Personality Disorders and Unmet Needs Among Psychiatric Inpatients
The measurement of needs has become increasingly important to mental health professionals. For example, it is now recognized that in the management of schizophrenia, needs assessment is complementary to clinical evaluation ( 1 ). There is agreement on the importance of capturing consumer perspectives on illness ( 2 ), and assessment of need builds on the work of Maslow ( 3 ), who described a "hierarchy of needs" extending from basic physiological needs to "self-actualization" needs.
In a mental health context, needs include broad domains of health and social functioning, which are necessary to survive and prosper in the community. Needs can be assessed from different perspectives, including staff, patient, or caregiver, and have been differentiated into unmet needs (current serious problems whether or not help is given) and met needs (no or moderate problems because of help given) ( 4 ). In the United Kingdom, the "ability to benefit" from health care interventions is an essential component of the U.K. Department of Health's definition of need ( 5 ).
Internationally, the Camberwell Assessment of Need (CAN) ( 4 ) is the most widely used need assessment ( 1 , 6 , 7 , 8 , 9 ), and studies using the CAN suggest that a policy of actively assessing and addressing patient-rated unmet needs may lead to improved quality of life ( 10 ). Nevertheless, surveys with standardized assessments have found high levels of unmet need in populations of people with mental illness ( 11 , 12 ), suggesting that needs are sometimes overlooked by informal needs assessment ( 13 ). In addition, although community studies consistently record high rates of psychiatric disorders, it is not clear to what extent these rates reflect the met or unmet need for treatment ( 14 ). This uncertainty is particularly the case for personality disorders; recent estimates of community prevalence in the United States are as high as 15 percent ( 15 ).
Patients with personality disorders certainly place a high demand on health and social services ( 16 , 17 , 18 ). One explanation for this high demand might be that such patients have a significantly greater number of unmet needs. However, no studies have examined the association between personality disorders and need. We set out to examine the association between unmet need and personality disorders in a sample of psychiatric inpatients from the United Kingdom. We tested the hypothesis that among psychiatric inpatients, the presence of a personality disorder would be independently associated with a significantly greater mean number of unmet needs.
Methods
Sample
We followed standard data collection protocols approved by the internal review board of the Maudsley Hospital research ethics committee. The study was conducted across four mixed-sex, general adult acute psychiatry wards serving an inner-city borough of London. The wards were divided between two hospital sites, and recruitment took place between April and August 2004. All inpatients during the study period were eligible for inclusion. Patients who were unable to complete an interview in English were excluded, as were those too disturbed to cooperate with a research interview. Potential participants were given written and verbal information about the study, and written informed consent was obtained. Each participant received £10 ($17.50) for taking part in the study. A total of 345 people were inpatients during the course of the study. Over the study period, 97 patients left the wards before they could be invited to participate, 15 patients did not speak sufficient English, and nine patients were too disturbed, which left a potential pool of 224 patients, of whom 153 (68 percent) took part in the study.
Assessments
The first author evaluated all participants. Sociodemographic data were obtained. The Duke-UNC Functional Social Support Questionnaire ( 19 ) was included, because we anticipated that social support might confound an association between personality disorders and unmet need. The questionnaire measures social support by using eight five-category Likert-format questions; possible scores range from 8 to 40, with higher scores indicating poor social support. The Camberwell Assessment of Need Short Assessment Schedule (CANSAS) ( 4 ) assesses the presence of met and unmet need in 22 health and social domains (shown in Table 2 ). For each domain, patient responses are scored as unmet need (current serious problem, regardless of any help received), met need (no or moderate problem because of help given), no need, or not disclosed. The summary unmet need score is the number of domains with an unmet need; it ranges from 0 to 22, with higher scores indicating more unmet need.
 |
The Alcohol Use Disorders Identification Test (AUDIT) ( 20 ) is a ten-item screening test for alcohol use disorders that covers the domains of excessive alcohol intake, dependence, and problems related to drinking. A score between 0 and 40 is generated, with scores of 8 or more indicating harmful use of alcohol, and those of 16 or more indicating alcohol dependence. Patients completed a checklist about their use of nonprescribed drugs over the previous 12 months.
The Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) ( 21 ) was administered. The assessment of personality disorder took place at the end of the assessment of needs, in order to minimize the possibility that knowledge of personality status would bias the other clinical assessments. Patients were grouped according to the presence or absence of any personality disorder. In addition, the severity of the personality disorder was rated on the basis of Tyrer and Johnson's criteria ( 22 ). According to these criteria, severity of personality disorder can be grouped into one of four levels: no personality disorder, personality difficulty, simple personality disorder (either a single personality disorder or multiple personality disorders within the same cluster), and diffuse personality disorder (two or more personality disorders from different clusters).
