Predictors of Missed First Appointments at Community Mental Health Centers After Psychiatric Hospitalization
With respect to the treatment of psychiatric disorders, nonadherence may be defined as failure to enter a treatment program, premature termination of treatment, or incomplete implementation of instructions, including filling prescriptions ( 1 ). Nonadherence to treatment has a major impact on the effectiveness of therapeutic interventions and presents many problems in clinical practice ( 1 , 2 ). In a managed behavioral health care setting, Nelson and colleagues ( 3 ) demonstrated that patients who did not attend an outpatient appointment after discharge were two times as likely as those who kept at least one outpatient appointment to be rehospitalized in the same year. Patients who adhere to treatment recommendations have a lower relapse rate, which demonstrates the need for special attention and interventions designed to enhance adherence ( 4 ). Patients who do not attend their appointments after hospital discharge are at risk of being rehospitalized or relapsing, sometimes with serious symptoms that may endanger themselves or others ( 5 , 6 ).
The factors potentially associated with nonadherence are numerous, but the results of research in this area are somewhat inconsistent ( 7 , 8 ). In one study, five significant predictors of missed first appointments were being younger, being Hispanic, having a poorer family support system, not taking psychotropic drugs, and having health insurance ( 5 ). A longer period from contact to appointment may be another factor associated with nonadherence ( 3 ). Nosé and coworkers ( 1 ) cited lack of insight, positive symptoms, younger age, male gender, history of substance abuse, unemployment, and low social functioning as factors associated with nonadherence.
In this study, we sought to determine the predictors of an important aspect of nonadherence—failure to keep the first outpatient appointment after psychiatric hospitalization. We were particularly interested in determining practical, readily available predictors from the patient's chart and the treatment team during hospitalization, without the use of rating scales that are not routinely used in clinical practice. In addition to analyzing predictors that were significant in bivariate tests, we determined which risk factors were independently predictive when the analysis controlled for the other factors.
Methods
Charts were examined for consecutively discharged patients hospitalized either on the inpatient unit or the crisis stabilization unit of a large, urban, public-sector hospital. This county hospital serves a predominantly low-income, urban population, a majority of which is African American. Both the longer-stay inpatient unit (average length of stay of approximately 14 days) and the crisis stabilization unit (average length of stay of about seven days) admit patients primarily for evaluation and treatment of first episodes of illness or acute exacerbations of severe and persistent mental illnesses. These units do not routinely admit patients with mental retardation or dementia. Patients for whom substance use or withdrawal is the primary clinical focus are usually referred to other facilities.
Participating community mental health clinics included the main outpatient clinic affiliated with the hospital, located two blocks away; an adjacent specialized community outreach clinic; an intensive day treatment program; three county-operated clinics in the south central, south, and west catchment areas of the county; and an intake and initial assessment clinic for these three outlying county clinics. Charts of patients discharged with follow-up appointments to clinics other than these designated clinics—for example, to private practices or to community mental health clinics located in other counties—were excluded. Charts of patients who were hospitalized more than once during the period of data collection were not included a second time. Although support services before the first appointment, such as reminder calls, may have an impact on adherence rates, these services are not provided in this setting. On their discharge papers, patients routinely are given the clinic name, address, and telephone number along with the time and date of the first appointment.
Basic demographic, socioeconomic, psychosocial, and clinical data were obtained both by abstracting from the medical charts and by consulting with the social worker, the psychiatry resident or psychology intern, and the attending psychiatrist caring for the patient during hospitalization. A variety of continuous and categorical variables were recorded in a systematic way by using a data collection form designed by the research team. The outcome variable was whether the patient attended the first scheduled community mental health appointment after hospital discharge. This information was obtained by calling the established contact person at each of the mental health clinics within a week after the scheduled appointment to determine whether the patient had attended. Predictor and outcome information was gathered for 234 patients between December 2003 and July 2004. The research was approved by Emory University's institutional review board and the Grady Health System's research oversight committee.
A concerted effort was made to minimize missing data. Upon completion of data collection, approximately one-third of the variables contained at least one missing value among the 234 patients. Among these 19 variables, 15 contained three or fewer missing values. Of the remaining four variables with more than three missing values, the variable for the Global Assessment of Functioning score upon admission contained four missing values, 22 values were missing for the variable for the years of education, 23 values were missing for the variable estimating duration (in months) of prior outpatient treatment with an established clinician contained, and 32 values were missing for the variable for the number of prior psychiatric hospitalizations. To prevent biases in the sample, these four variables were excluded from subsequent analyses. Although double data entry was not performed, the accuracy of data entry was checked for a random sample, with acceptable results.
