Differential Medication Adherence Among Patients With Schizophrenia and Comorbid Diabetes and Hypertension
Most patients with chronic conditions, such as schizophrenia, diabetes, and hypertension, must take medications regularly if they are to avoid adverse health outcomes ( 1 , 2 , 3 , 4 , 5 , 6 , 7 ). Although self-care plans routinely emphasize the importance of appropriate medication use, many patients are poorly adherent to pharmacotherapy ( 8 ) and fall short of achievable health goals as a result. Multiple studies have documented low rates of adherence to antipsychotic medications among patients with schizophrenia ( 9 , 10 , 11 , 12 ), and although some risk factors for medication nonadherence have been identified ( 13 , 14 , 15 ), adherence behaviors remain poorly understood overall.
Medication adherence often has been considered to be a patient-level attribute, under the assumption that most determinants of adherence affect all treatments in a regimen similarly. However, patients' beliefs about the necessity and side effects of specific medications may contribute to differences in adherence ( 16 ). Several studies have reported that patients with multiple medical conditions actively choose which treatments to forego when cost pressures become a problem ( 17 , 18 , 19 ). Little is known about the extent to which patients with schizophrenia and comorbid physical illnesses vary in their adherence across types of drugs or the characteristics of prescriptions associated with adherence levels.
Using longitudinal data from medical records of a Department of Veterans Affairs (VA) national patient registry, we examined variation in medication adherence across drug types in a large sample of patients receiving care for schizophrenia as well as two comorbid conditions: diabetes and hypertension. For patients with schizophrenia, adherence to medications for comorbid problems could be poorer either because patients see no immediate symptomatic benefit of these treatments or because their clinicians justifiably emphasize the importance of using their antipsychotic medication ( 20 , 21 ). However, patients with schizophrenia often have deficits in cognitive flexibility, concentration, and memory ( 22 , 23 , 24 , 25 ). These deficits may lessen adherence across all of the medications in the patient's regimen, thereby reducing variations in adherence across therapeutic classes ( 26 ). The VA provides an ideal setting in which to examine intrapatient variation in medication adherence behaviors, because the VA prescription benefit provides relatively generous and consistent coverage nationwide ( 27 ) and national VA disease registries enable the identification of a large sample of patients with schizophrenia and multiple comorbidities.
Methods
Data sources
Data were obtained from the VA National Psychosis Registry ( 28 ), which includes clinical and health service utilization data for all VA patients with a psychotic disorder. Information in the registry is compiled from annual extracts of administrative databases representing all VA inpatient and outpatient services, as well as all medication refills. The VA Ann Arbor Healthcare System Human Subjects Committee approved analyses such as those in this study with a waiver of informed consent.
Sample selection
Using the registry, we identified patients in fiscal year 2001 (FY 2001; October 1, 2000, through September 30, 2001) who had ICD-9 diagnosis codes indicating schizophrenia or a schizoaffective disorder, as well as both diabetes and hypertension. Only patients with refill information indicating that they were using oral medications for each condition during the year were eligible for inclusion in the analytic sample of 3,397 patients. For these patients, we evaluated medication adherence in FY 2002. Once patients are prescribed medication for schizophrenia, diabetes, and hypertension, they may switch drugs but rarely discontinue medication use altogether. Thus we assumed that all patients should be refilling each medication type throughout the observation period. No patients filled prescriptions for insulin during the study period, suggesting that all should have been using oral hypoglycemic agents continuously. We excluded 1,623 patients who were using more than two medications within a class, because adherence measures for these complex regimens have not been validated. Finally, we excluded patients with fewer than 90 noninstitutionalized days of observation in FY 2002 and those who filled two or more prescriptions as outpatients during an inpatient stay. The final analytic sample included 1,686 patients.
Measuring adherence with medication possession ratios
Medication possession ratios (MPRs) provided a validated measure of patients' adherence on the basis of their pattern of medication refills ( 5 , 9 , 29 ). For patients with only one medication within a therapeutic class, MPRs were calculated by dividing the total number of days of medication supplied by the number of days' supply needed if the patient was taking a full dosage of medication continuously during outpatient periods in FY 2002. For patients taking more than one medication within a therapeutic class, we calculated medication-specific MPRs and then a weighted average to estimate the class-specific MPR. If two medications within a class were prescribed concurrently, the denominator for the second drug's "days' supply needed" extended only until the end of its prescription if the other drug within the class continued to be prescribed. The equation was thus MPR=number of days of medication supplied by outpatient pharmacies)/(number of days' supply needed for continuous outpatient medication use).
