Effect of Medicaid Eligibility Category on Racial Disparities in the Use of Psychotropic Medications Among Youths
Abstract
OBJECTIVE: This study sought to determine the degree to which Medicaid eligibility categories modify disparities between black and white youths in the prevalence of psychotropic medication. METHODS: Computerized claims for 189,486 youths aged two to 19 years who were continuously enrolled in a mid-Atlantic state Medicaid program for the year 2000 were analyzed to determine population-based annual prevalence of psychotropic medication by race or ethnicity and by whether the youths were eligible for Medicaid for reasons of family income, disability, or foster care placement. Logistic regression was used to assess the interaction of eligibility category and race. RESULTS: The mean annual prevalence of psychotropic medication for the population was 9.9 percent. The prevalence was 2.17 times higher for white youths than for black youths (16.5 percent compared with 7.6 percent). However, within eligibility categories, the white-to-black disparity was 3.8 among youths who were eligible for Medicaid because their family income was below the federal poverty level and 3.2 for youths enrolled in the State Children's Health Insurance Program. CONCLUSIONS: Medicaid eligibility categories had a profound impact on the racial disparity associated with the prevalence of psychotropic medications for youths. Eligibility category should be taken into account when ascertaining the role of access, undertreatment, and culture in disparities in mental health treatment.
Racial disparities in health care—and mental health care in particular—have been a focus of considerable interest among clinical and health service researchers. The Surgeon General's report (1) was a call to action on this subject. As a result, numerous agencies and centers are engaged in seeking a better understanding of the reasons these disparities occur.
Medicaid data are a major source of information about racial disparities in treatment patterns; previous Medicaid studies suggested that minority racial status was associated with a lower rate of treatment with psychotropic medications (2,3,4). Both income level and race or ethnicity have been found to have an independent impact on the prevalence of medication treatment (5,6). The generally lower use of mental health services among adults from racial or ethnic minority groups who have severe mental disorders has been related to mistrust and racially biased diagnoses (7). Racially biased diagnosis of adults with schizophrenia has been well documented (8). It follows that there would also be disparities in the choice of prescribed psychotropic medications and dosage (9). Among children, negative attitudes toward medication (10) and cultural differences (11) have been implicated in lower use of stimulants. Across the age groups, barriers to service use include limited availability of professionals from minority groups and geographic barriers (12).
Medicaid data are particularly important for studying children, because Medicaid provides medical insurance to more than 25 percent of youths in the United States (13). As a group, youths who are enrolled in Medicaid have more chronic health problems (14,15), more identified mental health problems (16,17,18), and similar or higher use of psychotropic medication than youths covered by managed care HMO insurance (19,20,21,22). Others have reported intermediate rates between youths who are covered by managed care programs and those who have commercial insurance (23).
However, Medicaid is made up of numerous eligibility categories with widely varying demographic and service use patterns. For example, children in foster care accounted for 50 percent of all Medicaid psychiatric visits in California, even though this group represented less than 4.8 percent of California's (developmental or other) enrollees (24). A similar service pattern was noted in Colorado, Washington State, and Pennsylvania (25). To organize and better understand these variations, Medicaid eligibility categories for youths can be grouped according to income or special needs. Income at or below the poverty level qualifies families for Temporary Assistance to Needy Families (TANF), and income up to 200 percent above the poverty level qualifies families for the State Children's Health Insurance Program (S-CHIP) (in states where the S-CHIP is administered by Medicaid). Special-needs categories include out-of-home placement (foster care) and documented disability (developmental or other chronic physically or mentally disabling condition) that entitles recipients to Supplemental Security Income (SSI).
Most analyses of the prevalence of psychotropic medication among Medicaid-enrolled youths have exclusively used aggregated eligibility categories (3,26,27,28,29,30). However, several investigators have compared service use and treatment findings for Medicaid-enrolled youths from low-income families with youths who have disability coverage (4) or who are in foster care (24,31).
Only two mental health service studies compared Medicaid-enrolled youths across three eligibility categories (low income, SSI, and foster care). Harman and colleagues (32) reported on psychotropic drug expenditures from seven counties in southwestern Pennsylvania in 1995. DosReis and associates (33) analyzed 1996 data from one county in a mid-Atlantic state to report use of mental health services and medications. Both studies indicated sizable treatment differences across the three eligibility categories.