After the assessment, OPCRIT ( 23 ) was used to review participants' case records to generate an axis I diagnosis based on the current illness episode ( 23 ).
Power calculation
The primary outcome variable in this study was the mean number of unmet needs. In a previous U.K. study, Boardman and colleagues ( 24 ) reported that the mean±SD number of unmet needs in a sample of acutely unwell psychiatric adult inpatients was 5±3. A prestudy power calculation indicated that use of a total sample of 150 would permit detection of a 2.5 unit increase (from 5 to 7.5) in the mean number of unmet needs among those with a personality disorder at the 5 percent level with a high probability (power greater than 80 percent).
Statistical analysis
Analyses were performed with SPSS (version 10) ( 25 ). A strategy for the statistical analysis of the association between personality disorder and unmet need was drawn up before the data were inspected. The data were initially inspected to examine the baseline characteristics of the study sample. The statistical association between mean level of unmet need and personality disorder was examined by using a t test. Associations between individual domains of need and personality disorder were examined by using chi square tests and odds ratios. Univariate associations between personality disorder and other baseline measures, and between unmet need and baseline measures, were examined by using chi square tests (categorical variables), t tests, one-way analysis of variance (for normally distributed continuous variables), and Mann-Whitney tests (for skewed continuous variables). The association between personality disorder and unmet need was examined for possible sources of confounding by using stepwise linear regression modeling. Covariates were included in the model if they were significantly associated with unmet need (p<.05) on a priori grounds (age and gender) or if the variable had previously been shown to be associated with unmet need ( 8 ).
Results
No statistically significant differences were found between the 153 participants and the 71 nonparticipants in terms of age or gender. However, compared with nonparticipants, a greater proportion of participants were voluntary patients as opposed to involuntary inpatients (χ 2 =5.28, df=1, p=.02). Participants were also more likely to have shorter hospital stays than nonparticipants (Mann-Whitney U=1,728, p=.005).
The mean±SD age of participants was 39.1±11.1 years. Ninety-three participants (61 percent) were male, and 106 participants (69 percent) were single. Sixty-nine participants (45 percent) were white, 64 (42 percent) were black, and 20 participants (13 percent) belonged to another ethnic group. Sixty-three participants (41 percent) were living alone before hospital admission. The median duration of illness was ten years, with an interquartile range of four to 21 years. Ninety-one participants (60 percent) described being in regular contact with a community mental health team before their admission. Fourteen participants (9 percent) were in their first episode of contact with psychiatric services. Participants' mean±SD score on the Duke-UNC Functional Social Support Questionnaire was 22.1±8.2. The mean number of unmet needs was 3.6±2.8.
In terms of axis I diagnoses, 40 participants (26 percent) had a schizophrenia-related disorder (schizophrenia, schizoaffective disorder, or schizophreniform disorder); 33 (22 percent), delusional disorder; 31 (20 percent), psychosis not otherwise specified; and 37 (24 percent), affective disorder (major depression, mania, or hypomania). Twelve participants (8 percent) had no axis I diagnosis. On the AUDIT questionnaire, 24 participants (16 percent) had scores indicating dependence on alcohol, 15 (10 percent) had scores indicating harmful use of alcohol, and 114 (75 percent) reported no alcohol misuse. Seventy-four participants (48 percent) had used nonprescribed drugs in the year before recruitment; 64 (42 percent) admitted using cannabis, 19 (12 percent) had used crack cocaine, 13 (8 percent) had used other forms of cocaine, and 15 (10 percent) had used heroin.
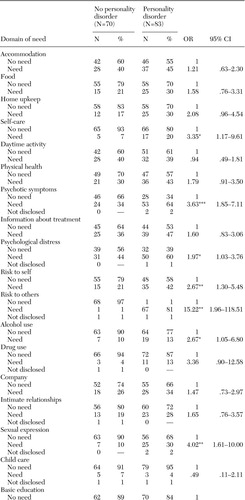
Table 1 shows the prevalence and severity of personality disorder.
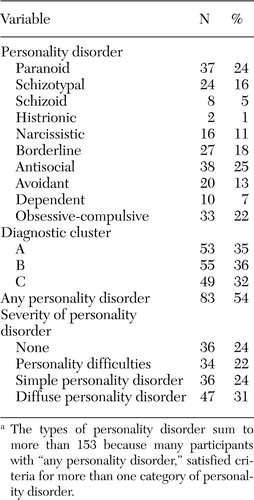 |
a The types of personality disorder sum to more than 153 because many participants with any personality disorder, satisfied criteria for more than one category of personality disorder.
