Antidepressant Utilization in British Columbia From 1996 to 2004: Increasing Prevalence but Not Incidence
Antidepressants comprise the fourth largest therapeutic category of global pharmaceutical sales, accounting for more than $20 billion in sales in 2004 (U.S. dollars) ( 1 ). Studies have shown that the prevalence of antidepressant use in North American and European populations generally has increased over time ( 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 ). Such studies typically qualify the volume of prescriptions or the type of drugs received by populations ( 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 ), often using standardized dose measures (such as the World Health Organization's Defined Daily Dose) to gauge population prevalence ( 2 , 7 , 9 , 10 , 11 ). Relatively few studies have used patient-specific definitions to measure population-level prevalence ( 4 , 5 , 6 , 8 , 10 , 11 , 12 ) or assessed both incident and prevalent antidepressant users ( 4 , 11 , 12 ).
As expenditures for antidepressants continue to increase with time, driven by increases in prescription volume consumed by populations, analyses of both prevalent and incident users will improve our understanding of utilization and appropriateness. Information about the characterization of new users is especially important in understanding changes in the burden of depression (however severe) and predicting future utilization trends. Moreover, detailed descriptions of population drug use will serve as a background for future studies of effectiveness. The objectives of this study were to investigate both the prevalence and incidence of antidepressant use across age and socioeconomic strata as well as by drug class in British Columbia, Canada, by using a comprehensive and population-based prescription drug database.
Methods
This study employed a population-based, person-specific data set that contained prescription dispensation records and demographic information for approximately 4.1 million residents living in British Columbia from 1996 to 2004 (calendar years). Data describing prescription drug utilization were extracted from the British Columbia PharmaNet system. PharmaNet is a computer network linking all pharmacies in the province. Provincial law requires that information from every prescription dispensed at retail pharmacies for residents living in the community or within long-term care facilities must be entered into this database. Information extracted for this study included the following fields: date, anonymized patient identifier, drug quality, and drug identifier.
Drug identifiers were then linked to the World Health Organization's Anatomical Therapeutic Chemical (ATC) classification codes. Antidepressants were divided into five classes according to ATC codes as follows: tricyclic antidepressants (N06AA: amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, and trimipramine), selective serotonin reuptake inhibitors (SSRIs) (N06AB: citalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline), novel agents (N06AX: nefazodone, trazodone, tryptophan, mirtazapine, venlafaxine, and bupropion), monoamine oxidase inhibitors (MAOIs) (N06AG and N06AF: moclobemide, phenelzine, and tranylcypromine), and bupropion for smoking cessation (N07BA02). Escitalopram was not marketed in Canada at the time of this analysis.
Anonymized patient identifiers were linked to population registries to obtain sociodemographic information and relevant population denominators. The study cohort consisted of every resident eligible for the provincially administered, universal public health insurance (British Columbia Medical Services Plan). This excludes First Nations people (indigenous people), veterans, and Royal Canadian Mounted Police (total excluded: 4% of the population). Sociodemographic information included age, sex, and a measure of socioeconomic status. The measure of socioeconomic status used was the median census-reported income for households within the neighborhood of a given resident. The population was divided into quintiles ranging from those living in the lowest-income neighborhoods to those living in the highest-income neighborhoods.
For 1996 through 2004 we calculated the quarterly prevalence of antidepressant use per 1,000 inhabitants, stratified by age, socioeconomic status, and drug class. Prevalent antidepressant users were individuals who filled at least one prescription for an antidepressant in the given quarter. Individuals filling prescriptions for more than one type of antidepressant (for example, fluoxetine and venlafaxine) within a given quarter were counted as one user of each type of antidepressant. Denominators included all individuals in the study cohort during the period of interest, stratified by age and socioeconomic status as necessary.
For 1996 through 2004 we calculated the quarterly incidence of antidepressant use per 1,000 inhabitants, stratified by age, sex, socioeconomic status, and drug class. Incident antidepressant users were individuals who resided within the province for at least 275 days of each of two years before filling their first-ever prescription for an antidepressant. The two-year residency requirement ensured that "incident users" were residents of British Columbia who had not previously filled an antidepressant prescription for at least a two-year period. Denominators for the incidence calculation included all individuals who satisfied an equivalent residency requirement—had resided in the province for at least 275 days of each of two years before the year of interest.
Time-series analysis was utilized to assess trends in incident and prevalent antidepressant use. Autocorrelation in the error term was assessed and the optimal model selected. One p value was reported per model, with significant (p<.05) models indicating a significant change in use with time. All analyses were conducted in SAS version 8.0 using SAS/ETS. The University of British Columbia Behavioural Research Ethics Board approved this study.
