Correlates of Adverse Childhood Events Among Adults With Schizophrenia Spectrum Disorders
In this article, we examine the correlates of adverse childhood events in a large, multisite sample of public-sector mental health clients with a diagnosis of schizophrenia. The long-term health implications of adverse childhood events are becoming better understood in the general population. However, no published studies have reported on this relationship among people with schizophrenia. At the same time, the few available studies suggest that people with severe mental illness often experience adverse childhood events, including childhood sexual and physical abuse, neglect, witnessing domestic violence, and out-of-home placement ( 1 , 2 , 3 ). In addition, people with schizophrenia spectrum disorders may be more vulnerable to the impact of such events ( 1 , 3 , 4 ), and they are often characterized as having worse physical health and mental health functioning than the general population ( 5 ).
National surveys report that adverse events in childhood are common. Adverse events represent a broader category than trauma per se, which is defined by criteria specified in DSM-IV ( 6 ) and must involve actual or threatened death or serious injury or a threat to physical integrity. Adverse events also may include nontraumatic stressors, such as parental divorce or placement outside of the home. Using the more inclusive category of adverse events, the National Comorbidity Survey (NCS) ( 7 ) found that 50% of respondents reported experiencing two or more such events, including physical, sexual, or emotional abuse; neglect; parental substance abuse or mental illness; witnessing domestic violence; or the loss of a parent. The Adverse Childhood Experiences (ACE) study ( 8 ), which was conducted in a primary care setting, found that more than half of the sample had experienced at least one kind of adverse event in childhood and that 25% reported more than two types of events. Results from these studies also suggest that childhood abuse, neglect, and household dysfunction often occur together. For example, in the ACE study, 80% of individuals who were sexually abused in childhood reported at least one other type of adverse childhood experience, and 55% reported two or more types of other adverse experiences ( 8 ). Childhood adversity is associated with a broad range of negative health and mental health outcomes, both in childhood and among adult survivors.
There is emerging evidence that childhood sexual abuse and physical abuse are related to more severe symptoms among people with schizophrenia and other severe mental illnesses ( 9 , 10 , 11 , 12 ). However, little research has examined the relationship between the broad spectrum of adverse experiences in childhood and clinical, functional, and health outcomes of adults with schizophrenia. Studies to date have been limited by small samples ( 5 ) and have not examined the impact of cumulative exposure to adverse events in this population. With this study we aimed to examine the cumulative effects of these associations in a large, multisite sample.
Correlates of adverse childhood events among children
Several studies have reported associations between specific types of childhood adversity and physical and mental health outcomes in childhood. Children who have experienced the death of close family members appear to be at increased risk of depression, somatization, and obsessive-compulsive disorder ( 13 ). Children raised by nonparent kin or in foster care are at risk of increased health problems, developmental delays, and mental health problems compared with children raised by parents ( 14 , 15 , 16 , 17 , 18 ). Children who have witnessed domestic violence have high rates of internalizing and externalizing disorders, such as depression, aggression, and alcohol or drug use ( 19 , 20 ). Studies also have found that having a parent who is mentally ill is associated with increased family dysfunction and disorganization, exposure to violence, parent-child separation ( 21 , 22 , 23 ), and increased rates of mood disorders, anxiety disorders, and addictive disorders beyond what can be accounted for by genetic vulnerability ( 24 , 25 , 26 ).
Correlates of adverse childhood events among adults
Childhood abuse has been linked to increased medical problems in adulthood, including chronic fatigue syndrome, lung disease, autoimmune disorders, diabetes, migraines, gastrointestinal disorders, and ulcers ( 27 , 28 , 29 , 30 ). Findings from a number of studies indicate correlations between childhood abuse and increased rates of adult psychiatric disorders, including posttraumatic stress disorder (PTSD), depression, substance use disorders, borderline personality disorder, psychotic disorders, bipolar disorder, eating disorder, panic disorder, and antisocial personality disorder ( 2 , 31 , 32 , 33 , 34 , 35 , 36 ).
