Treatment Costs Related to Bipolar Disorder and Comorbid Conditions Among Medicaid Patients With Bipolar Disorder
Bipolar disorder, a recurrent illness with manic-depressive episodes, affects more than 2.6% of the U.S. adult population ( 1 , 2 ). The lifetime prevalence rate for bipolar spectrum disorders ranged from 3.0% to 6.5% in the U.S. adult population across several studies ( 3 , 4 ). The comorbid clinical conditions usually include psychiatric conditions, such as anxiety, alcohol and drug abuse, impulse-control disorders, and personality disorders ( 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 ), and medical conditions, such as hypertension, diabetes, chronic obstructive pulmonary disease, cerebral-vascular disease, and obesity ( 7 , 15 , 16 , 17 ).
The economic burden of bipolar disorder in the United States was estimated as $45 billion in 1991, including 17% for treatment costs and 83% for productivity loss, premature death, and family burden ( 18 ). The lifetime cost to all patients with bipolar disorder in the United States was estimated at 24 billion in 1998 dollars ( 19 ). In the United Kingdom the annual economic impact of bipolar disorder was estimated as £2 billion (about $3 billion U.S.) in 2002 ( 20 ). On the basis of medical claims, an adult patient with bipolar disorder in the United States annually spent $7,200 in private insurance settings in 1998 ( 21 ) and $12,100 in the Medicaid program in 2000 ( 22 ). Not only is the Medicaid program the nation's dominant payer for mental health services ( 23 ), but the number of Medicaid enrollees in managed care organizations has increased since the mid-1990s as well ( 24 ). According to California Medicaid data, the annual treatment cost for patients with bipolar disorder was $10,450, with inpatient care accounting for 44% and outpatient care accounting for 45% ( 25 ).
Even though cost studies have been conducted, treatment costs related to bipolar disorder and comorbid conditions for patients with bipolar disorder, including costs of medications, have not been previously examined. Previous cost estimates did not separate costs related to bipolar disorder and those related to comorbid conditions. Treatment costs for mental illness have become high and burdensome for managed care organizations and state Medicaid programs.
Mood stabilizers and anticonvulsants, such as lithium, carbamazepine, and divalproex sodium, are commonly used to control hypomanic or manic episodes ( 1 ). Emergent therapies for bipolar treatment include newer anticonvulsants (lamotrigine) and second-generation antipsychotics (olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole) ( 26 , 27 ). Recent prescription data indicate that 42%–64% of patients with bipolar disorder received mood stabilizers and 44%–60% received antipsychotic augmentation therapy ( 25 , 28 ). Patients with bipolar disorder often receive antidepressants during depressive episodes and as a component of maintenance treatment ( 26 ).
The objectives of this study were to measure and compare costs related to bipolar disorder and to comorbid conditions and to assess factors associated with different medications, clinical comorbidities, age, and gender for Medicaid patients with bipolar disorder.
Methods
Study design and data source
A retrospective cohort study was conducted. The primary data source was a multistate medical claims database (PHARMetrics) that included seven state Medicaid managed care programs in the Midwest, Northeast, South, and West. This database covers approximately two million managed care Medicaid enrollees from January 1998 to December 2002 (five calendar years). All Medicaid recipients were covered by health maintenance organizations. The Medicaid claims database included all pharmacy, medical, and institutional claims administered by managed care organizations. The medical claims included inpatient psychiatric hospital care and care provided in mental health centers, psychiatric residential treatment centers, and other medical care. Use of medical claims data to study health services and utilization has been well documented ( 29 , 30 ). The reliability and validity of diagnoses in claims data are also well documented in the literature ( 31 ).
Each medical claim was recorded with accompanying ICD-9 diagnostic codes that justified the medical service. Patient names, insurance plan identification numbers, and other patient identifiers were deleted from the claims database. We used randomized patient numbers and birth years to conduct data analyses. This project was approved by the University of Cincinnati Medical Center Institutional Review Board.
Patient selection
During the study period, 48,965 Medicaid patients had at least one medical claim with a diagnosis of affective disorder ( ICD-9 code 296.xx). We excluded 30,624 patients who had only a depression diagnosis ( ICD-9 codes 296.2x and 296.3x) and 4,841 patients who had a diagnosis of schizophrenia ( ICD-9 code 295) during the study period. Because Medicaid recipients aged 65 or older might also have Medicare coverage, their Medicaid claims may not reflect a complete medical picture. Therefore, 29 patients who were older than 64 were also excluded.