Results
Prevalence
As shown in Figure 1 , between 1996 and 2004, quarterly period prevalence of antidepressant use increased from 34.8 to 71.6 per 1,000 population. Although prevalence of antidepressant use generally increased with age (p<.05 for all age groups), prevalence was higher among residents aged 45 to 64 than among residents aged 65 to 84 from 1999 onward. Prevalence increased between the first quarter of 1996 and the last quarter of 2004 for all age groups but did so at different rates. Among adults, it increased by 58% for residents older than 85 years (from 75.1 to 118.4 per 1,000 population), by 80% for residents aged 65 to 84 years (55.9 to 100.8 per 1,000 population), by 95% for residents aged 45 to 64 years (56.5 to 110.4 per 1,000 population), and by 93% for residents aged 20 to 44 (34.9 to 67.2 per 1,000 population). Prevalence among the pediatric age group (19 years or younger) increased from 4.5 per 1,000 in the beginning of 1996, to a maximum of 10.7 per 1,000 at the end of 2003, and then declined to 9.1 per 1,000 by the end of 2004. The total change in prevalence among the pediatric group was 102%.
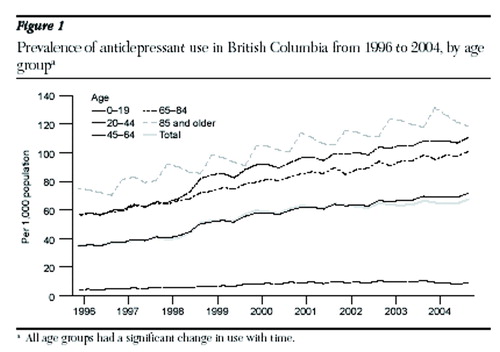
When analyzed by socioeconomic status, all groups demonstrated increased prevalent use with time (p<.05 for all socioeconomic strata). A socioeconomic gradient was observed in prevalent antidepressant use, with a tendency for lower socioeconomic status groups to have higher prevalence of exposure. The lowest income quintile demonstrated the greatest prevalence of antidepressant use both at the beginning and end of the study period (46.5 and 87.0 per 1,000) and the two highest income quintiles, the least antidepressant use (30.2 and 32.6 per 1,000 at the first quarter and 63.9 and 64.0 per 1,000 at the last quarter for the fourth and fifth income quintiles, respectively). [A figure showing the prevalence of antidepressant use by socioeconomic status is available as an online supplement at ps.psychiatryonline.org.]
Analysis of antidepressant use by drug class over time revealed a changing practice pattern. The novel group of antidepressants demonstrated the greatest increase in prevalence over time. In early 1996 the relative proportions of all the prevalent antidepressant users (N=131,586) was 47% (61,999 persons) for SSRIs, 37% (48,401 persons) for tricyclic antidepressants, and 13% (17,198 persons) for novel agents, and in late 2004 that pattern of prevalent users (N=287,391) had shifted to 48% (137,157 persons) for SSRIs, 17% (49,025 persons) for tricyclic antidepressants, and 33% (94,739 persons) for novel agents.
The prevalence of use of the novel group of antidepressants increased from 4.5 to 23.6 per 1,000 population between early 1996 and late 2004 (p<.05). Use of SSRIs also increased throughout the study period, from 16.4 to 34.2 per 1,000 (p<.05). Use of tricyclic antidepressants was constant over the study period, 12.8 and 12.2 per 1,000 at the first and last quarters (p<.05). The prevalence of MAOI use decreased from 1.1 to .3 per 1,000 during the study period (p< .05). Finally, although not used as an antidepressant, bupropion for smoking cessation was included separately in the analysis. At first Canadian launch, in the third quarter of 1998, this drug was widely and rapidly adopted, among 2.76 per 1,000 British Columbians. Population prevalence peaked in the first quarter of 1999 (7.1 per 1,000) and declined over time to 1.3 per 1,000 at the end of 2004, although this finding was not significant. [A figure showing the prevalence of antidepressant use by drug class is available as an online supplement at ps.psychiatryonline.org.]
