Effects of Caregivers' Perceived Stigma and Causal Beliefs on Patients' Adherence to Antidepressant Treatment
Abstract
OBJECTIVE: Nonadherence to prescribed medications is a significant problem in the treatment of mood disorders. Previously proposed adherence models have not been sufficiently accurate in identifying patients who do not adhere to treatment. This study evaluated the importance of the social context in adherence by using a prospective, longitudinal analysis. Specifically, this study evaluated the effects of caregivers' causal beliefs about depression and their perceptions of stigma on three-month treatment adherence among patients with depression. METHODS: Fifty patients with major depressive disorder and their primary caregivers were identified at a psychiatric hospital's outpatient clinic. Attributions for the causes of depression (either cognitive and attitudinal or medical and biological) and perceived stigma were assessed among caregivers at baseline, and patients' adherence was evaluated three-months after treatment began. RESULTS: Data were available for 47 patients at follow-up. Caregivers' attribution of depression to cognitive and attitudinal problems significantly predicted patients' decreased adherence. However, the degree of patients' adherence was not predicted by caregivers' attributions to medical and biological causes and caregivers' perceived stigma. CONCLUSIONS: The findings stress the importance of patients' social environment in determining treatment adherence and the necessity of educating caregivers about the impact that their causal attributions have on patients' behavior. Involving caregivers in treatment may improve their attitude toward patients with depression and, in doing so, enhance patients' adherence and outcome.
Lifetime prevalence of depression is estimated to be about 12 to 15 percent (1). Recurrent or chronic depression is common (2) and is often attributed to insufficient treatment (3). Although medications offer safe and effective treatment and have relatively benign side effects, many patients with depression do not get an adequate trial of treatment (4). In fact, up to 52 percent of patients who take antidepressants do not adhere to treatment, either by missing doses or by prematurely discontinuing pharmacologic therapy (5,6). In general, discontinuation rates are highest during the first month of treatment, with 35 percent of primary care patients dropping out and a steady decline thereafter (7).
The determinants of nonadherence among patients with depression have not been sufficiently examined (8). Most studies have used the Health Belief Model to predict the likelihood of adherence. This model suggests that patients initiate or continue medication treatment on the basis of their individual beliefs, attitudes, and expectations of their illness and its treatment. For example, Elkin and colleagues (9) examined how patients' attributions of the cause of their depression (cognitive, interpersonal, and medical) affected short-term adherence to different treatments (cognitive-behavioral therapy, interpersonal psychotherapy, and pharmacotherapy). Their data suggested that congruency between attributions and treatment type predicted adherence. However, it is important to note that 60 percent of their sample did not report a clear predilection for one attribution. Therefore, it appears that attributions are not singular in people's minds.
While affirming the utility of the Health Belief Model in a recent literature review, Cohen and colleagues (8) evaluated other factors that might contribute to adherence. Interestingly, marriage was the only demographic variable that was positively associated with adherence among patients with depression, suggesting that the social environment may play a role in adherence (10,11). Sirey and colleagues (12,13) further emphasized the importance of the social context in health-related actions. They tested how adherence is affected by perceived stigma—that is, the belief that most people will devalue and discriminate against persons with mental illness and those who use psychiatric treatment. They found that the degree of stigma that patients with depression perceived predicted both drug treatment nonadherence and treatment discontinuation.
A newer model that highlights the role of social support systems in treatment decisions is the network episode model (14,15). This model conceptualizes mental health service use as a social process that is negotiated through contacts with the community, the treatment system, and social service agencies. Thus decisions about scheduling an appointment or filling a prescription are greatly affected by contacts with others, who may or may not be supportive of the need for these services. The importance of the social environment within the context of care was also recently acknowledged in a number of reports that encouraged researchers to examine how health is influenced by social contexts—such as families, neighborhoods, schools, work sites, and political jurisdictions (16).
Empirical support already exists for the potential negative effects of family caregivers on the outcome of illness among patients with depression (17,18). Moreover, a recent study showed that among patients with bipolar disorder, caregivers' burden and emotional overinvolvement at baseline affected medication adherence seven months into treatment and outcome 15 months into treatment (19). However, studies have not yet explored the relationship between caregivers' attitudinal characteristics and medication adherence among patients with unipolar depression.