The experience of prolonged foster care (five or more years) is associated with poorer social functioning among adults ( 37 ) and with elevated rates of various psychiatric symptoms and diagnoses. These include increased self-destructive and high-risk behaviors, substance use, depression and other mood disorders, and anxiety disorders ( 38 , 39 , 40 , 41 , 42 , 43 ). Bereavement in childhood also has been reported to be related to depression in adulthood ( 44 , 45 ).
In addition to research showing associations between specific types of childhood adversity and physical and mental health functioning, there is evidence that the total cumulative exposure to adverse childhood events is related to several negative outcomes. For example, the ACE study found a strong and graded relationship between the amount of exposure to adverse childhood events and rates of substance use disorders, suicide attempts, and multiple sexual partners in adulthood. In addition, cumulative exposure to adverse childhood events predicted adult health problems, such as sexually transmitted diseases, heart disease, and cancer ( 8 ). These findings are consistent with those reported in the NCS study, which reported that total adverse childhood event exposure was correlated with increased rates of mood, anxiety, and addictive disorders in adulthood ( 7 ).
On the basis of major research in the general population ( 46 ), we hypothesized that greater exposure to adverse experiences in childhood would be related to worse functioning across several domains among people with schizophrenia, including psychiatric problems, substance abuse, physical health problems, and social functioning.
Methods
Participants
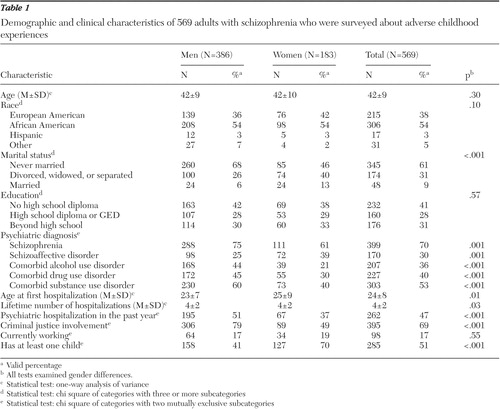
Participants included 624 adults with schizophrenia or schizoaffective disorder drawn from a larger investigation (N=1,152) of risky behavior and sexually transmitted diseases among women and men with severe mental illness ( 47 ). Participants entered the study between June 1997 and December 1998. The larger sample also included persons with affective disorders, chronic PTSD, and other diagnoses and who met state criteria for severe mental illness. However, the analyses presented in this article included only those with primary schizophrenia spectrum diagnoses. All participants were receiving treatment through the public mental health systems of Connecticut, Maryland, New Hampshire, or North Carolina, and study procedures were approved by all relevant institutional review boards. The settings from which they were recruited were diverse in that the mental health centers were located in rural, urban, and small metropolitan areas. Among the 624 persons with schizophrenia or schizoaffective disorders, 569 had complete data on adverse childhood events, which could be assessed and were included in the analyses. Characteristics of the sample are described in Table 1 .
 |
Measures
This study assessed psychiatric diagnosis, adverse childhood events, psychiatric problems, substance abuse, physical health, and social functioning through chart review, structured expert ratings, and standardized self-reports.
Psychiatric diagnosis. Diagnoses were ascertained with the Structured Clinical Interview for DSM-IV (SCID) (46) for 219 participants (19% of the sample), and chart diagnoses for the rest of the sample. Good agreement was found between SCID and chart diagnoses for those clients assessed by SCID ( κ =.72), which supports the general reliability of chart diagnoses for the broad purposes of the study.
Adverse childhood events. Standardized, self-report measures were administered to participants in an interview format to assess childhood abuse, household dysfunction, and loss that occurred during the first 16 years of life.