The numerator of the MPR was calculated by adding the number of days' supply from each outpatient prescription filled during the year. Medications received at the time of discharge from inpatient stays were included in the outpatient supply. For prescriptions filled in FY 2001, we included the number of days' supply, if any, that extended into FY 2002. The denominator of the MPR was calculated as the number of noninstitutionalized days between the start of the fiscal year and either the end of the year or the date of death.
An MPR of 1.0 indicates that the patient received all the medications needed to take a full dosage continuously throughout the period, whereas an MPR of .5 indicates medication sufficient for only half of needed days. As in prior studies ( 5 ) some patients had MPRs greater than 1.0, most likely because these patients lost prescriptions or providers frequently changed their prescription dosages.
Covariates
Information on patients' sociodemographic characteristics and health service use was obtained from the National Psychosis Registry. Medication copayments and other limits on coverage are waived for VA patients with military service-connected disabilities, and we captured data on service connection from administrative files. Patients' distance to VA care was calculated on the basis of zip code of residence according to standard procedures ( 30 ). We used indicators of psychiatric and nonpsychiatric hospitalizations in the 12 months before FY 2002 to measure the severity of patients' psychiatric and physical illness. Patients' involvement with outpatient care was measured by the number of mental health and medical outpatient visits during the year. We included a count of all medications filled during FY 2002 as a measure of patients' overall medication burden.
In addition to medication type, we considered three other characteristics of each treatment regimen: whether the patient filled one or two different medications of one type during the year, the average number of days of medication supplied per refill, and the proportion of medication refills that were mailed to the patient versus dispensed at VA outpatient centers.
Analytic approach
The primary goal of our analyses was to examine intrapatient variation in medication adherence across treatment types and to estimate the impact on adherence of other medication-specific characteristics and patient-level covariates. We fit multivariate logistic regression models in which MPRs less than .8 were used as the dependent variable to indicate a significant adherence problem. Medication type was the primary predictor variable of interest. MPRs less than .8 have been found in prior studies to be associated with poorer outcomes ( 5 , 29 ). All multivariate analyses were multilevel, with patients' adherence represented by three observations, one observation for each therapeutic class. Additional medication-level data were included (such as average refill interval) as well as patient-level covariates (such as race). We controlled for the nesting of adherence data within patients and patients within facilities by using the cluster command in SAS ( 31 ).
Three nested multivariate models were estimated. In model 1, we included medication type indicators as well as indicators of patients' sociodemographic characteristics as controls for confounding. In model 2, we included all of the variables in model 1, as well as measures of patients' health service use. Model 3 included all previous variables as well as additional information about the number of medications in each therapeutic class (one or two), average number of days supplied, and the proportion of refills dispensed by mail versus in outpatient centers.
We conducted extensive auxiliary analyses to test the robustness of the models. Analyses with MPR cutoff points of 50%, 60%, 70%, and 90% showed a similar pattern of effects. We refit models for the subset of 1,318 patients with two full years of refill data—in other words, refills in FY 2002 and FY 2003—in order to expand the opportunities to detect poor adherence for treatments with relatively high numbers of days supplied per refill.
Results
Patient and regimen characteristics
Most patients were male, Caucasian, and unmarried ( Table 1 ). Most had not been hospitalized in the prior 12 months, although patients had relatively high rates of outpatient mental health and physical service use. Single-medication regimens were more common for antipsychotic treatment (78% of patients) than for treatment of diabetes (54%) or hypertension (50%) ( Table 2 ). Patients were more likely to receive a medication supply of 30 days or less when refilling their antipsychotic medications (79%) than when filling prescriptions for their hypoglycemic (16%) or antihypertensive medications (11%).
 |
 |
Variation in adherence across medication types
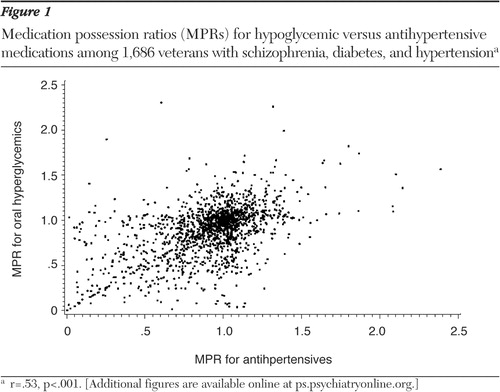
Bivariate analyses suggested substantial intrapatient variation in MPRs. Figure 1 shows the MPRs for hypoglycemic versus antihypertensive medications. The distributions were similar for hypoglycemic versus antipsychotic medications and for antipsychotic versus antihypertensive medications. [Figures illustrating the MPRs for these other bivariate comparisons are available in an online supplement to this article at ps.psychiatryonline.org.] The bivariate correlation of MPRs was highest for patients' two physical disorders ( Figure 1 ), hypertension and diabetes (r=.53). Statistically significant but weaker associations were observed between the MPRs for each physical condition and patients' antipsychotic medication. Information about antipsychotic medication adherence explained only 13% of the variance in patients' antihypertensive MPRs, and antipsychotic MPRs explained only 16% of the variance in MPRs for hypoglycemic medications.