On the basis of the above research, a potentially influential characteristic may be caregivers' beliefs about the origins of the depression. It has been shown that caregivers vary in their beliefs about the causes of depression, attributing it to psychosocial, genetic, or cognitive problems (20). In concordance with research on how patients' attributions of the causes of their illness can affect their treatment (9), caregivers' attributions may have a similar effect on patients' treatment behavior. Another caregiver characteristic that may play a role in patients' treatment course is caregivers' fear of stigma. Horwitz (21) found that family members were less likely than friends to encourage their relative with mental illness to seek psychiatric services. The study suggested that family members' fear of stigma might induce kin to normalize or deny the relatives' psychiatric problems. Although this interesting interpretation was not directly examined in Horwitz's study, a recent study (22) demonstrated that caregivers of patients with psychiatric diagnoses are indeed highly concerned about stigma directed toward patients and their families.
Our study was a prospective, longitudinal analysis of the effects of caregivers' attributions of the cause of the illness and caregivers' perceived stigma on patients' three-month treatment adherence. Specifically, we hypothesized that if caregivers showed high levels of cognitive and attitudinal attributions (for example, the belief that pessimistic attitudes about many things are a cause of the patient's problems) and high levels of perceived stigma before treatment was initiated, medication adherence would be decreased, whereas high levels of medical and biological attributions (for example, the belief that an imbalance of certain substances in the brain is a cause of the patient's problems) would predict increased adherence.
Methods
Sample
The participants were interviewed as part of a larger longitudinal observational study on the treatment and course of depression, which was carried out from October 1995 to December 1997 (23). The study was approved by the institutional review board of the Weill Medical College of Cornell University. Newly admitted patients of an outpatient mental health clinic of a psychiatric hospital in Westchester County were approached, and a written informed consent was obtained from patients who participated in the study. Consenting patients were asked to identify a caregiver.
The primary caregiver was the one who satisfied the greatest number (and at least three) of the following five criteria (24): is a spouse, parent, or spouse equivalent; has the most frequent contact with the patient; helps to financially support the patient; has most frequently been a collateral in the patient's treatment; and is the emergency contact. In case of a tie, the patient was asked to select the person who has been most closely involved with his or her care. The selected caregiver was contacted, and informed consent was obtained.
Data collection
Patients were selected with a two-stage sampling procedure that was described in detail by Sirey and colleagues (12). Patients and caregivers were assessed at the initiation of outpatient mental health care. Patients who received prescriptions for antidepressant medications (N=50) and their caregivers accounted for this study's sample. Follow-up interviews with the patients were conducted three months after treatment was initiated to assess medication side effects and to evaluate adherence. All data were collected by a trained research assistant who was supervised by research psychologists who were participating in the initial data collection for the parent study (23).
Measures
Caregivers' measures. The caregivers' perceived stigma was assessed with a 15-item instrument (Link's scale of perceived stigma), which comprised two scales: perceived stigma of patients and perceived stigma of families (25). The scales evaluate beliefs about the degree of devaluation and discrimination directed toward persons with mental illness and their families. Each statement was rated by using a 4-point scale; possible scores range from 1, strongly agree, to 4, strongly disagree.
Struening and colleagues (22) reported satisfactory internal consistency reliability for both scales (Cronbach's alpha of .82 for the perceived stigma of patients, and Cronbach's alpha of .71 to .77 for the perceived stigma of families) when administered to caregivers of patients with serious mental disorders. Similar Cronbach's alpha rates were obtained in our sample: Cronbach's alpha of .77 and Cronbach's alpha of .73, respectively.
The caregivers' causal attributions were measured by using a 20-item self-report instrument (significant others' attitudes and beliefs about depression [Family Attitudes and Beliefs]) (20). Two subscales were used in this study: medical and biological attributions (five items) and cognitive and attitudinal attributions (seven items). Each item was rated on a 5-point Likert scale; possible scores range from 1, strongly disagree, to 5, very strongly agree.