Incidence
As shown in Table 1 , between 1998 and 2004 a total of 575,858 individuals who met our inclusion criteria filled first prescriptions for antidepressants. The quarterly incidence of antidepressant use increased dramatically from 6.5 per 1,000 at the beginning of 1998 to peak at 11.3 per 1,000 at the beginning of 1999. This was followed by a decline to 4.2 per 1,000 by the end of 2004 ( Figure 2 ). All adult age groups (groups consisting of those older than 19 years) displayed a similar pattern of incident use over time, with a peak in early 1999 and a gradual decrease to the end of the study period. Residents aged from 20 to 64 years displayed the most pronounced peak in incident antidepressant use in 1999 (p<.05 for all adult age groups). Pediatric residents (19 years or younger) displayed different patterns of incident use compared with adults. The lowest quarterly incident use of antidepressants was among residents younger than nine years, with .9 users per 1,000 population in the first quarter of 1998 and .4 users per 1,000 in the fourth quarter of 2004 (p<.05). Quarterly incident antidepressant use among residents aged ten to 19 years was much higher and declined slightly over the same period (from 3.2 to 2.7 per 1,000, although this finding was not significant). Incident antidepressant use among females increased from 8.0 per 1,000 at the beginning of the study to peak at the beginning of 1999 at 12.4 per 1,000 and declined to 4.8 per 1,000 at the end of 2004. At the same time points, the incidence of antidepressant prescribing for males was 4.9, 10.1, and 3.6 per 1,000.
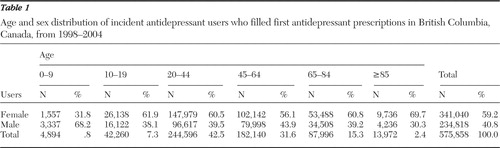 |
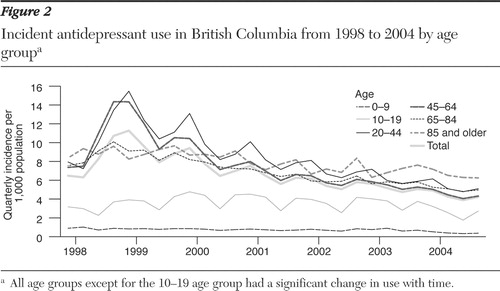
We observed a socioeconomic gradient in incident antidepressant prescribing, with the lowest income quintile demonstrating the highest incidence of use (7.8 versus 5.5 per 1,000 at the beginning of the study, 12.8 versus 9.6 per 1,000 at the first quarter of 1999, and 4.4 versus 4.1 per 1,000 at the end of the study for the first and fifth quintiles, respectively) (p<.05 for all socioeconomic strata). Incident bupropion use increased dramatically in early 1999 (from 2.4 per 1,000 at market launch in the third quarter of 1998, peaking at 5.2 per 1,000 in the first quarter of 1999) and then gradually declined though the end of 2004 (p<.05). [A figure showing the incidence of antidepressant use by socioeconomic status is available as an online supplement at ps.psychiatryonline.org.]
Except for late 1998 and early 1999, when bupropion for smoking cessation incidence was greatest, incident SSRI prescribing was consistently highest, although the quarterly incidence declined through the study period from 3.3 to 1.6 per 1,000 (p<.05). The quarterly incidence of tricyclic antidepressant use also decreased from 2.3 to 1.1 per 1,000 (p<.05). Conversely, the quarterly incidence of novel agents increased over time from .8 to 1.2 per 1,000 (p<.05). [A figure showing the incidence of antidepressant use by drug class is available as an online supplement at ps.psychiatryonline.org.]
Discussion
Utilizing a comprehensive, population-based prescription drug database containing data on all prescriptions filled in British Columbia, we observed an increase in prevalent antidepressant use from 1996 to 2004. Like others who evaluated the nature of drug use within the class of antidepressants, we observed that the increase in prevalence of antidepressant use over time was largely associated with a shift from tricyclic antidepressants to SSRIs and novel agents ( 2 , 3 , 5 , 7 , 9 , 15 , 16 ). By 2004, overall, 7.2% of the entire population of British Columbia had filled a prescription for an antidepressant. Trends in prevalent antidepressant use among British Columbians were not mirrored by trends in incident antidepressant use. There was an upward trend in new antidepressant use in early 1999, accounted for by new prescriptions for bupropion for smoking cessation, but overall, incident antidepressant use declined over time. This suggests that the trajectory of increasing prevalence in antidepressant use over time could have been much greater by 2004, had antidepressant initiation continued at 1999 rates.