Childhood sexual abuse was assessed with the Sexual Abuse Exposure Questionnaire ( 48 ). This self-report scale identifies ten categories of increasingly invasive sexual experiences. This scale has been shown to have good test-retest reliability for both women and men with serious mental illness ( 49 ). Participants were considered to have experienced childhood sexual abuse if they responded affirmatively to any of the six items involving physical sexual contact.
Childhood physical abuse was assessed by the three most severe items from the violence subscale of the Conflict Tactics Scales ( 50 , 51 ), a widely used measure of domestic violence. An affirmative response on any of the three questions was used to indicate child physical abuse (being hit, being knocked down or thrown, and being burned or scalded on purpose).
Parental separation or divorce was defined by a response of yes to the question, "When you were growing up, did your parents/caretakers get a divorce or separation?"
Parental mental illness was defined by an affirmative response to the question, "When you were growing up, did your parent(s)/caretaker(s) ever see a counselor, psychologist, or psychiatrist, or go to a mental hospital, or take medication for an emotional problem?"
Domestic violence was determined by the following item: "When you were growing up, did you see or hear your parents/caretakers arguing or fighting a lot?"
Foster care and kinship care were assessed by two questions that asked the respondent whether she or he was placed in an orphanage, foster home, boys' home, reformatory, detention home, or jail or similar placement, or sent to live with relatives, family friends, or other people.
Parental death was based on client self-report of whether the client's father or mother died before the person turned 16.
Psychiatric problems
Health-related quality of life was assessed with the 12-item Short-Form Health Survey (SF-12) ( 52 ). The SF-12 consists of items assessing physical and mental health and yields two summary scores: the mental component summary (MCS) and physical component summary (PCS). Scoring is normatively based, with a mean±SD of 50±10; higher scores indicate better health. The SF-12 is reliable and valid in general and medical populations ( 52 ), as well as for people with severe mental illness ( 53 ).
PTSD was assessed with the PTSD Checklist (PCL) ( 54 ), a self-report screening measure for PTSD. The PCL includes 17 questions, one for each DSM-IV PTSD symptom, requiring the respondent to rate the severity of each symptom over the past month on a 5-point Likert scale, with higher scores indicating more severe symptoms. PTSD diagnoses are made if at least one criterion B (intrusive) symptom, three criterion C (avoidant) symptoms, and two criterion D (hyperarousal) symptoms are rated at 3 or above on the Likert scale. The PCL has strong test-retest reliability and convergent validity for people with severe mental illness ( 55 ).
Psychiatric symptoms were assessed with a subset of items from the Brief Psychiatric Rating Scale (BPRS) ( 56 ). The BPRS is a widely used interview for assessing psychiatric symptoms among persons with severe mental illness. The instrument includes 24 items, of which ten items are based on observation of the client alone. Because of interview length and concerns about client burden, only the observational items on the BPRS were included in this study, and these included items from three of the four factors reported by Thomas and colleagues ( 57 ): thought disturbance, animation, and apathy.
Hospitalization history was measured by the age at first hospitalization, the lifetime number of psychiatric hospitalizations, and the number of hospitalizations in the prior year.
Substance abuse
Current alcohol and drug use disorders were identified through a combination of the Dartmouth Assessment of Lifestyle Instrument (DALI) ( 58 ) and chart or SCID diagnosis. The DALI is an 18-item screening tool for substance use disorders (abuse or dependence) that was specifically developed and validated for persons with severe mental illness. It has high classification accuracy for DSM-IV substance use disorders of alcohol, cannabis, and cocaine. Cutoff scores have been developed with an empirically derived algorithm. Clients were categorized as having a substance use disorder if either the DALI or diagnosis (via chart or SCID) was positive for a substance use disorder.
Physical health outcomes
Physical health was assessed with items from the Piedmont Health Survey ( 59 ). Questions were asked about the following chronic medical problems: asthma, diabetes, heart trouble, hypertension, arthritis, cancer, lung disease, ulcers, stroke, epilepsy, head injury, and infectious diseases (such as sexually transmitted diseases and hepatitis). The problems endorsed were summed to form an overall measure of health problems. Participants also were asked to report for the past six months the number of times they had received care for a physical health problem and the number of days hospitalized for physical health problems. Health-related limitations were assessed by the PCS of the SF-12 ( 52 ). Scoring is normatively based, with a mean of 50±10; higher scores indicate better health.