Previous research has demonstrated that most persons do not have a clear predilection for a single attribution (9). To examine the strength of endorsement of each attribution scale separately, each subscale was analyzed as a continuous variable. The internal consistency reliability of these subscales was not evaluated in previous research. In this sample we found a Cronbach's alpha of .62 for the medical and biological attribution scale and a Cronbach's alpha of .75 for the cognitive and attitudinal attribution scale. To increase the reliability of the medical and biological attribution scale, we excluded one of the items from the scale—that is, "an illness, which affects him/her emotionally instead of physically, is a cause of his/her problems." This change resulted in an acceptable alpha of .72.
Patients' baseline measures. The diagnosis of major depressive disorder at baseline was established by using the Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P) (26). Depression severity was assessed with the structured interview guide for the 17-item Hamilton Depression Rating Scale (27,28). The patients' overall level of functioning was assessed with the Global Assessment of Functioning scale (29).
Patients' three-month measures. Information about whether the patient was given a prescription for antidepressants, as well as the dosage and duration of treatment, was collected by using the patient's self-report and chart review. When these sources were not consistent, only the chart review data were used (23).
The patients' three-month medication adherence was assessed with a brief interview that was conducted by a trained research assistant to determine the frequency and pattern of missed doses. Adherence was then rated on a Likert scale; possible scores range from 6, full adherence, to 1, total nonadherence, reflecting cessation of medication use. Although self-reports are subject to influences of deception and poor recall, previous research has shown a high correlation between pill count and self-reports (30). In previous research, Sirey and colleagues (13) demonstrated the concordance between patient's self-report ratings and blood tests recorded in the patient's chart. These researchers also reported that their adherence distribution was skewed, as most patients tend to report good compliance. Given this fact, the adherence variable that we used in our study was dichotomized; patients who scored 6 on the adherence scale were classified as adherent, and all others were classified as nonadherent.
The presence of medication side effects and their severity were assessed; possible severity scores range from 1, not at all bothersome, to 3, extremely bothersome.
Data analysis procedures
Bivariate analyses were conducted for all demographic variables, patients' clinical characteristics, and the main outcome variable (medication adherence). These preliminary analyses were used to assess any clinical and demographic variables that were significantly associated with the dependent variable. A linear regression analysis was performed to examine the hypothesis, controlling for any significant demographic and clinical variables. Only variables that had significant univariate or bivariate associations (p<.05, two-tailed test) with the dependent variable were included in the final regression analysis.
Results
Sample
Fifty patients who were given a prescription for antidepressants and their caregivers were surveyed at the initiation of treatment. At the three-month follow-up, 47 of the patients were reinterviewed. All patients met criteria for major depressive disorder, as measured by the SCID-P. Table 1 summarizes the demographic and clinical characteristics of the patients and caregivers at baseline.
Variables associated with adherence
The kinship between the caregiver and the patient was the only significant demographic variable that predicted patients' adherence. Patients whose caregivers were their spouses were more likely than those whose caregivers were other family members or friends to adhere to their medications (χ2=4.08, df=1, p<.05). No other significant relationships were found between medication adherence and caregivers' and patients' demographic characteristics—that is, age, gender, living arrangement, education, income, and work status. In addition, no relationship was found between adherence and patients' clinical characteristics—that is, severity of illness, overall functioning, previous hospitalizations, previous depressive episodes, medication type, treatment side effects, and severity of side effects.
A logistic regression analysis was conducted to test the relationship between caregivers' causal attributions, caregivers' perceived stigma, and patients' medication adherence. The kinship variable of the significant caregiver (spouse compared with other family member) was entered into the model first, followed by all caregivers' variables of interest (that is, perceived stigma of patients, perceived stigma of families, medical and biological attribution, and cognitive and attitudinal attribution); adherence was the dependent variable. This analysis resulted in an overall significant model, (χ2=11.34, df=5, p<.05). The model's Nagelkerke R2 predicted 32.8 percent of the variance in the adherence scores (31). As shown in Table 2, of the variables entered into the model, caregivers' belief that the patients' illness stemmed from cognitive and attitudinal problems was the only variable that significantly predicted poor adherence to the recommended medication treatment, after the analysis controlled for caregivers' kinship. In fact, among the patients whose caregivers' scores on the cognitive and attitude attribution scale were at the top third of the sample, 40 percent (6 of 15 patients) reported nonadherence; among patients whose caregivers' scores were at the lower third of the sample, 10 percent (2 of 20 patients) reported nonadherence.