Several possible explanations for the increase in prevalent users over time include the expansion of therapeutic indications for antidepressants to include conditions such as anxiety disorders ( 17 , 18 ), neuropathic pain ( 19 ), smoking cessation ( 20 ), and premenstrual dysphoric disorder ( 21 ), as well as continued or expanding off-label use for sleep, migraines, and fibromyalgia ( 22 ). Patients and practitioners may be influenced by direct-to-consumer advertising of antidepressants ( 23 ). Another possibility could be that duration of depression and treatment of depression are increasing with time ( 24 , 25 ). There may be increased clinician awareness and adherence to the growing evidence base that recommends continued antidepressant use for severe or recurrent depression ( 26 , 27 ). The improved tolerability of newer antidepressants marketed throughout the 1990s may have increased patient willingness to take and persist with therapy or increased prescriber willingness to utilize such therapies for more medically complex patients at extremes of age ( 6 , 28 , 29 ).
The increase in incident antidepressant use observed in late 1999 corresponded with the launch of bupropion for smoking cessation in Canada ( 30 ); however, this phenomenon was short-lived, and incident antidepressant use declined throughout the study period. Perhaps the observed decline in new use of antidepressants after 1999 represents a saturation effect—those who would have been started on an antidepressant had already been started, thus creating a declining incidence. Several events may have contributed to the decline in incident antidepressant use over time, including the withdrawal of nefazodone resulting from hepatotoxicity ( 31 ), public concern about dependence, withdrawal and discontinuation syndromes ( 32 ), and self-harm behavior associated with antidepressants ( 33 ).
Persistence with therapy may further contribute to the different patterns observed between prevalent and incident antidepressant use. The prevalent users included all users who had been taking an antidepressant before the quarter of interest, as well as incident users for that quarter. Although it is known that adherence to antidepressants is poor ( 34 , 35 ), this study suggests that a large proportion of antidepressant users are occasional or intermittent users for long periods of time. Age could further contribute to the different patterns of use, as persistence with medications generally increases with age ( 34 ), as do the number of (nondepressive) indications for antidepressant prescribing ( 36 ).
Our findings are consistent with those of other recent Canadian studies that assessed antidepressant prevalence ( 5 , 6 , 37 , 38 , 39 ). In a recent study, Beck and colleagues ( 37 ) found that in 2002, 5.8% of Canadians aged 15 years and older who responded to the Canadian Community Health Survey (CCHS) self-reported the use of antidepressant drugs for any indication in the past 12 months; over the same period, our data show 6.1% to 6.3% of British Columbians of all ages filled a prescription for an antidepressant. Our results are similar to those of Mamdani and colleagues ( 5 ), who observed that 10.9% of Ontario seniors had filled a prescription for an antidepressant by the end of 2002; at this time point we observed that 9.4% of British Columbians aged 65 to 85 years and 11.1% of those older than 85 years filled an antidepressant prescription. In Manitoba, Fransoo and colleagues ( 38 ) observed that 6.5% of Manitobans—8.6% of females and 4.5% of males—filled at least two prescriptions for antidepressants in 2003 through 2004 (age adjusted to reflect the population of Manitoba). In 1996-1997 through 1998-1999, 4.3% of Manitobans filled at least two prescriptions for antidepressants (age and sex adjusted) ( 39 ); this prevalence increased to 5.5% in 1999-2000 through 2000-2001 ( 39 ).
Although incident use of antidepressants was higher among middle-aged populations, prevalent use increased with age. We observed that the greatest prevalent use was among those older than 85 years and the greatest peak in incident use occurred among those aged 20 to 64 years. It is possible that the use of bupropion for smoking cessation explains these patterns of use. Several authors have examined the use of antidepressants by age groups and have found increasing use with increasing age ( 8 , 9 , 11 , 12 , 36 , 40 ), an increase in use through middle age (ages 46 to 65 years) with a decline among patients older than 65 years ( 15 , 37 ), or a decline in use among patients older than 85 years ( 41 ). Variability in study duration, study year, and age categories likely accounts for the variability in age patterns of antidepressant use. Our findings are consistent with those of the only other Canadian study that looked at antidepressant use by age categories, although the study examined only a single time point ( 37 ).
We observed a socioeconomic gradient in antidepressant prescribing, in which those with the lowest socioeconomic status had a greater incidence and prevalence of antidepressant utilization, compared with those with the highest socioeconomic status, consistent with that observed with 2002 CCHS data ( 37 ) and with the expectation that those with lower socioeconomic status would have a greater burden of disease ( 42 , 43 ). However, others did not observe a clear socioeconomic gradient in prevalent antidepressant use ( 38 ).