Social functioning
Homelessness was defined as having no regular residence or as living in a shelter or on the street over the past six months.
Poverty status was based on past-year income and was determined by using the 1999 guidelines of the Department of Health and Human Services. These guidelines take into account income, marital status, and number of children.
Criminal justice involvement was defined as having ever been arrested for an alcohol offense, a drug offense, or a driving offense; for writing bad checks, shoplifting, loitering, trespassing, or being a public nuisance; physical or sexual assault against someone; or other miscellaneous offenses.
Work functioning was defined by whether the client was working at the time of the survey and whether the client had worked in the past year.
Overall functioning was assessed with the Global Assessment Scale ( 60 ). Scores on this scale range from 0 to 100 points. The measure assesses overall functional and symptomatic adjustment, with higher scores reflecting better functioning. Scores under 41, which represent "impairment in reality testing or communication" or "major impairment in several areas," were considered indicative of poor functioning.
Parental status was defined as having at least one child.
Procedure
After giving informed consent, respondents participated in structured interviews lasting 60 to 90 minutes, received pretest counseling for HIV-AIDS, and provided blood specimens as part of a screening for HIV and other sexually transmitted diseases. All participants were paid $35 and were provided with test results, posttest counseling, and referrals for follow-up testing and treatment, as needed. Permission also was obtained for chart review and obtaining information from treatment providers.
Statistical analyses
Prevalence rates of adverse events in childhood were computed first, followed by examination of the association between different types of adverse events. The association between cumulative number of adverse events and functional outcomes was then examined by performing logistic regression analyses, which controlled for demographic characteristics (gender, age, and race). Because of the large number of tests, we report significance only when p<.01.
Results
Prevalence of childhood adversities
Among the 569 adults with schizophrenia in this study, only 14% reported that they had experienced no adverse childhood events, whereas 18% reported one event and 46% had experienced three or more events. In the ACE and NCS studies, by comparison, about one-fifth and one-third of respondents, respectively, had experienced more than two adverse events, compared with about half the persons in our study. These results are summarized in Table 2 .
 |
Table 3 summarizes the co-occurrence of different adverse events in childhood. The most common form of adverse childhood event was child physical abuse, followed by witnessing domestic violence, foster or kinship care, parental separation or divorce, child sexual abuse, parental mental illness, and finally, parental death. Most clients who had experienced one adverse event had also experienced between two and three other events. For example, for those who had mentally ill parents, more than half also experienced parental divorce, foster care, and childhood physical and sexual abuse. For those who had experienced sexual abuse as children, more than half also experienced childhood physical abuse, witnessed domestic abuse, and were placed in foster care.
 |
Adverse childhood events and functional outcomes
The results of the logistic regression analyses evaluating the associations between cumulative exposure to adverse childhood events and hypothesized outcomes are summarized in Table 4 . As shown, adverse childhood events were significantly related to six of the ten measures of psychiatric disorder, the exceptions being BPRS score, recent psychiatric hospitalization, and recent self-injurious or suicidal behavior. All measures of substance abuse were significantly related to cumulative number of adverse childhood events. Adverse childhood events were significantly related to four of eight health functioning outcomes, including physician visits, health problems, and most strongly, HIV infection. Finally, with respect to social functioning, adverse events in childhood were related to homelessness and criminal justice system involvement but not to work, poverty, parental status, or overall functioning.
 |
Discussion
There are several limitations to this study. This was a retrospective study; thus underreporting of adverse childhood events may have occurred. Longitudinal follow-up of adults whose childhood abuse was documented has shown that their retrospective reports of childhood abuse are likely to underestimate the actual occurrence ( 61 , 62 ). In addition, although a large, multisite sample was used, it was nonetheless a convenience sample and may not be representative of all clients of the public mental health system in this country. For example, the sample underrepresents the Hispanic population. Finally, the measures used in this study also were not identical to those used in the NCS and ACE studies, so comparisons are somewhat approximate.