In the study reported here we expanded on the Medicaid study by dosReis and associates (33) by increasing the sample size from the county level (fewer than 16,000 persons) to the state level (more than 218,000), assessing more recent data (from the year 2000), and adding a fourth eligibility category, the S-CHIP, which in this state has already grown bigger than the TANF eligibility category. The prevalence of psychotropic medications among youths was assessed in relation to demographic characteristics, with a particular focus on the potential modifying effect of Medicaid eligibility categories on the racial disparity in prevalence of psychotropic medication.
We expected that the severity of health conditions would vary between the TANF recipients and the other eligibility groups (26), which could influence medication use. With additional data now available for S-CHIP-insured youths, the relationship of race or ethnicity and eligibility categories can be more precisely explored. Most important is the advance of methodology for studies of racial disparities from Medicaid data sources, given that commercial insurance data generally do not identify race or ethnicity; federal treatment surveys, such as the National Ambulatory Care Survey, are restricted to treated populations; and patient-reported survey data, such as the Medical Expenditure Panel Survey, tend to be of insufficient size or limited reliability to ensure accurate assessment of racial disparities in use of services, particularly prescription drugs.
Methods
This study was a cross-sectional analysis of pharmacy claims and encounter data for children enrolled in a state Medicaid program (fee-for-service and managed care plans) in the year 2000. The study protocol was approved by the institutional review boards of the University of Maryland, Baltimore, and the Maryland Department of Health and Mental Hygiene.
The study population comprised 261,638 Medicaid-enrolled youths who were aged two through 19 years as of January 1, 2000. Four major eligibility categories were identified: TANF, the S-CHIP, foster care, and SSI. The rationale for distinguishing these eligibility categories was that the first two categories (TANF and the S-CHIP) represent the poor or uninsured, whereas foster care and SSI generally represent youths who have complex social or medical or mental health problems. These categories were determined on the basis of the coverage type and coverage group variables in the Medicaid eligibility-spans file. Enrollees who had been enrolled for only one month were excluded to enable us to more accurately assess the prevalence of medication, and enrollees who had more than one eligibility type during the year (16.7 percent) were excluded to produce mutually exclusive eligibility categories for a total of 217,900 youths.
Four dependent variables were created to measure the annual prevalence of psychotropic medication per 100 enrollees. We defined prevalence as the presence of one or more prescription claims for any psychotropic drug and, specifically, for three major drug classes during the study year (2000). For each recipient, we created dichotomous variables to calculate the prevalence of psychotropic medication for the following four modified American Hospital Formulary Service (AHFS) drug classifications: any psychotropic medication (stimulants, antidepressants, neuroleptics, lithium, mood stabilizer anticonvulsants [carbamazepine, valproic acid, and gabapentin], antiparkinsonians, hypnotics, anxiolytics or alpha-agonists); stimulants; antidepressants; and neuroleptics. Neuroleptics were restricted to the AHFS category that excludes neuroleptic products for coughs and colds and for nausea.
Information about the main independent variables (eligibility category and race) and demographic covariates (age and gender) was obtained from the demographic and eligibility-spans file. Self-reported race or ethnicity was categorized as white, black, or other (Hispanic, Asian, Native American, or Pacific Islander). The duration of enrollment (in months) was determined from the eligibility-spans file. We classified recipients as continuously enrolled for the year if they had been enrolled in Medicaid for at least ten months.
Analyses were conducted by using SAS Unix version 7.0. Bivariate analysis of the prevalence of psychotropic medication according to race or ethnicity, eligibility category, age, gender, and enrollment time was first completed to screen for effect modification and potential confounders. Logistic regression was used to estimate the association between psychotropic drug use and race or ethnicity, adjusting for age and gender among the continuously enrolled (N=189,486). Because we had hypothesized that the association between drug use and race or ethnicity varied by eligibility category, we tested for significance of the interaction of race and eligibility category in the models by using the likelihood ratio test.
Age and gender were included as covariates in the final models. Models were developed for each of the four classes of psychotropic drugs (stimulants, antidepressants, neuroleptics, and any psychotropic drug). Odds ratios and 95 percent confidence intervals are reported.