A diagnosis of bipolar disorder was indicated by any of the following ICD-9 codes: 296.0, 296.1, and 296.4–296.8. The index date of bipolar diagnosis (the date of selection for the cohort) was the first date of diagnosis indicated by ICD-9 bipolar codes during the study period. This resulted in a total of 13,471 patients with a bipolar diagnosis for the final cohort study.
Definitions and measure s
Treatment cost was defined as the sum of claims reimbursed in U.S. dollars for recipients' hospitalization (hospital accommodation, medical therapy services, physician encounters, and radiology diagnosis fees), emergency room visits (emergency room services and associated medical services), outpatient visits, mental health care (mental health inpatient care, mental health services, mental retardation services, and mental health support services), physician encounters, prescription drugs, laboratory tests, and other medical claims (for example, surgical procedures and transportation). The total treatment cost for patients with bipolar disorder was divided into cost related to bipolar disorder and to comorbid conditions.
Although the reimbursement (paid amount) may represent the financial burden on the managed care organizations, the charged amount has more generalizability to other health care environments. The reimbursement amount was used as a proxy of treatment cost that represents the financial burden on the Medicaid programs. For each medical claim from 1998 to 2002, costs were adjusted using the medical component of the Consumer Price Index (MCPI) as the dollar value in 2002 based on data from the Bureau of Labor Statistics. The annual MCPI rates of change were found to be 5.4% in 2001–2002, 4.2% in 2000–2001, 3.7% in 1999–2000, and 3.4% in 1998–1999 (32,33). Because MCPI covers all major aspects of medical services and pharmaceutical products that are related to the scope of our study, it was appropriate to use MCPI instead of general CPI for this study.
Bipolar-related treatment cost involved three areas. First, all medical claims with any ICD-9 codes for bipolar disorder for hospitalization, outpatient visits, and physician encounters were considered as direct costs of bipolar disorder. Second, some selected laboratory tests indicated by the Current Procedural Terminology (CPT) codes were also considered directly relevant for treatment of bipolar disorder, including serum drug concentration, complete blood and platelet count, chem-7 panel, thyroid function tests, liver function tests, urinalysis, electrocardiography, pregnancy tests, and glucose tests ( 19 ). Third, pharmacy claims for prescription drugs of mood stabilizers, antidepressants, first-generation and second-generation antipsychotics, and other concomitant therapies were documented. [A list of the prescription medications (both generic and brand names) documented in the study is available in an online supplement to this article at ps.psychiatryonline.org.]
Major clinical comorbidities for patients with bipolar disorder, as noted in previous studies ( 13 , 14 , 15 , 16 , 17 , 34 ), were categorized as psychiatric disorders, including alcohol and drug use disorders, anxiety disorders, impulse-control disorders, personality disorders, and eating disorders; and as medical conditions, including cerebral-vascular diseases, ischemic heart diseases, neoplasm or cancer, arthritis, obesity, diabetes mellitus, hypertension, and chronic obstructive pulmonary diseases.
Statistical analysis
Age for each patient was calculated on the basis of when the index date of bipolar disorder (the first bipolar diagnosis) occurred during the study period. Age categories were less than 13, 13–17, 18–34, 35–49, and 50–64 years. Both bipolar-related cost and total treatment cost were described and categorized by patient's hospitalization, outpatient care, physician encounters, prescriptions, laboratory tests, and other medical care. The follow-up quarters were decided on the basis of the index date for each patient.
The preliminary data analysis showed that treatment cost data were highly skewed distributions because of high-cost outliers, no use of medications for bipolar disorder, or different enrollment durations. Hence, Poisson regression analysis ( 35 ) was conducted for this study. The dependent variable was the sum of treatment cost divided by the total number of enrollment months per patient. The covariates included age, sex, medication use, psychiatric comorbidities, and medical comorbidities. All statistical analyses were conducted using SAS for Windows, version 8.1.