Discussion
When depression strikes a family member or a friend, caregivers naturally search for its causes and must confront its stigmatizing attributes. This study revealed that patients whose caregivers felt that depression stemmed from cognitive and attitudinal problems at the start of pharmacotherapy treatment were less likely to adhere to their medications three months into treatment, after the analysis controlled for kinship between the patient and the caregiver. However, caregivers' perceived stigma and medical and biological attributions did not predict treatment adherence. It is possible that a relationship between perceived sigma and treatment adherence might be better discerned by a more specific assessment of caregivers' beliefs—that is, assessing their level of stigmatization of patients with depression and their families, rather than of patients with mental illness and their families.
The fact that cognitive and attitudinal attributions, but not medical and biological attributions, predicted patients' adherence may reflect cognitive biases of patients with depression—that is, the tendency to disqualify positive information, yet pay close attention to, dwell on, and remember negative information (32,33). Thus caregivers' negative messages likely affected the patients' behavior more than positive ones. For instance, although caregivers who believed that depression stemmed from medical and biological factors may have encouraged medication treatment, the patients may have failed to pay attention to these encouraging comments or dismissed them altogether.
By contrast, it was expected that caregivers who strongly attributed depression to cognitive and attitudinal factors would criticize and blame the patients. Such behavior by caregivers will suggest to patients that medications are useless. Because of negative thinking bias, depressed patients may have been more likely to attend to and be influenced by such remarks and behavior, resulting in markedly reduced adherence.
Caregivers' beliefs may be alterable through intervention. Evidence shows that opinions about the causes of mental illness can be changed with exposure to alternative information or experience (34). Future work could develop caregiver interventions that specifically target the complexity of depression, its multiple etiologies, and possible treatments. In fact, a recent review of diverse interventions for bipolar disorder concluded that adherence is maximized when the patient's family members or the significant other is involved in the treatment (35). Moreover, it may be especially important to address the cognitive aspects of depression and correct caregivers' misperceptions that depressed patients can easily control their faulty cognitions and negative attitudes.
Of additional note is our finding that patients with caregivers who were spouses, as opposed to other family members, were more adherent to medication treatment, independent of living arrangements. This finding is consistent with those from previous studies that stated that marital status is associated with improved treatment adherence among patients with depression (10,11). This finding further underscores the importance of the social environment in patients' medication use.
Several limitations of this study should be noted. First, the sample was relatively small and homogeneous, which limits the generalizability of the findings. Given that only one of the four main analyses of variables that predict adherence yielded significant results, the possibility of type I error cannot be discarded. Moreover, because participants in this study were selected from a hospital-affiliated clinic, it is likely that they were more severely depressed than patients in other clinic settings. The influence of the caregiver on treatment adherence may vary depending on the severity of depression and the degree of functional impairment.
Conclusions
This study examined caregivers' attributions and perceptions of stigma separately. However, previous theory and research have shown that the types of attributions that people make about mental illness—that is, how controllable and stable they perceive mental illness to be—are strongly related to the stigma they elicit (36,37,38). Therefore, future research should examine how these two interact to affect caregivers' response to patients. Finally, building on previous findings, this study suggests that caregivers' and patients' beliefs may play important roles in the patients' treatment behavior. Further studies are needed to simultaneously examine the causal attributions of patients and their caregivers and determine how these attributes affect the adherence and outcome of patients with depression.
Dr. Sher and Dr. McGinn are affiliated with the Ferkauf Graduate School of Psychology of Yeshiva University in the Bronx, New York. Dr. Sirey and Dr. Meyers are with the department of psychiatry at New York Presbyterian Hospital, Westchester Division, in White Plains and with the department of psychiatry at Weill Medical College of Cornell University in White Plains. Send correspondence to Dr. Sher at Metropolitan Center for Mental Health, 1090 St. Nicholas Avenue, New York, New York 10032 (e-mail, [email protected]).