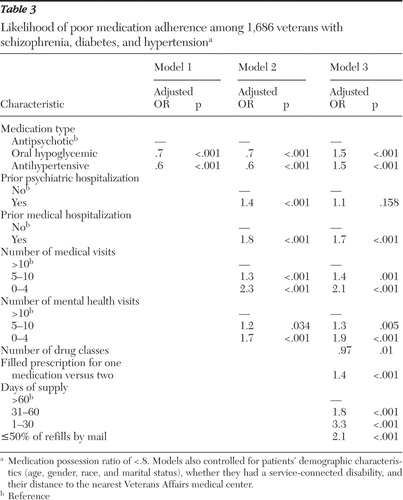
In unadjusted analyses, patients were less likely to have poor adherence (MPR less than .8) to their hypoglycemic (29%) or antihypertensive medications (26%) than to their antipsychotic medications (35%; p< .001). Multivariate analyses controlling for patients' sociodemographic characteristics and health service use ( Table 3 , model 2), showed a similar pattern. However, when other characteristics of each medication regimen, including the average days' supply, were controlled for (model 3), the adjusted odds of poor adherence were significantly higher for hypoglycemic and antihypertensive medications than for antipsychotic medication (both adjusted odds ratios were 1.5, p<.001). Regimens with an average 30 days' supply or less were associated with a 3.3-fold increase in the relative odds of nonadherence as compared with a supply of 60 days or more.
 |
Discussion
Memory and attentional difficulties, high levels of substance use, and other psychosocial problems are common among patients with psychotic disorders ( 24 ). One might expect that these challenges and other patient-level risk factors would impair adherence across all treatments in a patient's regimen, muting intrapatient variation in medication use. However, in this large, national sample of patients with schizophrenia who had diabetes and hypertension, we found that patients' adherence to their antipsychotic regimen was only moderately correlated with adherence to regimens for diabetes and hypertension.
After the analyses adjusted for refill length and other covariates, patients were significantly more likely to have poor adherence to their hypoglycemic and antihypertensive regimens than to their antipsychotic medications. Mental health clinicians understandably consider the management of psychotic symptoms to be extremely important in improving patients' functional status, and patients with schizophrenia may also perceive taking antipsychotic medication to be more important than taking medications for comorbid physical conditions. Unfortunately, patients with poor adherence to diabetes and hypertension treatments are at increased risk of serious adverse outcomes, including kidney failure, blindness, stroke, and heart disease.
Patients with several co-occurring conditions, such as those in this study, often see multiple providers, and this may lead to inconsistent communication about their self-care and medication management. In the VA, most prescriptions for antipsychotic agents are written by psychiatrists, whereas most antihypertensive and diabetes medication prescriptions are written by primary care providers. Some VA facilities have coordinated physical and psychiatric services for patients with serious mental illness, although most facilities do not. For patients with mental illness and one or more comorbid physical conditions, VA care is likely more integrated than care in many health care settings, because all VA providers have access to a common electronic medical record that includes all pharmacy data and patients use an integrated pharmacy for all of their treatments. Patients treated in health systems with poorer treatment coordination may experience even greater differences in their adherence behavior across drug classes. Concurrent management by multiple prescribers with poor coordination may negatively impact patients' therapeutic alliance with their clinicians—a factor that has been found to affect patients' adherence to multiple drug types ( 15 , 32 , 33 , 34 ).
On average, patients received fewer days' supply of their antipsychotic medication than their other medication types, and the pattern of effects in our nested models suggests that this may be one of the reasons for observed lower levels of adherence with antipsychotic therapy than with other therapies in unadjusted analyses. The link between adherence problems and shorter supplies may reflect greater opportunities to detect poor adherence when more refills are required. Unfortunately, addressing this analytic problem through methods such as limiting the sample to patients with 30- or 90-day supplies of all medications in their regimen focuses on a population that is far from typical in the VA and elsewhere. Filling antipsychotic medications for 30-day periods or less avoids the problem of undetected adverse medication events and likely promotes more frequent assessments. However, short refill intervals increase the burden on patients to organize transportation, clinic appointments, and all of the concomitant administrative tasks associated with outpatient service use.