Bivariate analyses were performed on the potential predictors in relation to the outcome variable of interest—adherence with the first scheduled community mental health appointment after psychiatric hospitalization. Continuous variables were analyzed by using t tests for independent samples. Dichotomous and categorical predictor variables were analyzed by using chi square tests of association. The bivariate analyses were conducted to exclude covariates and predictors from the logistic regression model that were not significantly associated with a missed appointment Logistic regression modeling was performed by using variables that were significantly associated (p≦.10) with a missed appointment in the bivariate tests. A backward stepwise selection method was used in which the removal testing is based on the probability of the likelihood-ratio statistic, which is based on the maximum partial likelihood estimates. In the final model, all remaining predictors were independently significant at p<.05. Adjusted odds ratios and 95 percent confidence intervals were computed to determine effect estimates for variables that were significantly, independently predictive (p<.05) of a missed appointment when the analysis controlled for the other covariates. SPSS 12.0 software was used for all statistical tests.
Results
Thirteen patients did not have an outcome that was recorded as "yes, did keep first follow-up appointment" or "no, did not keep first follow-up appointment." Analyses were conducted by using data only from patients with an "adherent" or "nonadherent" outcome (N=221). In this sample of 221 patients, 80 (36 percent) kept their first scheduled follow-up appointment, whereas 141 (64 percent) did not.
The mean±SD age of the entire sample was 38.4±12.3 years, and the mean number of years of education was 12.0±2.4 years; no difference was found between the two groups for either variable (data not shown). Sociodemographic characteristics of the sample are consistent with those of the population of patients served by the two inpatient units and by the hospital in general. Basic sociodemographic data for the two groups are shown in Table 1 . Just over half the patients (124 patients, or 56 percent) were female, and 185 (84 percent) were African American. A total of 209 (95 percent) were unemployed, and the difference between the percentage of adherent patients who were employed part- or full-time (9 percent) compared with the percentage of nonadherent patients who were employed (4 percent) approached significance (p=.10). For the majority of patients the largest source of payment was either Medicaid (86 patients, or 39 percent) or Medicare (27 patients, or 12 percent), and for 105 (48 percent) the category was uncompensated or self-pay. No significant differences were found between the two groups on these variables.
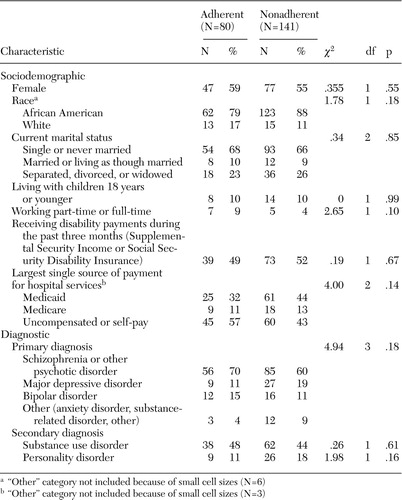 |
Overall, 141 patients (64 percent) had a primary diagnosis of schizophrenia or another psychotic disorder, 36 (16 percent) had a primary diagnosis of major depressive disorder, and 28 (13 percent) had a primary diagnosis of bipolar disorder. A total of 100 (45 percent) were documented to have a diagnosis of a substance use disorder, and 35 (16 percent) were documented to have a diagnosis of a personality disorder. The diagnostic distributions of the two groups are shown in Table 1 . The two groups did not differ with regard to any of these diagnostic categories.
Psychosocial characteristics of the two groups are shown in Table 2 . None of the psychosocial variables assessed were found to be significantly different between the two groups. The difference in the percentage of patients documented as having axis IV problems related to the primary support group (for example, death of a family member or health problems in the family) approached statistical significance (54 percent in the adherent group compared with 66 percent in the nonadherent group; p=.07).
