive case management only ( Table 3 ). Table 4 contains significant findings according to year of final observation period. However, given the multiple comparisons involved over several time points, these findings should be regarded cautiously, as descriptive, rather than hypothesis driven.
 |
 |
Housing tenure
With housing "failure" defined as the date of the first interview after obtaining housing at which a client was homeless for at least one day, 172 (44%) met the definition for loss of housing within a period of five years after baseline. Thirty-four percent of these individuals (N=59) returned to homelessness for at least one day within the first six months of being housed. Seventy-two percent of participants remained housed after one year (N=282), 60% remained housed after two years (N=235), 52% remained housed after three years (N=204), 47% remained housed after four years (N=184), and 36% remained housed after five years (N=141). Results from the survival analysis indicate that compared with the other two groups, participants in the HUD-VASH group had a lower risk of returning to homelessness over the five-year period (87% lower risk compared with participants in the group with intensive case management only and a 76% lower risk compared with those in the standard care group), even after the analysis controlled for significant between-group differences ( Figure 1 ).

An additional survival analysis using a stepwise procedure was conducted to identify variables that significantly predicted loss of housing. The greatest risk factor for discontinuous housing was scores at the time of housing on the drug index subscale of the ASI. Having a diagnosis of posttraumatic stress disorder (PTSD) also increased the relative risk of discontinuous housing. Variables that lowered participants' risk of discontinuous housing included having a psychiatric problem or mood disorder at intake and having higher scores at the time of housing on the psychiatric subscale of the ASI. Treatment assignment remained a significant predictor of loss of housing after these factors were adjusted for, with participants in the HUD-VASH group having an 82% lower risk of loss of housing than participants in the group with intensive case management only and an 80% lower risk than participants in the standard care group. [A table showing the results of two separate Cox regression survival models controlling for site and significant covariates is available as an online supplement at ps.psychiatryonline.org.]
To explore potential moderating effects of drug use and psychiatric problems, additional analyses were conducted with a stratified sample on the basis of median splits of scores at the time of housing on the ASI drug subscale and on the ASI psychiatric subscale. No significant between-group differences were found among participants with lower scores on the ASI drug subscale. However, among participants with higher scores on the ASI drug subscale at the time of housing, participants in the HUD-VASH group were almost three times as likely as the other two groups to remain continuously housed ( χ2 =12.02, df=2, p=.002).
Similar analyses indicate that among participants with lower scores at the time of housing on the ASI psychiatric subscale, participants in the HUD-VASH group were 1.8 times as likely as participants in the standard care group to remain continuously housed ( χ2 =6.12, df=2, p=.05). Among participants with higher scores at the time of housing on the ASI psychiatric subscale, participants in the HUD-VASH group were 2.1 times as likely as those in the other two groups to remain continuously housed ( χ2 =9.03, df=2, p=.01).
Discussion
The study presented here examined the relative risk and predictors of returning to homelessness after successful housing in a sample of 392 formerly homeless veterans who participated in a randomized controlled trial. Over the course of up to five years of follow-up, 44% of all participants (N=172) returned to homelessness for at least one day after being successfully placed into housing. Consistent with previous research ( 9 ), one-third of these episodes occurred within the first six months of being housed.
Participants in the HUD-VASH group were initially housed at a higher rate and were less likely to return to homelessness than the other two groups. Although the groups did not differ in terms of alcohol or drug use at baseline or at the time of being housed, the HUD-VASH group had significantly lower scores on indices of alcohol and drug use and lower expenditures on substances at the interview before the final observation period. This finding is consistent with a recent reanalysis of the original HUD-VASH data using a multiple imputation technique that revealed significantly better drug and alcohol outcomes for participants in the HUD-VASH group, compared with those in the other two groups ( 18 ).
Consistent with previous research showing the positive relationship between enhanced quality of life and reduced substance use ( 19 ), participants in the HUD-VASH group also reported higher levels of quality of life at the time of being housed and before the final interview in the study. Proponents of supported housing models contend that the key elements of choice and integrated housing contribute to greater housing stability and appropriate use of mental health services, which in turn lead to improved functioning ( 20 ). Given that the Section 8 certificate likely opened up more housing options, it is possible that participants in the HUD-VASH group felt more content with the help that they received from their case managers and more satisfied with and secure in their housing situation once housed. These elements may have provided a stable foundation from which participants in the HUD-VASH group could focus on other areas of healing and health.
Consistent with previous research in this area, substance use was found to be a major risk factor for loss of housing after successful placement ( 7 , 8 , 9 ). Having a PTSD diagnosis also resulted in an 85% increased risk of reduced housing tenure. Having more psychiatric problems in general, however, was related to a lower risk of reduced housing tenure. Perhaps individuals with more psychiatric problems were more engaged in supportive services that helped to prevent subsequent loss of housing. After the analyses controlled for these additional risk factors, participants in the HUD-VASH group continued to have an 82% and an 80% reduction, respectively, in discontinuous housing, compared with those in the group with intensive case management only and those in the standard care group. An exploratory examination of the potential moderating impact of substance use or psychiatric problems revealed that HUD-VASH may have been particularly effective for participants with substance abuse problems.