As a consequence, shorter refill intervals may be associated with an increased frequency of adherence problems because of the inconvenience and effort involved in frequent refilling. More research is needed to tease out the observed relationship between refill interval and adherence and to identify the ideal balance between refilling burden and close psychiatric follow-up for patients using antipsychotic medications.
The results of this study should be considered within the context of several limitations. MPRs measure refill rates, and refilling behavior may not necessarily reflect patients' actual medication use. Some VA patients receive services from non-VA providers, and these encounters are not available in VA data sets. However, previous studies have reported relatively limited cross-system use of mental health services among VA mental health users ( 35 , 36 ). Many patients exclusively use the VA pharmacy because of the relatively generous prescription benefit ( 27 ), so non-VA medication refilling is unlikely to drive the pattern of effects we observed.
Because of its large population of patients with chronic mental illness and detailed electronic pharmacy data, the VA is one of the only health care systems in the country with the data necessary for a study such as this. Nevertheless, VA patients are predominantly male, with low socioeconomic status and a high prevalence of comorbid chronic conditions. As a consequence, findings about these patients and their medication adherence behaviors may not generalize to other treatment settings. It would be useful to repeat this study with a non-VA sample to determine whether the levels of adherence and the differences in adherence across therapeutic classes are similar to those reported here.
Three-medication regimens are common for patients with hypertension, and 36% of patients using both antipsychotics and antihyperensives were excluded because they used three or more antihypertensive medications. Among patients using medication for both schizophrenia and diabetes, 14% were excluded from the current study because they were using three or more medications for one of these conditions. As three-medication regimens become increasingly standard for patients who have poorly controlled disease, adherence measures based on refills will need to be expanded to reliably identify patients experiencing problems.
Conclusions
Patients with schizophrenia and comorbid diabetes and hypertension appeared to be selective about the medications that they did and did not use as prescribed. After analyses adjusted for days' supply, patients appeared to be more adherent with their antipsychotic medications than medications for their other conditions. This intrapatient variation in adherence may reflect the greater value placed on controlling symptoms of schizophrenia or greater emphasis on mental health medications by their clinicians. This study provides some insights into medication characteristics that may influence regimen adherence for patients with multiple chronic health problems. Clinicians should carefully consider characteristics of medication regimens, including the refill interval, in designing treatment plans that minimize adherence problems.
Acknowledgments and disclosures
This study was supported by the Department of Veterans Affairs Health Services Research and Development Service. John Piette is a VA Research Career Scientist. Michele Heisler is a VA Career Development awardee.
The authors report no competing interests.
1. Robinson D, Woerner MG, Alvir JM, et al: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of General Psychiatry 56:241-247, 1999Google Scholar
2. Rubin RR: Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. American Journal of Medicine 118(suppl):27S-34S, 2005Google Scholar
3. Stephenson J: Noncompliance may cause half of antihypertensive drug "failures." JAMA 282:313-314, 1999Google Scholar
4. Viguera AC, Baldessarini RJ, Hegarty JD, et al: Clinical risk following abrupt and gradual withdrawal of maintenance neuroleptic treatment. Archives of General Psychiatry 54:49-55, 1997Google Scholar
5. Valenstein M, Copeland LA, Blow FC, et al: Pharmacy data identifies poorly adherent patients at increased risk for admission. Medical Care 40:630-639, 2002Google Scholar
6. Gilmer TP, Dolder CR, Lacro JP et al: Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. American Journal of Psychiatry 161:692-699, 2004Google Scholar
7. Weiden PJ, Kozma C, Grogg A, et al: Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services 55:886-891, 2004Google Scholar
8. Osterberg L, Blaschke T: Adherence to medication. New England Journal of Medicine 353:487-497, 2005Google Scholar
9. Valenstein M, Blow FC, Copeland LA, et al: Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophrenia Bulletin 30:255-264, 2004Google Scholar