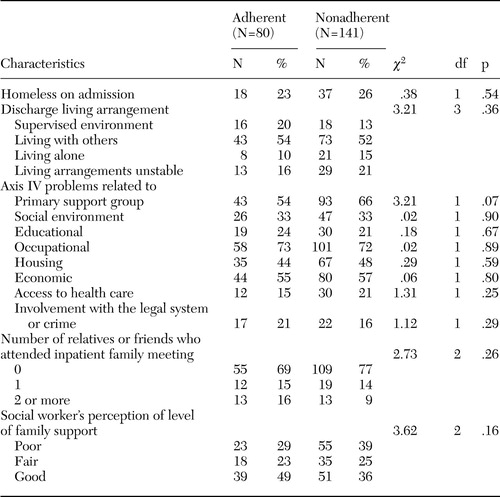 |
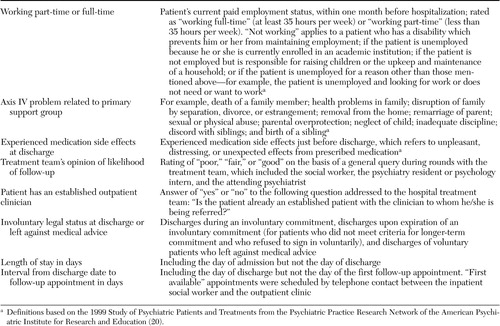
Table 3 shows the broad variety of clinical variables that were evaluated. The two groups differed on four of the 12 clinical variables. Compared with the adherent group, the nonadherent group had a lower percentage of patients rated as experiencing medication side effects at the time of discharge (25 percent compared with 15 percent; p=.06). Nonadherent patients were more likely to be rated "poor" by the treatment team at discharge with regard to likelihood of entering follow-up care (38 percent compared with 19 percent) and less likely to be rated "good" (25 percent compared with 48 percent; χ 2 =13.94, df=2, p<.01). Only 26 percent of nonadherent patients had an established outpatient clinician, compared with 44 percent of the adherent group (χ 2 =7.77, df=1, p<.01). Involuntary legal status at discharge was significantly different between the two groups (48 percent of the nonadherent group compared with 30 percent of the adherent group; χ 2 =6.48, df=1, p=.01). The group characterized as having an involuntary legal status at the time of discharge included six patients who had voluntary legal status but were discharged against medical advice.
 |
Length of stay in days and interval from discharge date to follow-up appointment in days were also predictors of a missed appointment (data not shown). Nonadherent patients had a shorter mean length of stay (10.5±6.5 days compared with 13.2±9.3 days in the adherent group; t=2.49, df=219, p=.01). Nonadherent patients had a longer mean interval from discharge date to follow-up appointment (16.0±13.9 days compared with 10.6±9.3 days in the adherent group; t=3.10, df=218, p<.01).
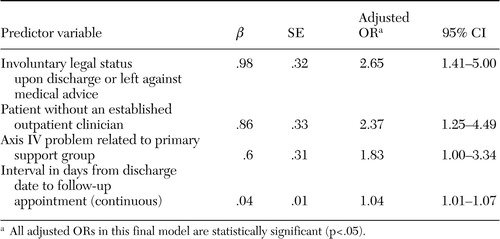
Eight variables that were associated with the outcome at the p≦.10 level were entered into a logistic regression model. Exact definitions and operationalizations of these eight variables are provided in Table 4 . As shown in Table 5 , four of eight predictors were independently associated with outcome when the analysis controlled for the other variables. Patients who had an involuntary legal status at hospital discharge or those who were discharged against medical advice had an odds of nonadherence nearly three times that of those with a voluntary legal status at discharge. Patients without an established outpatient clinician had an odds of nonadherence more than twice that of those with an established outpatient clinician. Patients with axis IV problems related to their primary support group had an odds of nonadherence nearly twice that of their counterparts. The interval from discharge date to follow-up appointment date (continuous variable) was also independently predictive of nonadherence, with each additional day increasing the odds of nonadherence by about 4 percent. For this model, the Cox-Snell R 2 statistic was .12.
 |
 |
The relationship between the outpatient clinic site and follow-up rates was examined. Of the 148 patients with a scheduled follow-up at a clinic affiliated with the hospital, 61 (41 percent) kept their first appointment, and of the 73 patients with a scheduled follow-up at a county clinic not affiliated with the hospital, 19 (26 percent) kept their first appointment (χ 2 =4.88, df=1, p=.03). When this variable was included in the logistic regression model, it did not remain in the final model, and the remaining four independently predictive variables therefore did not change.
Discussion
Several recent studies have focused increased attention on the issue of nonadherence with psychiatric outpatient visits ( 5 , 7 ), although research on missed clinical appointments is much less extensive than research on medication nonadherence. Adherence to treatment among psychiatric patients, at least in terms of medication adherence, is clearly associated with risk of rehospitalization and the overall economic costs of mental illnesses ( 9 , 10 , 11 , 12 ). It is likely that patients who do not attend their outpatient appointments after hospitalization will become nonadherent to prescribed medications. This study may be of particular value because it focused on patients with serious mental illnesses with a very high rate of nonadherence being treated in an urban community mental health setting with limited resources available for strategies that enhance adherence. Thus understanding the predictors of a missed first outpatient appointment is especially crucial. Furthermore, all predictors were readily available variables from the patient's hospital chart and treatment team.