The prevalence of adverse childhood events reported in this sample was high, suggesting greater exposure to adverse childhood events among clients with schizophrenia in comparison with community samples ( 7 , 8 ). These findings are consistent with previous research indicating that adverse events in childhood are related to subsequent development of a range of mental illnesses, including schizophrenia ( 1 , 3 , 63 ). However, this study goes beyond prior research in this area by documenting relationships between cumulative exposure to adverse childhood events and different functional outcomes.
Our results suggest that adverse childhood events represent risk factors for psychiatric, substance abuse, health, and social functioning problems among adults with schizophrenia, as they do in the population as a whole. Because the primary disorder of schizophrenia is associated with high levels of morbidity and dysfunction in all of these domains, it may be harder to demonstrate the added impact of adverse childhood events on some of the variables assessed, such as poverty and unemployment. Adverse childhood events cumulatively predicted most of the mental health indices (such as presence of PTSD, alcohol or drug use disorders, days of hospitalization, suicidal thoughts, and self-rated mental health). These results are consistent with other studies showing relationships between childhood sexual and physical abuse and psychiatric symptoms in severe mental illness ( 2 , 5 , 9 , 10 , 11 , 12 , 64 ). Childhood adversity was also a powerful predictor of physical health outcomes, such as number of physician visits, self-rated physical problems, total number of self-reported physical illnesses, and presence of HIV. These findings extend prior research on the health correlates in adulthood of childhood adversity in the general population ( 27 , 28 , 29 , 30 ) to persons with schizophrenia.
Finally, adversity in childhood was a less strong predictor of functional outcomes in this study, predicting criminal justice involvement and homelessness but not poverty, employment status, or global functioning. Homelessness, criminal justice system involvement, and substance use disorders have all been linked to each other and to childhood adversity in the general population. All together, the findings suggest that even among people with an established severe mental illness (schizophrenia), those with higher levels of childhood adversity have significantly worse psychiatric, health, and social functioning than similar individuals with less exposure to such events.
Conclusions
Important implications of this study are that most clients with diagnoses of schizophrenia in the public mental health system are likely to have been exposed to serious adverse events in childhood and that the social and psychological consequences of this exposure include worse health, mental health, and functional outcomes. Exposure to adverse childhood events is associated with elevated rates of comorbid conditions such as alcohol abuse, drug abuse, and PTSD, even though these diagnoses are already elevated in this population. These comorbid disorders have a deleterious effect on the course of illness and may add considerable complexity to treatment management. Tailored interventions to address the adult consequences related to adverse childhood events may be necessary to improve outcomes for many clients with schizophrenia spectrum disorders.
Acknowledgments and disclosures
This research was supported by grants R01-MH-50094-03S2, P50-MH-43703, R01-MH-48103-05, P50-MH-51410-02, R24-MH-54446-05, and R01-MH-52872 from the National Institute of Mental Health, by grant UNC-CHJ from the Duke Program on Services Research for People With Severe Mental Disorders, by grant CT DMH from Yale, and by grant EPP97-022 from the Veterans Affairs Epidemiologic Research Information Center. The authors acknowledge the contributions of the members of the five-site Health and Risk Study Research Committee. Connecticut: Susan M. Essock, Ph.D., and Jerilynn Lamb-Pagone, M.S.N. Duke University, Durham, North Carolina: Marvin Swartz, M.D., Jeffrey Swanson, Ph.D., and Barbara J. Burns, Ph.D. Durham, North Carolina: Marian I. Butterfield, M.D., Keith G. Meador, M.D., M.P.H., Hayden B. Bosworth, Ph.D., Mary E. Becker, Richard Frothingham, M.D., Ronnie D. Homer, Ph.D., Lauren M. McIntyre, Ph.D., Patricia M. Spivey, and Karen M. Stechuchak, M.S. Maryland: Fred C. Osher, M.D., Lisa A. Goodman, Ph.D., Lisa J. Miller, Jean S. Gearon, Ph.D., Richard W. Goldberg, Ph.D., John D. Herron, L.C.S.W., Raymond S. Hoffman, M.D., and Corina L. Riismandel. New Hampshire: Patricia C. Auciello, M.S., George Wolford, Ph.D., Mark C. Iber, Ravindra Luckoor, M.D., Gemma R. Skillman, Ph.D., Rosemarie S. Wolfe, M.S., Robert M. Vidaver, M.D., and Michelle P. Salyers, Ph.D.