Our analysis is subject to several limitations. First, the definition of incident antidepressant users may misclassify individuals as incident users if they had previously used and discontinued an antidepressant more than two years before the incident prescription. It may also miss individuals who used only samples given to them by physicians because that information does not appear in the PharmaNet data. Second, studies that utilize prescription drug databases assess only prescriptions that were filled, not prescriptions that were written.
Conclusions
We have shown that prevalence of antidepressant use in an entire population has increased dramatically from 1996 to 2004, whereas incidence increased from 1998 to 1999 but then decreased through 2004. Many complex factors likely contribute to prescribing patterns of antidepressants in populations. Future studies could utilize the British Columbia prescription drug data to observe patterns of persistence with antidepressants in order to further explain the differences observed between prevalent and incident users.
Acknowledgments and disclosures
This research was supported by the Canadian Institute for Health Research.
The authors report no competing interests.
1. Leading Therapy Classes by Global Pharmaceutical Sales, 2004. IMS Health. Available at www.imshealth.com/ims/portal/front/articleC/0,2777,65997123402471234109,00.html. Accessed July 31, 2006Google Scholar
2. Guaiana G, Andretta M, Corbari L, et al: Antidepressant drug consumption and public health indicators in Italy, 1955 to 2000. Journal of Clinical Psychiatry 66:750-755, 2005Google Scholar
3. Hemels ME, Koren G, Einarson TR: Increased use of antidepressants in Canada: 1981-2000. Annals of Pharmacotherapy 36:1375-1379, 2002Google Scholar
4. Isacsson G, Boethius G, Henriksson S, et al: Selective serotonin reuptake inhibitors have broadened the utilisation of antidepressant treatment in accordance with recommendations: findings from a Swedish prescription database. Journal of Affective Disorders 53:15-22, 1999Google Scholar
5. Mamdani M, Rapoport M, Shulman KI, et al: Mental health-related drug utilization among older adults: prevalence, trends, and costs. American Journal of Geriatric Psychiatry 13:892-900, 2005Google Scholar
6. Mamdani MM, Parikh SV, Austin PC, et al: Use of antidepressants among elderly subjects: trends and contributing factors. American Journal of Psychiatry 157:360-367, 2000Google Scholar
7. Mant A, Rendle VA, Hall WD, et al: Making new choices about antidepressants in Australia: the long view 1975-2002. Medical Journal of Australia 181(suppl):S21-S24, 2004Google Scholar
8. Middleton N, Gunnell D, Whitley E, et al: Secular trends in antidepressant prescribing in the UK, 1975-1998. Journal of Public Health and Medicine 23:262-267, 2001Google Scholar
9. Poluzzi E, Motola D, Silvani C, et al: Prescriptions of antidepressants in primary care in Italy: pattern of use after admission of selective serotonin reuptake inhibitors for reimbursement. European Journal of Clinical Pharmacology 59:825-831, 2004Google Scholar
10. Rosholm JU, Gram LF, Isacsson G, et al: Changes in the pattern of antidepressant use upon the introduction of the new antidepressants: a prescription database study. European Journal of Clinical Pharmacology 52:205-209, 1997Google Scholar
11. Rosholm JU, Andersen M, Gram LF: Are there differences in the use of selective serotonin reuptake inhibitors and tricyclic antidepressants? A prescription database study. European Journal of Clinical Pharmacology 56:923-929, 2001Google Scholar
12. Van Eijk ME, Bahri P, Dekker G, et al: Use of prevalence and incidence measures to describe age-related prescribing of antidepressants with and without anticholinergic effects. Journal of Clinical Epidemiology 53:645-651, 2000Google Scholar
13. Roberts E, Norris P: Growth and change in the prescribing of anti-depressants in New Zealand: 1993-1997. New Zealand Medical Journal 114:25-27, 2001Google Scholar
14. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203-209, 2002Google Scholar
15. Lawrenson RA, Tyrer F, Newson RB, et al: The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. Journal of Affective Disorders 59:149-157, 2000Google Scholar
16. Pirraglia PA, Stafford RS, Singer DE: Trends in prescribing of selective serotonin reuptake inhibitors and other newer antidepressant agents in adult primary care. Primary Care Companion to the Journal of Clinical Psychiatry 5:153-157, 2003Google Scholar