Of the 153 participants, 83 (54 percent) met all DSM criteria for any type of personality disorder (referred to as any personality disorder in Table 1 ). Of these 83 participants, 36 (24 percent of the total sample) met Tyrer and Johnson's criteria ( 22 ) for simple personality disorder, and 47 (31 percent) met Tyrer and Johnson's criteria for diffuse personality disorder. Tyrer and Johnson define a diffuse disorder as meeting all DSM criteria for two or more personality disorders; the two or more disorders must be from different clusters.
The presence of a personality disorder was associated with more unmet need (t=-3.83, df=151, p<.001), but no association with met need was found. Participants with personality disorders were also more likely to report alcohol misuse (χ 2 =6.75, df=2, p=.03) and use of nonprescribed medication (χ 2 =12.43, df=1, p<.001). No statistically significant associations were found between personality disorder and any other sociodemographic or clinical variable.
Univariate associations between personality disorder and individual domains of need are presented in Table 2 . Personality disorder was significantly associated with greater need in eight of 22 domains of need: self-care, psychotic symptoms, psychological distress, risk to self, risk to others, alcohol use, sexual expression, and budgeting.
Unmet need was significantly associated with being white (F=3.38, df=2, 150, p=.04), being of no fixed abode (F=4.25, df=3, 149, p=.007), misusing alcohol (F=9.92, df=2, 150, p<.001), using nonprescribed drugs (t=-2.75, df=151, p=.007), not having regular contact with psychiatric services before admission (t=2.79, df=151, p=.006), and having poor social support (F=10.83, df=1, 151, p=.001). These variables were entered, along with severity of personality disorder, age, gender and axis I diagnosis, into a stepwise linear regression model of unmet need. The coefficients from the final regression model are shown in Table 3 . Severity of personality disorder remained significantly associated with unmet need, even after the analysis adjusted for the effects of all covariates. The model was tested for an interaction between personality disorder and alcohol misuse, but no such interaction was found.
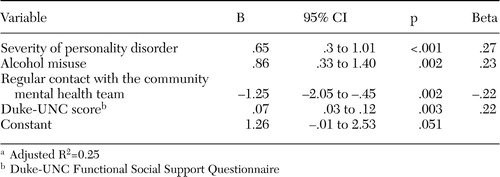 |
a Adjusted R 2 =0.25
Discussion
In this study, the presence of a personality disorder was robustly and independently associated with the number of unmet needs. The association was highly significant, and in a linear regression model, the severity of personality disorder was the strongest predictor of unmet need. Specific domains of need associated with the presence of a personality disorder were self-care, psychotic symptoms, psychological distress, risk to self, risk to others, alcohol use, sexual expression, and budgeting.
The associations between personality disorder and need in the domains of psychotic symptoms and psychological distress are consistent with research showing that the presence of a comorbid personality disorder can make mental illness more resistant to treatment ( 26 , 27 , 28 ). Personality disorder has been shown to be predictive of future violence and suicidal behavior in samples of persons with mental disorders ( 29 , 30 , 31 ). Our additional finding of a significant association between personality disorder and self-reported need in the domains of risk to self and others is consistent with this previous research and highlights the importance of thoroughly assessing for a personality disorder as part of the general risk assessment of all adult psychiatric patients.
The association of personality disorder with greater need in the domains of self-care (difficulties in keeping clean and tidy), sexual expression (dissatisfaction with sex life), and budgeting (problems in the daily management of finances) has not previously been demonstrated, and these areas are rarely identified as priorities for assessment or intervention in psychiatric treatment settings. This study identified their specific importance among persons with personality disorders, and attention should be given to ensuring that they are routinely considered in the management of individual patients as well as in needs-based service planning.
Numerous studies have examined the prevalence of personality disorders in psychiatric hospital populations, although no previous study has examined the association between personality disorder and needs. Similarly, previous psychiatric surveys of need have tended to concentrate on populations of psychotic patients and have not examined the service needs of patients with personality disorders. The overall prevalence of personality disorder in this study was 54 percent. It is difficult to compare this figure with prevalence estimates from previous studies of personality disorder from the United States or indeed the United Kingdom because of differences in sampling strategy, diagnostic criteria, and assessment methods. In addition, changes in service provision in the United Kingdom, characterized by a reduction in availability of inpatient beds, are likely to have contributed to a concentration of the most complex cases in hospitals, with consequent changes in the inpatient prevalence of personality disorder over time.