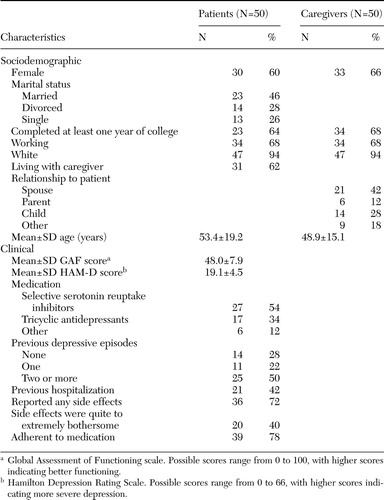 |
Table 1. Baseline characteristics of patients who were taking antidepressants and their caregivers
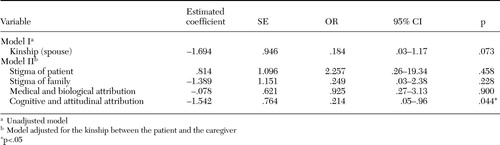 |
Table 2. Summary of hierarchical regression analysis for variables that were assessed among caregivers at baseline to predict patients' adherence to antidepressant treatment at the three-month follow-up (N=47)
1. Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision. Washington, DC, American Psychiatric Association, 2000Google Scholar
2. Thase ME, Sullivan LR: Relapse and recurrence of depression: a practical approach for prevention. CNS Drugs 4:261–277, 1995Crossref, Google Scholar
3. Keller MB, Lavori PW, Mueller TI, et al: Time to recovery, chronicity, and levels of psychopathology in major depression: a five-year prospective follow-up of 431 subjects. Archives of General Psychiatry 49:806–816, 1992Google Scholar
4. Delgado PL: Approaches to the enhancement of patient adherence to antidepressant medication treatment. Journal of Clinical Psychiatry 61(suppl 2):6–9, 2000Medline, Google Scholar
5. Lin EH, Von Korf M, Katon W, et al: The role of the primary care physician in patients' adherence to antidepressant therapy. Medical Care 33:1–10, 1995Crossref, Medline, Google Scholar
6. Maddox JC, Levi M, Thompson C: The compliance with antidepressants in general practice. Journal of Psychopharmacology 8:48–53, 1994Crossref, Medline, Google Scholar
7. Simon GE, Von Korff M, Wagner EH, et al: Patterns of antidepressant use in community practice. General Hospital Psychiatry 15:399–408, 1993Crossref, Medline, Google Scholar
8. Cohen NL, Parikh SV, Kennedy SH: Medication compliance in mood disorders: relevance of the health belief model and other determinants. Primary Care Psychiatry 6:101–110, 2000Crossref, Google Scholar
9. Elkin I, Yamaguchi JL, Arnkoff DB, et al: "Patient-treatment fit" and early engagement in therapy. Psychotherapy Research 9:437–451, 1999Google Scholar
10. Lader M: The problems of safety and compliance with conventional antidepressant drugs. Acta Psychiatrica Scandinavica 308:91–95, 1983Google Scholar
11. Fawcett J: Compliance: definition and key issues. Journal of Clinical Psychiatry 56(suppl 1):4–8, 1995Medline, Google Scholar
12. Sirey JA, Bruce ML, Alexopoulos GS, et al: Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. American Journal of Psychiatry 158:479–481, 2001Link, Google Scholar
13. Sirey JA, Bruce, ML, Alexopoulos GS, et al: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services 52:1615–1620, 2001Link, Google Scholar
14. Pescosolido BA, Boyer CA: How do people come to use mental health services? Current knowledge and changing perspectives, in A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. Edited by Scheid TL, Horwitz AV. New York, Cambridge University Press, 1999Google Scholar
15. Pescosolido BA, Boyer CA, Lubell KM: The social dynamics of responding to mental health problems: past, present, and future challenges to understanding individuals' use of services, in Handbook of Sociology and Social Research. Edited by Phelan JC, Aneshensel CS. Dordrecht, Netherlands, Kluwer Academic Publishers, 1999Google Scholar
16. Kirchstein R: Toward higher levels of analysis: Progress and promise in research on social and cultural dimensions of health. Presented at the conference entitled Higher Levels of Analysis: Progress and Promise in Research on Social and Cultural Dimensions of Health, Bethesda, Md, June 27–28, 2000Google Scholar