The authors report no competing interests.
1. Bebbington PE, Bhugra D, Brugha T, et al: Psychosis, victimisation and childhood disadvantage: evidence from the second British National Survey of Psychiatric Morbidity. British Journal of Psychiatry 185:220-226, 2004Google Scholar
2. Garno JL, Goldberg JF, Ramirez PM, et al: Impact of childhood abuse on the clinical course of bipolar disorder. British Journal of Psychiatry 186:121-125, 2005Google Scholar
3. Read J, Perry BD, Moskowitz A, et al: The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry 64:319-345, 2001Google Scholar
4. Heads T, Taylor P, Leese M: Childhood experiences of patients with schizophrenia and a history of violence: a special hospital sample. Criminal Behaviour and Mental Health 7:117-130, 1997Google Scholar
5. Lysaker PH, Meyer PS, Evans JD, et al: Childhood sexual trauma and psychosocial functioning in adults with schizophrenia. Psychiatric Services 52:1485-1488, 2001Google Scholar
6. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
7. Kessler RC, Davis CD, Kendler KS: Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine 27:1101-1119, 1997Google Scholar
8. Felitti VJ, Anda RF, Nordenberg D, et al: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 14:245-258, 1998Google Scholar
9. Ellason JW, Ross C: Childhood trauma and psychiatric symptoms. Psychological Reports 80:447-450, 1997Google Scholar
10. Muenzenmaier K, Meyer I, Struening E, et al: Childhood abuse and neglect among women outpatients with chronic mental illness. Hospital and Community Psychiatry 44:666-670, 1993Google Scholar
11. Ross CA, Anderson G, Clark P: Childhood abuse and the positive symptoms of schizophrenia. Hospital and Community Psychiatry 45:489-491, 1994Google Scholar
12. Read J, Argyle N: Hallucinations, delusions, and thought disorder among adult psychiatric inpatients with a history of child abuse. Psychiatric Services 58:1467-1472, 1999Google Scholar
13. Patton GC, Coffey C, Posterino M, et al: Life events and early onset depression: cause or consequence? Psychological Medicine 33:1203-1210, 2003Google Scholar
14. Chernoff R, Combs-Orme T, Risley-Curtiss C, et al: Assessing the health status of children entering foster care. Pediatrics 93:594-601, 1994Google Scholar
15. Halfon N, Berkowitz G, Klee L: Mental health service utilization by children in foster care in California. Pediatrics 89:1238-1244, 1992Google Scholar
16. Halfon N, Mendonca H, Berkowitz G: Health status of children in foster care: the experience of the Center for the Vulnerable Child. Archives of Pediatrics and Adolescent Medicine 149:386-392, 1995Google Scholar
17. Mcintyre A, Kessler TY: Psychological disorders among foster care children. Journal of Clinical Child Psychology 15:297-303, 1986Google Scholar
18. Pilowsky DJ: Psychopathology among children placed in family foster care. Psychiatric Services 46:906-910, 1995Google Scholar
19. el-Bayoumi G, Borum ML, Haywood Y: Domestic violence in women. Medical Clinics of North America 82:391-401, 1998Google Scholar
20. Sisley A, Jacobs LM, Poole G, et al: Violence in America: a public health crisis—domestic violence. Journal of Trauma 46:1105-1112, 1999Google Scholar
21. Beardslee WR, Versage EM, Gladstone TR: Children of affectively ill parents: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry 37:1134-1141, 1998Google Scholar
22. Beck CT: Maternal depression and child behaviour problems: a meta-analysis. Journal of Advanced Nursing 29:623-629, 1999Google Scholar