17. Fricchione G: Clinical practice: generalized anxiety disorder. New England Journal of Medicine 351:675-682, 2004Google Scholar
18. Stein MB: Advances in recognition and treatment of social anxiety disorder: a 10-year retrospective. Psychopharmacology Bulletin 37(suppl 1):97-107, 2003Google Scholar
19. Sindrup SH, Otto M, Finnerup NB, et al: Antidepressants in the treatment of neuropathic pain. Basic and Clinical Pharmacology and Toxicology 96:399-409, 2005Google Scholar
20. Hughes J, Stead L, Lancaster T: Antidepressants for smoking cessation. Cochrane Database of Systematic Reviews CD 000031, 2004Google Scholar
21. Freeman EW: Effects of antidepressants on quality of life in women with premenstrual dysphoric disorder. Pharmacoeconomics 23:433-444, 2005Google Scholar
22. Stone KJ, Viera AJ, Parman CL: Off-label applications for SSRIs. American Family Physician 68:498-504, 2003Google Scholar
23. Kravitz RL, Epstein RM, Feldman MD, et al: Influence of patients' requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA 293:1995-2002, 2005Google Scholar
24. Judd LL, Paulus MJ, Schettler PJ, et al: Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry 157:1501-1504, 2000Google Scholar
25. Patten SC: The duration of major depressive episodes in the Canadian general population. Chronic Diseases in Canada 22:6-11, 2001Google Scholar
26. Kennedy SH, Lam RW, Cohen NL, et al: Clinical guidelines for the treatment of depressive disorders. IV: medications and other biological treatments. Canadian Journal of Psychiatry 46(suppl 1):38S-58S, 2001Google Scholar
27. Mann JJ: The medical management of depression. New England Journal of Medicine 353:1819-1834, 2005Google Scholar
28. Geddes JR, Freemantle N, Mason J, et al: SSRIs versus other antidepressants for depressive disorder. Cochrane Database of Systematic Reviews CD001851, 2000Google Scholar
29. Williams JW Jr, Mulrow CD, Chiquette E, et al: A systematic review of newer pharmacotherapies for depression in adults: evidence report summary. Annals of Internal Medicine 132:743-756, 2000Google Scholar
30. Hebert S: Bupropion (Zyban, sustained-release tablets): reported adverse reactions. Canadian Medical Association Journal 160:1050-1055, 1999Google Scholar
31. Choi S: Nefazodone (Serzone) withdrawn because of hepatotoxicity. Canadian Medical Association Journal 169:1187, 2003Google Scholar
32. Nutt DJ: Death and dependence: current controversies over the selective serotonin reuptake inhibitors. Journal of Psychopharmacology 17:355-364, 2003Google Scholar
33. Fergusson D, Doucette S, Glass KC, et al: Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. British Medical Journal 330:396, 2005Google Scholar
34. Krueger KP, Berger BA, Felkey B: Medication adherence and persistence: a comprehensive review. Advances in Therapy 22:313-356, 2005Google Scholar
35. Maddox JC, Levi M, Thompson C: The compliance with antidepressants in general practice. Journal of Psychopharmacology 8:48-53, 1994Google Scholar
36. Percudani M, Barbui C, Fortino I, et al: Antidepressant drug prescribing among elderly subjects: a population-based study. International Journal of Geriatric Psychiatry 20:113-118, 2005Google Scholar
37. Beck CA, Patten SB, Williams JV, et al: Antidepressant utilization in Canada. Social Psychiatry and Psychiatric Epidemiology 40:799-807, 2005Google Scholar
38. Fransoo R, Martens P, Burland E, et al: Sex Differences in Health Status, Health Care Use, and Quality of Care: A Population-Based Analysis for Manitoba's Regional Health Authorities. Winnipeg, MB, Manitoba Centre for Health Policy, 2005Google Scholar
39. Martens P, Fransoo R, Burland E, et al: The Manitoba RHA Indicators Atlas: Population-Based Comparison of Health and Health Care Use. Winnipeg, MB, Manitoba Centre for Health Policy, 2003Google Scholar
40. Barbui C, Broglio E, Laia AC, et al: Cross-sectional database analysis of antidepressant prescribing in Italy. Journal of Clinical Psychopharmacology 23:31-34, 2003Google Scholar
41. Pietraru C, Barbui C, Poggio L, et al: Antidepressant drug prescribing in Italy, 2000: analysis of a general practice database. European Journal of Clinical Pharmacology 57:605-609, 2001Google Scholar
42. Marmot MG, Shipley MJ, Rose G: Inequalities in death—specific explanations of a general pattern? Lancet 1:1003-1006, 1984Google Scholar
43. Marmot MG, Kogevinas M, Elston MA: Social/economic status and disease. Annual Review in Public Health 8:111-135, 1987Google Scholar