This study had important limitations. Ninety-seven patients left the wards before they could be asked to participate in the study, which highlights the mobility of the acute psychiatric inpatient population in the United Kingdom and also raises the possibility of selection bias. Nevertheless, 68 percent of those approached agreed to participate. Although there were no significant differences between participants and nonparticipants with regard to age or gender, the nonparticipants may have differed on other characteristics, which we were unable to determine. As in other studies of personality disorder that have been conducted in acutely ill populations, the diagnosis of a personality disorder may have been biased by abnormal mental state at the time of assessment ( 32 ). The association between personality disorder and need in the domain of psychotic symptoms may reflect this bias. Furthermore, such bias is likely to exaggerate the strength of some of the detected associations, because psychopathology is known to be associated with need in the domains of psychological distress, risk to self, and risk to others ( 1 ). Nevertheless, recent evidence indicates that although the diagnostic status of patients with personality disorders may change significantly over time, functional status improves less significantly ( 33 ). Such findings add weight to the argument that the needs of patients with personality disorders should be assessed early in the treatment process, as was the case in this study. In order to reduce the possibility of knowledge of personality disorder status biasing the assessment of needs, we conducted the assessment of personality after the assessment of need. However, it is possible that knowledge of needs status biased our assessment of personality.
Finally, we did not assess the level of services actually provided to our participants and so were unable to determine whether the unmet needs identified by our participants were known to service providers. Furthermore, it is unknown whether the presence of a personality disorder is associated with systematic differences in the perception of need. Other research has shown that staff and service users may give different accounts of need ( 34 , 35 ), and therefore future research in this area should aim to incorporate the perspectives of both staff and users.
Conclusions
In this study, personality disorder was associated with greater levels of unmet need among psychiatric inpatients, specifically in the domains of self-care, psychotic symptoms, psychological distress, risk to self, risk to others, alcohol use, sexual expression, and budgeting. Clinically, these findings highlight for the first time the importance of a comprehensive assessment of need among patients with personality disorders. Furthermore, the association between personality disorder and risk to self and others means that assessment of personality disorders provides important information for the management of risk. From a research perspective, our findings suggest that future epidemiologic studies of personality disorder should incorporate measures of need. The findings need to be replicated in other countries, and it also remains to be seen whether these findings in an inpatient population generalize to persons who receive care in community settings.
Acknowledgment
This study was supported by funding from the U.K. Department of Health.
1. Ochoa S, Haro JM, Autonell J, et al: Met and unmet needs of schizophrenia patients in a Spanish sample. Schizophrenia Bulletin 29:201-210, 2003Google Scholar
2. Young AS, Sullivan G, Bogart LM, et al: Needs for services reported by adults with severe mental illness and HIV. Psychiatric Services 56:99-101, 2005Google Scholar
3. Maslow AH: Motivation and Personality. New York, Harper and Row, 1954Google Scholar
4. Phelan M, Slade M, Thornicroft G, et al: The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. British Journal of Psychiatry 167:589-595, 1995Google Scholar
5. National Health Service Management Executive: Assessing Health Care Needs: A DHA Discussion Paper. London, Department of Health, 1991Google Scholar
6. Evans S, Greenhalgh J, Connelly J: Selecting a mental health needs assessment scale: guidance on the critical appraisal of standardized measures. Journal of Evaluation in Clinical Practice 6:379-393, 2000Google Scholar
7. McCrone P, Leese M, Thornicroft G, et al: A comparison of needs of patients with schizophrenia in five European countries: the EPSILON Study. Acta Psychiatrica Scandinavica 103:370-379, 2001Google Scholar
8. Ruggeri M, Leese M, Slade M, et al: Demographic, clinical, social, and service variables associated with higher needs for care in community psychiatric service patients: The South Verona Outcome Project 8. Social Psychiatry and Psychiatric Epidemiology 39:60-68, 2004Google Scholar
9. Hansson L, Sandlund M, Bengtsson-Tops A, et al: The relationship of needs and quality of life in persons with schizophrenia living in the community: a Nordic multi-center study. Nordic Journal of Psychiatry 57:5-11, 2003Google Scholar