Results
Demographic and clinical characteristics
As shown in Table 1 , of 13,471 patients with bipolar disorder, 64% were female. The mean age was 29 years, and mean number of months of enrollment in Medicaid was 19. During the study period, patients with bipolar disorder received a variety of psychotropic medications: lithium, 13%; anticonvulsants, 35%; second-generation antipsychotics, 24%; first-generation antipsychotics, 22%; and antidepressants, 42%. Some patients received multiple medications for bipolar treatment. Twenty-eight percent of patients did not receive any of the medications for bipolar disorder documented for this study. Table 1 also shows key comorbidities for patients with bipolar disorder, including anxiety disorder (36%), hypertension (13%), drug use disorder (10%), alcohol use disorder (8%), obesity (8%), and diabetes (7%).
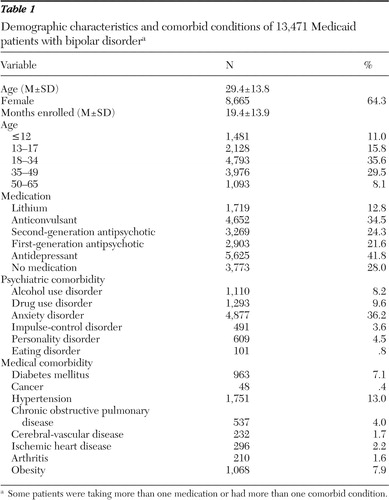 |
Treatment cost
Total treatment cost was attributed to cost related to treatment of bipolar disorder (30%) and comorbid conditions (70%) ( Table 2 ). The mean charge per patient-year was $22,110 for overall treatment (bipolar disorder and comorbid conditions). The mean reimbursed amount (cost) per patient-year was $11,641, with key cost components of inpatient care (35%), outpatient care (16%), prescription drugs (13%), and physician encounters (11%).
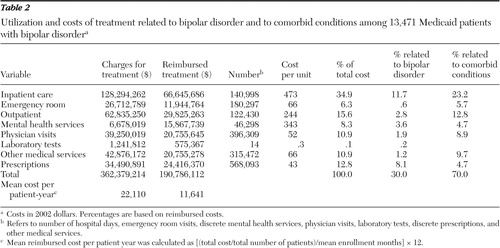 |
As shown in Table 3 , compared with costs for patients receiving antidepressants alone or no medication, the bipolar-related and total treatment costs were associated with use of second-generation antipsychotics (rate ratio [RR]=1.71 for bipolar-related cost and RR=1.26 for overall treatment), use of lithium (RR=1.27 and RR=1.00), and use of anticonvulsants (RR=1.37 and RR=1.06). The total treatment costs were also significantly associated with key comorbidities, such as drug use disorder (RR=1.58), cerebral-vascular disease (RR=1.72), ischemic heart disease (RR=1.47), and hypertension (RR=1.44).
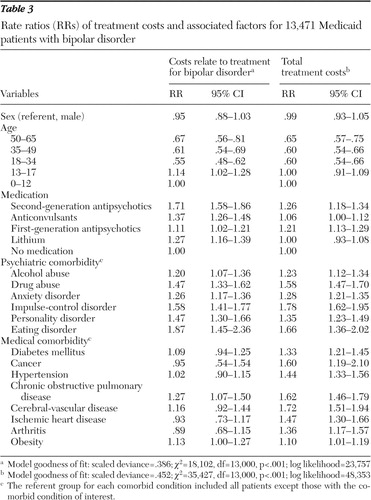 |
Discussion
This study compared costs for treatment related to bipolar disorder and to comorbid conditions among patients with bipolar disorder and examined costs associated with different medication use and key comorbidities. Not surprisingly, the major cost components for patients with bipolar disorder were hospital services, physician encounters, and prescription drugs.