17. Vaughn C, Leff J: The influence of family and social factors on the course of psychiatric illness: a comparison of schizophrenic and depressed neurotic patients. British Journal of Psychiatry 129:125–137, 1976Crossref, Medline, Google Scholar
18. Hooley JM, Orley J, Teesdale JT: Levels of expressed emotion and relapse in depressed patients. British Journal of Psychiatry 148:642–647, 1986Crossref, Medline, Google Scholar
19. Perlick DA, Rosenheck RA, Clarkin JF, et al: Impact of family burden and affective response on clinical outcome among patients with bipolar disorder. Psychiatric Services 55:1029–1035, 2004Link, Google Scholar
20. Jacob M, Frank E, Kupfer DJ, et al: Recurrent depression: an assessment of family burden and family attitudes. Journal of Clinical Psychiatry 48:395–400, 1987Medline, Google Scholar
21. Horwitz A: Family kin and friend networks in psychiatric help-seeking. Social Science and Medicine 12:297–304, 1978Medline, Google Scholar
22. Struening EL, Perlick DA, Link BG, et al: The extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services 52:1633–1638, 2001Link, Google Scholar
23. Sirey JA, Meyers BS, Bruce ML, et al: Predictors of antidepressant prescription and early use among depressed outpatients. American Journal of Psychiatry 156:690–696, 1999Abstract, Google Scholar
24. Pollak CP, Perlick D: Sleep problems and institutionalization of the elderly. Journal of Geriatric Psychiatry Neurology 4:204–210, 1991Crossref, Medline, Google Scholar
25. Link BG, Cullen FT, Struening EL, et al: A modified labeling theory approach to mental disorders: an empirical assessment. American Sociological Review 54:400–423, 1989Crossref, Google Scholar
26. First MB, Spitzer RL, Williams JB, et al: Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P). Washington, DC, American Psychiatric Press, 1995Google Scholar
27. Hamilton M: A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry 23:56–62, 1960Crossref, Medline, Google Scholar
28. Williams JB: A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry 45:742–747, 1988Crossref, Medline, Google Scholar
29. Endicott J, Spitzer RL, Fleiss JL: The global assessment scale: a procedure of measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 45:742–747, 1976Google Scholar
30. Myers ED, Branthwaite A: Outpatient compliance with antidepressant medication. British Journal of Psychiatry 160:83–86, 1992Crossref, Medline, Google Scholar
31. Nagelkerke NJD: A note on a general definition of the coefficient of determination. Biometrika 78:691–692, 1991Crossref, Google Scholar
32. Beck AT, Rush AJ, Shaw BF, et al: Cognitive Therapy of Depression. New York, Guilford, 1979Google Scholar
33. Burns DD: Feeling Good: The New Mood Therapy. New York, Morrow, 1980Google Scholar
34. Farina A: Stigma: Handbook of Social Functioning in Schizophrenia. Edited by Mueser KT, Tarrier N. Boston, Allyn and Bacon, 1998Google Scholar
35. Sajatovic M, Davies M, Hrouda DR: Enhancement of treatment adherence among patients with bipolar disorder. Psychiatric Services 55:264–269, 2004Link, Google Scholar
36. Weiner B: An attributional theory of achievement motivation and emotion. Psychological Review 92:548–573, 1985Crossref, Medline, Google Scholar
37. Weiner B: Searching for order in social motivation. Psychological Inquiry 7:199–216, 1996Crossref, Google Scholar
38. Corrigan PW: Mental health stigma as social attribution: implications for research methods and attitude change. Clinical Psychology: Science and Practice 7:48–67, 2000Crossref, Google Scholar