10. Cramer JA, Rosenheck R: Enhancing medication compliance for people with serious mental illnesses. Journal of Nervous and Mental Disease 187:53-55, 1999Google Scholar
11. Fenton WS, Blyler CR, Heinssen RK: Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophrenia Bulletin 23:637-651, 1997Google Scholar
12. McCombs JS, Nichol MB, Stimmel GL, et al: Use patterns for antipsychotic medications in Medicaid patients with schizophrenia. Journal of Clinical Psychiatry 60:5-11, 1999Google Scholar
13. Adherence to long term therapies: evidence for action. Geneva, World Health Organization, 2003Google Scholar
14. DiMatteo MR: Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care 42:200-209, 2004Google Scholar
15. Lacro JP, Dunn LB, Dolder CR, et al: Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. Journal of Clinical Psychiatry 63:892-909, 2002Google Scholar
16. Horne R, Weinman J: Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic illness. Journal of Psychosomatic Research 47:555-567, 1999Google Scholar
17. Goldman D, Joyce GF, Escarce JJ, et al: Pharmacy benefits and the use of drugs by the chronically ill. JAMA 291:2344-2350, 2004Google Scholar
18. Martin BC, McMillan JA: The impact of implementing a more restrictive prescription limit on Medicaid recipients: effects on cost, therapy, and out-of-pocket expenditures. Medical Care 34:686-701, 1996Google Scholar
19. Piette JD, Heisler M, Horne R, et al: A conceptually-based approach to understanding chronically-ill patients' responses to medication cost pressures. Social Science and Medicine 62:846-857, 2006Google Scholar
20. Redelmeier DA, Tan SH, Booth GL: The treatment of unrelated disorders in patients with chronic medical diseases. New England Journal of Medicine 338:1516-1520, 1998Google Scholar
21. McKeller J, Humphreys KH, Piette JD: Does depression's effect on diabetes self-care behaviors explain the relationship between depressive symptoms and subsequent diabetes-related physical symptoms? Diabetes Educator 30:485-492, 2004Google Scholar
22. Buchanan RW, Strauss ME, Kirkpatrick B, et al: Neuropsychological impairments in deficit vs nondeficit forms of schizophrenia. Archives of General Psychiatry 51:804-811, 1994Google Scholar
23. Wykes T, Reeder C, Corner J, et al: The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophrenia Bulletin 25:291-307, 1999Google Scholar
24. Aleman A, Hijman R, de Haan EH, et al: Memory impairment in schizophrenia: a meta-analysis. American Journal of Psychiatry 156:1358-1366, 1999Google Scholar
25. Hobart MP, Goldberg R, Bartko JJ, et al: Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia: II. convergent/discriminant validity and diagnostic group comparisons. American Journal of Psychiatry 156:1951-1957, 1999Google Scholar
26. Jeste SD, Patterson TL, Palmer BW, et al: Cognitive predictors of medication adherence among middle-aged and older outpatients with schizophrenia. Schizophrenia Research 63:49-58, 2003Google Scholar
27. Piette JD, Heisler M: Problems due to medication costs among VA and non-VA patients with chronic illnesses. American Journal of Managed Care 10:861-868, 2004Google Scholar
28. Blow FC, McCarthy JF, Valenstein M, et al: Care in the VHA for Veterans With Psychoses 2000: National Psychosis Registry (2nd Annual Report). Ann Arbor, Mich, VHA Health Services Research and Development, 2001Google Scholar
29. Steiner JF, Koepsell TD, Fihn SD, et al: A general method of compliance assessment using centralized pharmacy records. Medical Care 26:814-823, 1988Google Scholar
30. McCarthy JF, Blow FC: Older patients with serious mental illness: sensitivity to distance barriers for outpatient care. Medical Care 42:1073-1080, 2004Google Scholar
31. Littell RC, Milliken GA, Troup WW, et al: SAS Systems for Mixed Models. Cary, NC, SAS Institute, 1996Google Scholar
32. Piette JD, Heisler M, Krein S, et al: The role of physician trust as a buffer against medication non-adherence due to cost pressures. Archives of Internal Medicine 165:1749-1755, 2005Google Scholar
33. Day JC, Bentall RP, Roberts C, et al: Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Archives of General Psychiatry 62:717-724, 2005Google Scholar
34. Loffler W, Kilian R, Toumi M, et al: Schizophrenic patients' subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry 36:105-112, 2003Google Scholar
35. Desai RA, Rosenheck RA: The impact of managed care on cross-system use of mental health services by veterans in Colorado. Psychiatric Services 53:1599-1604, 2002Google Scholar
36. Hoff RA, Rosenheck RA: Cross-system service use among psychiatric patients: data from the Department of Veterans Affairs. Journal of Behavioral Health Services Research 27:98-106, 2000Google Scholar