The study presented here used data from a randomized controlled trial to examine the risk and predictors of loss of housing in a population of formerly homeless veterans. Because a criterion for this analysis was being housed at some point in the study, not all randomly assigned clients were included—thus these data have less internal validity than those of the initial trial. The data available in this study were also censored in most cases, because complete data for five years were available for only 28% of participants. The proportion who are reported to have lost their housing over the five years (44%) is a lower-bound estimate. However, the hazard ratios computed in this analysis provide an appropriate estimate for the relative risk across treatment categories.
Furthermore, the findings presented here pertain only to people who were housed for any length of time and who may have had as few as one day of subsequent days homeless. These criteria were selected to maximize the inclusion of the participants in the original randomized trial in the analysis presented here and to capture a more representative pattern of housing among formerly homeless individuals with psychiatric problems, substance abuse problems, or both. Finally, because the sample was limited to VA service users who are overwhelmingly male, the results may not be generalizable to other populations.
Conclusions
The study presented here is one of the few studies that has examined the rate and risk of loss of housing in a randomized controlled trial of a group of formerly homeless veterans. The results of this study suggest that adding vouchers to intensive case management, in addition to increasing the likelihood of obtaining housing, also can help to significantly reduce the risk of returning to homelessness, can enhance quality of life, and may provide a buffer to increased alcohol and drug use and expenditures on substances over time. Thus simply obtaining housing is not enough to ensure successful community tenure for a population of homeless people with psychiatric problems, addictive problems, or both—resources must be in place to help ensure that housing is maintained. Future research is needed to explore whether vouchers alone (without intensive case management) would achieve similar results.
Acknowledgments and disclosures
This study was funded by the VA New England Mental Illness Research, Education, and Clinical Center.
The authors report no competing interests.
1. Hurlburt MS, Wood PA, Hough RL: Providing independent housing for the homeless mentally ill: a novel approach to evaluating long-term longitudinal housing patterns. Journal of Community Psychology 43:291–310, 1996Google Scholar
2. Lehman AF, Dixon L, Kernan E, et al: A randomized trial of assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry 54:1038–1043, 1997Google Scholar
3. Rosenheck R, Kasprow W, Frisman L, et al: Cost-effectiveness of supported housing for homeless persons with mental illness. Archives of General Psychiatry 60:940–951, 2003Google Scholar
4. Shern D, Tsemberis S, Anthony W, et al: Serving street-dwelling individuals with psychiatric disabilities: outcomes of a psychiatric rehabilitation clinical trial. American Journal of Public Health 90:1873–1878, 2000Google Scholar
5. Shern DL, Tsemberis S, Winarski J, et al: The effectiveness of psychiatric rehabilitation for people who are street dwelling with serious disability related to mental illness, in Mentally Ill and Homeless. Edited by Breakey WR, Thompson JW. Amsterdam, Harwood Academic, 1997Google Scholar
6. Tsemberis SJ, Moran L, Shinn M, et al: Consumer preference programs for individuals who are homeless and have psychiatric disabilities: a drop-in center and a supported housing program. American Journal of Community Psychology 32:305–317, 2003Google Scholar
7. Goldfinger SM, Schutt RK, Tolomiczenko GS, et al: Housing placement and subsequent days homeless among formerly homeless adults with mental illness. Psychiatric Services 50:674–679, 1999Google Scholar
8. Hurlburt MS, Hough RL, Wood PA: Effects of substance abuse on housing stability of homeless mentally ill persons in supported housing. Psychiatric Services 47:731–736, 1996Google Scholar
9. Lipton FR, Siegel C, Hannigan A, et al: Tenure in supportive housing for homeless persons with severe mental illness. Psychiatric Services 51:479–486, 2000Google Scholar
10. Kasprow WJ, Rosenheck RA, Frisman L, et al: Referral and housing processes in a long-term supported housing program for homeless veterans. Psychiatric Services 51:1017–1023, 2000Google Scholar
11. McLellan A, Luborsky L, Woody G, et al: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease 268:26–33, 1980Google Scholar
12. Leonhard C, Mulvey K, Gastfriend DR, et al: The Addiction Severity Index: a field study of internal consistency and validity. Journal of Substance Abuse Treatment 18:129–135, 2000Google Scholar
13. Lehman A: A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 11:51–62, 1988Google Scholar
14. Lehman AF: Measures of quality of life among persons with severe and persistent mental disorders. Social Psychiatry and Psychiatric Epidemiology 31:78–88, 1996Google Scholar
15. Lam J, Rosenheck R: Social support and service use among homeless persons with serious mental illness. International Journal of Social Psychiatry 45:13–28, 1998Google Scholar
16. Vaux A, Athanassopulou M: Social support appraisals and network resources. Journal of Community Psychology 15:537–556, 1987Google Scholar
17. SPSS for Windows, Release 14.0.1. Chicago, SPSS Inc, 2005Google Scholar
18. Cheng A, Lin H, Kasprow W, et al: Impact of supported housing on clinical outcomes: analysis of a randomized trial using multiple imputation technique. Journal of Nervous and Mental Disease 195:83–88, 2007Google Scholar
19. Lam JA, Rosenheck RA: Correlates of improvements in quality of life among homeless persons with serious mental illness. Psychiatric Services 51:116–118, 2000Google Scholar
20. Siegel CE, Samuels J, Dei-In T, et al: Tenant outcomes in supported housing and community residences in New York City. Psychiatric Services 57:982–991, 2006Google Scholar