We found that the rate of nonadherence (64 percent) in our community mental health setting was particularly high, higher than rates reported in other studies ( 5 , 13 ). However, the rate was consistent with the 50 percent or more that we had estimated a priori, based on clinical experience. Several factors may account for the especially high rate of nonadherence in our sample, including demographic characteristics (for example, 94 percent of our sample was unemployed), the diagnostic distribution (primarily severe and persistent mental illnesses), and the fact that our entire sample consisted of hospitalized patients. The high rate of nonadherence also may be suggestive of system-level barriers to adherence.
Clearly, the missed appointment rate of more than 60 percent in this population deserves further research. In terms of predictors of nonadherence, the results are consistent with prior findings on the relationship between nonadherence and a poorer family support system, a longer waiting period from contact to appointment, unemployment, and lack of insight (if involuntary legal status at discharge is taken as a proxy of insight). This study did not replicate prior results of an association between nonadherence and younger age, male gender, and insurance status. Differences in study populations may account for differences in risk factors identified as significant predictors of nonadherence, although it is not altogether clear why, for example, length of stay was associated with adherence in our study (at least in bivariate tests) and not in other studies.
Involuntary legal status at discharge or leaving against medical advice was the strongest of the four independent predictors of outpatient nonadherence. This variable may be a marker of poor treatment alliance and impaired insight, both of which are associated with treatment nonadherence ( 1 , 8 ). This finding supports the need for research into psychotherapeutic and psychoeducational strategies designed to strengthen the treatment alliance and enhance insight. An alternative explanation for the association of involuntary legal status at discharge or leaving against medical advice with nonadherence could be that people with a particularly strong aversion to the hospital (as indicated by their unwillingness to be hospitalized voluntarily or their checking out against medical advice) skip follow-up visits to avoid the possibility of rehospitalization. Prior research supports the idea that fear of hospitalization can lead to avoidance of outpatient treatment among some patients ( 14 , 15 ), although the specific connection to involuntary status at discharge requires further research. Interventions aimed at encouraging the treatment team to put the patient's goals at the center of their discharge planning and to have the patient's choices drive the discharge plan also may have a strong effect on therapeutic alliance and resulting adherence to discharge plans.
In terms of problems with the primary support group, the aim of interventions in this area would be to work with the primary support group both in and out of the hospital, as is done with family psychoeducation programs, or to strengthen support groups, such as by introducing the patient to consumer support groups. An example of the latter would be the Peer Bridger Project of the New York Association of Psychiatric Rehabilitation Services in which consumers come into the hospital to meet with patients and then continue to support them after discharge. This and similar programs aim to help individuals who are being discharged from psychiatric hospitalization by easing the transition into community life and by significantly decreasing their need for readmission ( 16 , 17 ).
In addition to these clinical issues, our findings also are important from a policy and programmatic perspective, especially because not having an established outpatient clinician and the interval from discharge date to follow-up appointment were independent predictors of nonadherence. Interventions to improve continuity of care between the outpatient and inpatient settings may have an impact on adherence to follow-up care ( 6 , 13 , 18 ). For example, if the patient has an outpatient clinician, this provider could be included in discharge planning meetings with the patient in the hospital. If the patient has no established clinician, introducing him or her to the scheduled outpatient clinician and providing a tour of the assigned outpatient facility before discharge may be beneficial. Because 54 of the patients in this sample did not have an outpatient treatment history, further analyses should be conducted to determine differences in predictors of nonadherence between those with and without an outpatient treatment history.
In this sample, the interval in days from discharge date to follow-up appointment was a predictor of nonadherence. Other studies also have found that longer intervals between visits are associated with higher missed appointment rates, even after multivariate adjustment ( 7 , 19 ). Aftercare programs that provide follow-up appointments as soon after discharge as possible may confer overall cost savings to local mental health systems by decreasing the risk of nonadherence and subsequent rehospitalization. Further research is needed to determine the effectiveness of this and other potential interventions for improving adherence in this population.
Several methodological limitations of this study should be recognized. First, diagnostic and other variables were based on the hospital chart and clinicians' reports, without the use of rating scales administered directly to patients. However, the purpose of this research was to study clinically meaningful predictors that do not require patient assessment beyond that done as part of routine evaluation and treatment. Second, generalizability may be limited because of the sociodemographic and diagnostic characteristics of our sample. Third, we cannot exclude the possibility that some patients received care at a clinic other than the assigned one or later than the original scheduled appointment. However, this possibility is unlikely, because community mental health services are structured around a catchment area model and rescheduling of appointments tends to be much rarer than missing appointments without rescheduling. Fourth, because of the nature of the study, some variables of importance to the issue of missed outpatient appointments could not be assessed. For example, therapeutic alliance was not measured formally.