23. Nicholson J, Nason MW, Calabresi AO, et al: Fathers with severe mental illness: characteristics and comparisons. American Journal of Orthopsychiatry 69:134-141, 1999Google Scholar
24. Downey G, Coyne JC: Children of depressed parents: an integrative review. Psychological Bulletin 108:50-76, 1990Google Scholar
25. Gelfand DM, Teti DM: The effects of maternal depression of children. Clinical Psychology Review 10:329-353, 1990Google Scholar
26. Wals M, Hillegers MHJ, Reichart C, et al: Prevalence of psychopathology in children of a bipolar parent. Journal of the American Academy of Child and Adolescent Psychiatry 40:1094-1102, 2001Google Scholar
27. Romans S, Belaise C, Martin J, et al: Childhood abuse and later medical disorders in women: an epidemiological study. Psychotherapy and Psychosomatics 71:141-150, 2002Google Scholar
28. Goodwin RD, Hoven CW, Murison R, et al: Childhood abuse and risk of gastrointestinal disorders and migraine during adulthood. American Journal of Public Health 93:1065-1067, 2003Google Scholar
29. Goodwin RD, Stein MB: Association between childhood trauma and physical disorders among adults in the United States. Psychological Medicine 34:509-520, 2004Google Scholar
30. Talley NJ, Fett SL, Zinsmeister AR, et al: Gastrointestinal tract symptoms and self-reported abuse: a population-based study. Gastroenterology 107:1040-1049, 1994Google Scholar
31. Fergusson DM, Horwood LJ, Lynskey MT: Childhood sexual abuse and psychiatric disorder in young adulthood: II. psychiatric outcomes of childhood sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry 35:1365-1374, 1996Google Scholar
32. Hammersley P, Dias A, Todd G, et al: Childhood trauma and hallucinations in bipolar affective disorder: preliminary investigation. British Journal of Psychiatry 182:543-547, 2003Google Scholar
33. Kendall-Tackett KA, Williams LM, Finkelhor D: Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychological Bulletin 113:164-180, 1993Google Scholar
34. Kendler KS, Bulik CM, Silberg J, et al: Childhood sexual abuse and adult psychiatric and substance abuse disorders in women: an epidemiological and cotwin control analysis. Archives of General Psychiatry 57:953-959, 2000Google Scholar
35. Rind B, Tromovitch P: A meta-analytic review of findings from national samples on psychological correlates of child sexual abuse. Journal of Sex Research 34:237-255, 1997Google Scholar
36. Trull TJ: Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology 110:471-481, 2001Google Scholar
37. Jones MA, Moses B: West Virginia's Former Foster Children: Their Experience in Care and Their Lives as Young Adults. New York, Child Welfare League of America, 1984Google Scholar
38. Barth RP: On their own: the experiences of youth after foster care. Child and Adolescent Social Work Journal 7:419-440, 1990Google Scholar
39. Dumaret AC: Adult outcome of children reared for long term periods in foster families. Child Abuse and Neglect 21:911-927, 1997Google Scholar
40. Ehrle J, Green R, Clark R: Children Reared by Relatives: How Are They Faring? Washington, DC, Urban Institute, 2001Google Scholar
41. McDonald TP, Allen RI, Westerfelt A, et al (eds): Assessing the Long-Term Effects of Foster Care: A Research Synthesis. Washington, DC, Child Welfare League of America Press, 1996Google Scholar
42. Dube SR, Anda RF, Felitti VJ, et al: Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence and Victims 17:3-17, 2002Google Scholar
43. Kessler RC, Magee WJ: Childhood family violence and adult recurrent depression. Journal of Health and Social Behavior 35:13-17, 1994Google Scholar