10. Slade M, Leese M, Ruggeri M, et al: Does meeting needs improve quality of life? Psychotherapy and Psychosomatics 73:183-189, 2004Google Scholar
11. Murray V, Walker HW, Mitchell C, et al: Needs for care from a demand-led community psychiatric service: a study of patients with major mental illness. British Medical Journal 312:1582-1586, 1996Google Scholar
12. Slade M, Phelan M, Thornicroft G: A comparison of needs assessed by staff and by an epidemiologically representative sample of patients with psychosis. Psychological Medicine 28:543-550, 1998Google Scholar
13. Marshall M, Lockwood A, Green G, et al: Systematic assessments of need and care planning in severe mental illness: cluster randomised controlled trial. British Journal of Psychiatry 185:163-168, 2004Google Scholar
14. Bebbington PE: Population surveys of psychiatric disorder and the need for treatment. Social Psychiatry and Psychiatric Epidemiology 25:33-40, 1990Google Scholar
15. Grant BF, Hasin DS, Stinson FS, et al: Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry 65:948-958, 2004Google Scholar
16. Bender DS, Dolan RT, Skodol AE, et al: Treatment utilization by patients with personality disorders. American Journal of Psychiatry 158:295-302, 2001Google Scholar
17. Comtois KA, Russo J, Snowden M, et al: Factors associated with high use of public mental health services by persons with borderline personality disorder. Psychiatric Services 54:1149-1154, 2003Google Scholar
18. Murray MG, Anthenelli RM, Maxwell RA: Use of health services by men with and without antisocial personality disorder who are alcohol dependent. Psychiatric Services 51:380-382, 2000Google Scholar
19. Broadhead WE, Gehlbach SH, de Gruy FV, et al: The Duke-UNC Functional Social Support Questionnaire: measurement of social support in family medicine patients. Medical Care 26:709-723, 1988Google Scholar
20. Babor TF, de la Fuente JR, Saunders J, et al: AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva, World Health Organization, 1992Google Scholar
21. First MB, Gibbon M, Spitzer RL, et al: The Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, American Psychiatric Press, 1997Google Scholar
22. Tyrer P, Johnson T: Establishing the severity of personality disorder. American Journal of Psychiatry 153:1593-1597, 1996Google Scholar
23. McGuffin P, Farmer A, Harvey I: A polydiagnostic application of operational criteria in studies of psychotic illness: development and reliability of the OPCRIT system. Archives of General Psychiatry 48:764-770, 1991Google Scholar
24. Boardman AP, Hodgson RE, Lewis M, et al: North Staffordshire Community Beds Study: longitudinal evaluation of psychiatric inpatient units attached to community mental health centres: I. methods, outcome, and patient satisfaction. British Journal of Psychiatry 175:70-78, 1999Google Scholar
25. SPSS for Windows (version 10.0.5.). Chicago, SPSS, 1999Google Scholar
26. Feske U, Mulsant BH, Pilkonis PA, et al: Clinical outcome of ECT in patients with major depression and comorbid borderline personality disorder. American Journal of Psychiatry 161:2073-2080, 2004Google Scholar
27. Kay JH, Altshuler LL, Ventura J, et al: Impact of axis II comorbidity on the course of bipolar illness in men: a retrospective chart review. Bipolar Disorders 4:237-242, 2002Google Scholar
28. Berger P, Sachs G, Amering M, et al: Personality disorder and social anxiety predict delayed response in drug and behavioral treatment of panic disorder. Journal of Affective Disorders 80:75-78, 2004Google Scholar
29. Monahan J, Steadman HJ, Silver E: Rethinking Risk Assessment: The Macarthur Study of Mental Disorder and Violence. Oxford, United Kingdom, Oxford University Press, 2001Google Scholar
30. Moran P, Walsh E, Tyrer P, et al: Impact of comorbid personality disorder on violence in psychosis: report from the UK700 trial. British Journal of Psychiatry 182:129-134, 2003Google Scholar
31. Moran P, Walsh E, Tyrer P, et al: Does co-morbid personality disorder increase the risk of suicidal behavior in psychosis? Acta Psychiatrica Scandinavica 107:441-448, 2003Google Scholar
32. Zimmerman M: Diagnosing personality disorders: a review of issues and research methods. Archives of General Psychiatry 51:225-245, 1994Google Scholar
33. Skodol AE, Pagano ME, Bender DS, et al: Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychological Medicine 35:443-451, 2005Google Scholar
34. Slade M, Phelan M, Thornicroft G, et al: The Camberwell Assessment of Need (CAN): comparison of assessments by staff and patients of the needs of the severely mentally ill. Social Psychiatry and Psychiatric Epidemiology 31:109-113, 1996Google Scholar
35. Lasalvia A, Ruggeri M, Mazzi MA, et al: The perception of needs for care in staff and patients in community-based mental health services: the South-Verona Outcome Project 3. Acta Psychiatrica Scandinavica 102:366-375, 2000Google Scholar