The total treatment charge and reimbursed amounts per patient-year were $22,110 and $11,641 in 2002 dollars, respectively. On the basis of Wyatt and Henter's ( 18 ) estimation of $7 billion in treatment costs and Epidemiologic Catchment Area survey prevalence data (600,000 patients) ( 36 ), the annual treatment cost per patient in 1991 was $11,700. With a 4% annual inflation rate, the treatment cost would be approximately $18,012 in 2002. On the basis of the reported treatment cost (reimbursed amount) of $12,200 in 1996 for a patient with bipolar disorder by Stender and colleagues ( 21 ), this treatment cost would be approximately $16,054 in 2002 at a 4% annual inflation rate. Both treatment costs fall into the range between the Medicaid-reimbursed amount and the annual charge in the study reported here. The annual reimbursed amount ($11,641) in this study is slightly higher than Simon and Unützer's ( 22 ) estimation of $7,200 in 1998, presumably because the health plan they studied involved self-referral to specialty mental health services, moderate cost sharing for outpatient mental health services, prescription drug coverage, and limitations on long-stay psychiatric hospitalization ( 22 ). The study reported here included the seven-state managed care Medicaid population, which yielded a relatively large sample size. Thus the treatment cost for bipolar disorder should be representative of the cost for the Medicaid population.
Our findings are consistent with those of other studies that report that between 42% and 64% ( 25 , 28 ) of patients with bipolar disorder received lithium or anticonvulsants or both. More than half the patients with bipolar disorder in the study reported here received lithium or anticonvulsants or both plus antipsychotic augmentation or only antipsychotic monotherapy. The increased use of antipsychotics might be attributable to their antimanic or mood-stabilizing properties and more favorable tolerability profiles compared with first-generation agents ( 37 , 38 , 39 ). In addition, antipsychotic medications share several pharmacologic characteristics with antidepressants—that is, serotonin (5-HT) and norepinepherine reuptake inhibiting action and 5-HT-1A receptor agonism ( 27 , 40 , 41 ). Antipsychotic augmentation might also be efficacious for the treatment of bipolar depression, as seen in recent clinical trials ( 39 , 40 , 41 ).
Compared with patients who received lithium, those who received second-generation antipsychotics had the highest bipolar-related treatment costs, followed by those who received anticonvulsants and first-generation antipsychotics. The cost is likely attributable to the higher cost of second-generation antipsychotic medications. The study found that 70% of costs were for treatment of comorbid conditions. The total treatment cost was significantly associated with all key comorbidities, which is not surprising because bipolar disorder is commonly associated with psychiatric or medical comorbidities, such as anxiety disorder, alcohol and drug use disorders, personality disorder, eating disorder, diabetes mellitus, obesity, arthritis, hypertension, and chronic obstructive pulmonary disease ( 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ).
This study was limited to the managed care Medicaid population. Thus findings may not be generalizable to other patient populations. Although all state Medicaid programs receive prescription rebates from the pharmaceutical industry, we do not have any rebate information for the medical claims data. The prescription costs in this study were calculated on the basis of reimbursement or charge amounts. For those medical claims, there are up to two ICD-9 codes for each physician encounter and four ICD-9 codes for each episode of hospital care. We categorized the claims as bipolar related when at least one of the ICD-9 codes was related to a diagnosis of bipolar disorder. Although the laboratory test is a separated line item indicated by CPT codes, it is also difficult to identify each laboratory test related to treatment for bipolar disorder. Therefore, we might have overestimated the treatment costs attributable to bipolar disorder. Utilization and cost patterns in this cohort also reflect the characteristics of this particular health plan, which included a small amount of cost sharing for outpatient mental services and prescription drug coverage.
Given the limited research on costs related to bipolar disorder and comorbid conditions in the Medicaid population, the findings provide useful information for future illness management strategies and mental health policy decisions. The rising cost of antipsychotic medications has been a significant challenge for all state Medicaid programs. Medicaid has been cautious in its application of cost-containment measures for mental illness and antipsychotic medications because treatment regimens for bipolar disorder are not based on purely economic factors. Each medication may work uniquely for different patients because of patients' different medical conditions. Suboptimal treatment might lead to very costly outpatient care, inpatient hospitalization, or even suicide.
Conclusions
The findings of this study suggest that high treatment costs for bipolar disorder are associated with key psychiatric and medical comorbidities and antipsychotic medication use. Cost-containment efforts for patients with bipolar disorder may need to manage or prevent key psychiatric and medical comorbidities and to evaluate the association among use of different medications and treatment outcomes and hospital services.
Acknowledgments and disclosures
This study was funded by Bristol-Myers Squibb Company.