44. Brown GW, Moran P: Clinical and psychosocial origins of chronic depressive episodes: I. a community survey. British Journal of Psychiatry 165:447-456, 1994Google Scholar
45. Zlotnick C, Ryan CE, Miller IW, et al: Childhood abuse and recovery from major depression. Child Abuse and Neglect 19:1513-1516, 1995Google Scholar
46. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis-I Disorders—Patient Edition (SCID-I/P, Version 2.0). New York, New York State Psychiatric Institute, Biometrics Research Department, 1996Google Scholar
47. Rosenberg SD, Trumbetta SL, Mueser KT, et al: Determinants of risk behavior for HIV/AIDS in people with severe and persistent mental illness. Comprehensive Psychiatry 42:263-271, 2001Google Scholar
48. Rodriguez N, Ryan SW, Van De Kemp H, et al: Posttraumatic stress disorder in adult female survivors of childhood sexual abuse: a comparison study. Journal of Consulting and Clinical Psychology 65:53-59, 1997Google Scholar
49. Goodman LA, Thompson KM, Weinfurt K, et al: Reliability of reports of violent victimization and PTSD among men and women with SMI. Journal of Traumatic Stress 12:587-599, 1999Google Scholar
50. Straus M: Measuring intra-family conflict and violence: the Conflict Tactics Scales, in Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Edited by Straus M, Gelles R. New Brunswick, NJ, Transaction Books, 1989Google Scholar
51. Straus M: New scoring methods for violence and new norms for the Conflict Tactics Scales, in Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Edited by Straus M, Gelles R. New Brunswick, NJ, Transaction Books, 1989Google Scholar
52. Ware JJ, Kosinski M, Keller SD: A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care 34:220-233, 1996Google Scholar
53. Salyers MP, Bosworth HB, Swanson JW, et al: Reliability and validity of the SF-12 Health Survey among people with severe mental illness. Medical Care 38:1141-1150, 2000Google Scholar
54. Blanchard EP, Jones-Alexander J, Buckley TC, et al: Psychometric properties of the PTSD checklist. Behavior Therapy 34:669-673, 1996Google Scholar
55. Mueser KT, Salyers MP, Rosenberg SD, et al: A psychometric evaluation of trauma and PTSD assessments in persons with severe mental illness. Psychological Assessment 13:110-117, 2001Google Scholar
56. Lukoff D, Nuechterlein KH, Ventura J: Manual for the Expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594-602, 1986Google Scholar
57. Thomas A, Donnell A, Young T: Factor structure and differential validity of the expanded brief psychiatric rating scale. Assessment 11:177-187, 2004Google Scholar
58. Rosenberg SD, Drake RE, Wolford GL, et al: The Dartmouth Assessment of Lifestyle Instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155:232-238, 1998Google Scholar
59. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511-2518, 1990Google Scholar
60. Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 33:766-771, 1976Google Scholar
61. Widom CS, Shepard RL: Accuracy of adult recollections of childhood victimization: part 1. childhood physical abuse. Psychological Assessment 8:412-421, 1996Google Scholar
62. Widom CS, Morris S: Accuracy of adult recollections of childhood victimization: part 2. childhood sexual abuse. Psychological Assessment 9:34-46, 1997Google Scholar
63. Malmberg A, Lewis G, David A, et al: Premorbid adjustment and personality in people with schizophrenia. British Journal of Psychiatry 172:308-313, 1998Google Scholar
64. Swett C, Jr., Surrey J, Cohen C: Sexual and physical abuse histories and psychiatric symptoms among male psychiatric outpatients. American Journal of Psychiatry 147:632-636, 1990Google Scholar