Additionally, aside from patient characteristics, we did not examine institutional characteristics that might influence nonadherence, such as distance from the patient's home to the outpatient clinic. Other institutional characteristics that could affect adherence include the amount of client input regarding the clinic and clinician to which the client is assigned; atmosphere, reputation, neighborhood, attractiveness, or outreach activities of the clinic; and the availability of affordable and accessible transportation to the clinic.
Conclusions
Identifying relationships between institutional characteristics and adherence to follow-up care is an important area for future research. Clearly, there are many predictors of nonadherence other than those remaining in our final logistic regression model. Although data for these four variables are readily accessible in our system, they might not be available in other settings. Other inpatient psychiatric services should use information available to them that has been shown in previous research to predict adherence to assess and attempt to improve adherence among their patient populations.
Acknowledgment
This research was supported by grant 03004 from the Emory Medical Care Foundation.
1. Nosé M, Barbui C, Tansella M: How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychological Medicine 33:1149-1160, 2003Google Scholar
2. Boyer CA, McAlpine DD, Pottick KJ, et al: Identifying risk factors and key strategies in linkage to outpatient psychiatric care. American Journal of Psychiatry 157:1592-1598, 2000Google Scholar
3. Nelson EA, Maruish ME, Axler JL: Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatric Services 51:885-889, 2000Google Scholar
4. Novak-Grubic V, Tavcar R: Predictors of noncompliance in males with first-episode schizophrenia, schizophreniform, and schizoaffective disorder. European Psychiatry 17:148-154, 2002Google Scholar
5. Kruse GR, Rohland BM, Wu X: Factors associated with missed first appointments at a psychiatric clinic. Psychiatric Services 53:1173-1176, 2002Google Scholar
6. Olfson M, Mechanic D, Boyer CA, et al: Linking inpatients with schizophrenia to outpatient care. Psychiatric Services 49:911-917, 1998Google Scholar
7. Centorrino F, Hernan MA, Drago-Ferrante G, et al: Factors associated with noncompliance with psychiatric outpatient visits. Psychiatric Services 52:378-380, 2001Google Scholar
8. Fenton WS, Blyler CR, Heinssen RK: Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophrenia Bulletin 23:637-651, 1997Google Scholar
9. Thieda P, Beard S, Richter A, et al: An economic review of compliance with medication therapy in the treatment of schizophrenia. Psychiatric Services 54:508-516, 2003Google Scholar
10. Weiden PJ, Kozma C, Grogg A, et al: Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services 55:886-891, 2004Google Scholar
11. Olfson M, Mechanic D, Hansell S, et al: Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatric Services 51:216-222, 2000Google Scholar
12. Kelly GR, Scott JE: Medication compliance and health education among outpatients with chronic mental disorders. Medical Care 28:1181-1197, 1990Google Scholar
13. Axelrod S, Wetzler S: Factors associated with better compliance with psychiatric aftercare. Hospital and Community Psychiatry 40:397-401, 1989Google Scholar
14. Swartz MS, Swanson JW, Hannon MJ: Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behavioral Sciences and the Law 21:459-472, 2003Google Scholar
15. Campbell J, Schraiber R: The Well-Being Project: Mental Health Clients Speak for Themselves. Sacramento, California Network of Mental Health Clients, 1989Google Scholar
16. Kopelowicz A, Wallace CJ, Zarate R: Teaching psychiatric inpatients to re-enter the community: a brief method of improving the continuity of care. Psychiatric Services 49:1313-1316, 1998Google Scholar
17. UNM Psychiatric Center Peer Bridger Program, University of New Mexico. Available at http://hospitals.unm.edu/unmpc/peerbridgers/pbindex.shtml. Accessed Jun 09, 2005Google Scholar
18. Fink EB, Heckerman CL: Treatment adherence after brief hospitalization. Comprehensive Psychiatry 22:379-386, 1981Google Scholar
19. Kruse GR, Rohland BM: Factors associated with attendance at a first appointment after discharge from a psychiatric hospital. Psychiatric Services 53:473-476, 2002Google Scholar
20. Zarin DA, Pincus HA, West JC, et al: Practice-based research in psychiatry. American Journal of Psychiatry 154:1199-1208, 1997Google Scholar