Dr. Guo has received research grants from Bristol-Myers Squibb and Ortho-McNeil Janssen Company. Dr. Keck is a consultant to or on the advisory boards of Abbott Laboratories, AstraZeneca, Pharmaceuticals, Bristol-Myers Squibb, GlaxoSmithKline, Janssen Pharmaceutica, Eli Lilly and Company, Neurocrine Biosciences, Ortho-McNeil, Inc., Pfizer Pharmaceutical Company, and Shire. Dr. Patel is a consultant for Eli Lilly and Shire.
1. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. American Psychiatric Association, Washington, DC, 1994Google Scholar
2. Kessler RC, Chiu WT, Demler O, et al: Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry 62:617–627, 2005Google Scholar
3. Hirschfeld RM, Calabrese JR, Weissman MM, et al: Screening for bipolar disorder in the community. Journal of Clinical Psychiatry 64:53–59, 2003Google Scholar
4. Akiskal HS, Bourgeois ML, Angst J, et al: Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. Journal of Affective Disorders 59(suppl 1):S5–S30, 2000Google Scholar
5. Koenigsberg HW, Kaplan RD, Gilmore MM, et al: The relationship between syndrome and personality disorder in DSM-III: experience with 2,462 patients. American Journal of Psychiatry 142:207–221,1985Google Scholar
6. Brady KT, Lydiard RB: Bipolar affective disorder and substance abuse. Journal of Clinical Psychopharmacology 12(suppl 1):17S–22S, 1992Google Scholar
7. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorder in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8–19, 1994Google Scholar
8. Weissman MM, Bruce LM, Leaf PJ, et al: Affective disorders, in Psychiatric Disorders in America: The Epidemiological Catchment Area Study. Edited by Robins IN, Regier DA. New York, Free Press, 1991Google Scholar
9. Winokur G, Coryell W, Akiskal HS, et al: Alcoholism in manic depressive (bipolar) illness, familial illness, course of illness, and the primary-secondary distinction. American Journal of Psychiatry 152:365–372, 1995Google Scholar
10. Feinman J, Dunner D: The effect of alcoholism and substance abuse on the course of bipolar affective disorder. Journal of Affective Disorders 37:43–49,1996Google Scholar
11. McElroy SL, Altshuler LL, Suppes T, et al: Axis I psychiatric comorbidity and its relationship with the historical illness variables in 288 patients with bipolar disorder. American Journal of Psychiatry 158:420–426, 2001Google Scholar
12. Escamilla MA, Batki S, Reus VI, et al: Comorbidity of bipolar disorder and substance abuse in Costa Rica: pedigree- and population-based studies. Journal of Affective Disorders 71:71–83, 2002Google Scholar
13. Goodwin RD, Hoven CW: Bipolar-panic comorbidity in the general population: prevalence and associated morbidity. Journal of Affective Disorders 70:27–33, 2002Google Scholar
14. George EL, Miklowitz DJ, Richards JA, et al: The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinical correlates. Bipolar Disorder 5:115–122, 2003Google Scholar
15. Keck PE, McElroy SL, Strackowski SM, et al: 12-month outcome of patients with bipolar disorder following hospitalization for a major or mixed episode. American Journal of Psychiatry 155:646–652, 1998Google Scholar
16. Keck PE, McElroy SL: Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. Journal of Clinical Psychiatry 64:1426–1435, 2003Google Scholar
17. Wozniak J, Biederman J, Monuteaux MC, et al: Parsing the comorbidity between bipolar disorder and anxiety disorders: a familial risk analysis. Journal of Child and Adolescent Psychopharmacology 12:101–111, 2002Google Scholar
18. Wyatt RJ, Henter I: An economic evaluation of manic-depressive illness, 1991. Social Psychiatry and Psychiatric Epidemiology 30:213–219, 1995Google Scholar
19. Begley CE, Annegers JF, Swann AC, et al: The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics 19:483–495, 2001Google Scholar
20. Gupta DR, Guest JF: Annual cost of bipolar disorder to UK society. Journal of Psychiatry 180:227–233, 2002Google Scholar
21. Stender M, Bryant-Comstock L, Phillips S: Medical resource use among patients treated for bipolar disorder: a retrospective, cross-sectional, descriptive analysis. Clinical Therapeutics 24:1668–1676, 2002Google Scholar
22. Simon GE, Unützer J: Health care utilization and costs among patients treated for bipolar disorder in an insured population. Psychiatric Services 50:1303–1308, 1999Google Scholar
23. Koyanagi C, Forguer S, Alfano E: Medicaid policies to contain psychiatric drug costs. Health Affairs 24:536–544, 2005Google Scholar
24. Heisler M, DeMonner SM, Billi JE, et al: Medicaid managed care: are academic medical centers penalized by attracting patients with high-cost conditions? American Journal of Managed Care 9:19–29, 2003Google Scholar
25. Li J, McCombs JS, Stimmel GL: Cost of treating bipolar disorder in the California Medicaid (Medi-Cal) program. Journal of Affective Disorders 71:131–139, 2002Google Scholar
26. Keck PE, McElroy SC: Treatment of bipolar disorder, in American Psychiatric Association Textbook of Psychopharmacology, 3rd edition. Edited by Schatzberg AF, Nemeroff CB. Arlington, Va, American Psychiatric Publishing, 2004Google Scholar
27. Keck PE Jr, Marcus R, Tourkodimitris S, et al: A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. American Journal of Psychiatry 160:1651–1658, 2003Google Scholar
28. Blanco C, Laje G, Olfson M, et al: Trends in the treatment of bipolar disorder by outpatient psychiatrists. American Journal of Psychiatry 159:1005–1010, 2002Google Scholar
29. Guo JJ, Gibson JT, Gropper DM, et al: Empiric investigation on direct costs-of-illness and healthcare utilization of Medicaid patients with diabetes mellitus. American Journal of Managed Care 4:1433–1446, 1998Google Scholar
30. Guo JJ, Keck PE, Corey-Lisle PK, et al: Diabetes mellitus associated with antipsychotic use among patients with bipolar disorders: a retrospective, population-based case-control study. Journal of Clinical Psychiatry 67:1055–1061, 2006Google Scholar
31. Strom BL, Carson JL, Halpern AC, et al: A population-based study of Stevens-Johnson syndrome: incidence and antecedent drug exposures. Archives of Dermatology 127:831–838, 1991Google Scholar
32. Consumer Price Index for all urban consumers 1998, 1999, 2000, 2001, 2002. Washington DC, US Department of Labor, Bureau of Labor Statistics. Available at www.bls.govGoogle Scholar
33. Bureau of Labor Statistics. Medical care inflation continues to rise. Washington DC, US Department of Labor, Bureau of Labor Statistics, May 29, 2001. Available at www.bls.gov/opub/ted/2001Google Scholar
34. Hilty DM, Brady KT, Hales RE: A review of bipolar disorder among adults. Psychiatric Services 50:201–213, 1999Google Scholar
35. Austin PC, Ghali WA, Tu JV: A comparison of several regression models for analyzing cost of CABG surgery. Statistics in Medicine 22:2799–2815, 2003Google Scholar
36. Regier D, Narrow WE, Rae DS, et al: The de facto US mental and addictive disorders services: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry 50:85–94, 1993Google Scholar
37. Keck PE Jr, McElroy SL: Aripiprazole: a partial dopamine D2 receptor agonist antipsychotic. Expert Opinion on Investigational Drugs 12:655–662, 2003Google Scholar
38. Hirschfeld RM, Keck PE Jr, Kramer M, et al: Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, double-blind, placebo-controlled trial. American Journal of Psychiatry 161:1057–1065, 2004Google Scholar
39. Moller HJ, Nasrallah HA: Treatment of bipolar disorder. Journal of Clinical Psychiatry 64(suppl 6):9–17, 2003Google Scholar
40. Mamo D, Kapur S, Shammi CM, et al: A PET study of dopamine D2 and serotonin 5-HT2 receptor occupancy in patients with schizophrenia treated with therapeutic doses of ziprasidone. American Journal of Psychiatry 161:818–825, 2004Google Scholar
41. Papakostas GI, Petersen TJ, Nierenberg AA, et al: Ziprasidone augmentation of selective serotonin reuptake inhibitors (SSRIs) for SSRI-resistant major depressive disorder. Journal of Clinical Psychiatry 65(2):217–221, 2004Google Scholar