Results
As Table 1 shows, 217,900 Medicaid-enrolled youths aged two to 19 years had more than one month of enrollment during 2000 and were categorized into one of four mutually exclusive eligibility categories. These youths represented approximately 87 percent of the total population of Medicaid-enrolled two- to 19-year-olds. Across eligibility categories, the numbers of males and females were comparable except in the SSI category, which was 64 percent male. SSI showed a nearly linear increase with age, the S-CHIP showed a reverse trend by age, and the TANF and S-CHIP categories had comparatively fewer older adolescents (ages 15 to 19). The S-CHIP category had proportionally more two- to four-year-olds (35 percent) and fewer black youths (46 percent) than the other groups. White youths were in the minority in all categories. The "other" race or ethnicity group comprised enrollees identified as Hispanic (6.3 percent), Asian (1.9 percent), Native American (.2 percent), Pacific Islander (.02 percent), and unknown (2.7 percent).
In relation to duration of enrollment, the TANF group and the S-CHIP group had the lowest percentage of enrollment for a continuous period defined as ten to 12 months (83 percent to 88 percent). Exclusion of the small proportion of noncontinuous enrollees (13 percent) resulted in the restriction of further analyses to a continuously enrolled study population of 189,486. This approach ensured equal probability of prescription drug use across the four eligibility groups without requiring a time-consuming proportional analysis to adjust for the modest number of noncontinuous enrollees.
Table 2 shows prominent disparities in race-specific prevalence of any psychotropic medication and for the three drug classes. There was a white-black disparity of 2.17-fold (16.5 percent compared with 7.6 percent) and a white-"other" disparity of 3.75-fold (16.5 percent compared with 4.4 percent). Antidepressants had the greatest white-black disparity (2.6-fold), and neuroleptics had the least (twofold). Although the racial disparities were large, differences in age, gender, and eligibility category could have influenced these results. The composition was varied and small for the "other" race or ethnicity group: Hispanic (N=396), Asian (N=110), Native American (N=37), and Pacific Islander or Alaskan (N=1).
Table 3 shows the unadjusted medication prevalence for any psychotropic drug and for the three drug classes in relation to Medicaid eligibility groups. Most striking is the difference between the groups on the basis of TANF and S-CHIP eligibility compared with the SSI and foster care eligibility categories. Among SSI and foster care enrollees, psychotropic medications were dispensed for 34.7 percent and 25.8 percent of youths, respectively, whereas for the vast majority of the Medicaid population (86.4 percent), the psychotropic medication rate was only 7.4 percent (TANF) and 6 percent (S-CHIP). Comparing eligibility categories with respect to the three drug classes, 67 percent of the neuroleptic use was accounted for by youths in the SSI and foster care groups. There were far smaller disparities in usage rates by eligibility category for stimulants and antidepressants. Medication rates in the S-CHIP group were uniformly lower than in the TANF group for the three drug classes and for any psychotropic, largely because of the larger two- to four-year-old population in the S-CHIP group.
The findings from the multivariate logistic regression analysis account for the potential modifying effect of eligibility category on racial disparities with adjustment for age and gender. Table 4 lists the logistic regression results for main effects (model 1) and for the full model (model 2) in terms of beta coefficients and significance tests. The interaction of race and eligibility was found to be significant and was thus included in the multivariate logistic regression analysis. As shown in Table 5, the likelihood of white youths having a psychotropic medication dispensed was 2.2 times greater than for black youths if they were in foster care or were receiving SSI. By contrast, the disparity was 3.2 to 3.8 times greater for white youths than black youths in the S-CHIP and TANF groups. The table also shows that among the three medication classes, the antidepressant white-black disparity expressed as an odds ratio was most prominent regardless of the eligibility category. Comparing youths from the "other" racial category with black youths indicated only minor mainly nonsignificant disparities (range of odds ratios=.51 to 1.18).
Discussion
The major findings of this study are that racial disparities differed depending on the eligibility category by which a youth qualifies for Medicaid. First, the white-black disparity was significantly lower for the SSI and foster care groups (2.2-fold) than for the TANF and S-CHIP groups (3.8 and 3.2, respectively). Second, the racial composition of the S-CHIP population was markedly different from that of the other categories. Black enrollees accounted for 46 percent of the S-CHIP category, whereas they made up 68 percent of the TANF category. Third, Medicaid eligibility categories in themselves had a profound influence on psychotropic medication patterns among youths, revealing up to sixfold variations among categories. Finally, youths in the SSI and foster care categories accounted for 67 percent of all those with neuroleptic prescriptions. Before discussing how these findings might influence future studies of racial disparities in mental health care, we review the findings with respect to previous studies.
The previously reported disparity in race-specific psychotropic medication prevalence (2) was replicated but has now been shown to vary prominently by eligibility category, even after the data were adjusted for age and gender. The SSI and foster care groups had almost half the level of white-black disparity with respect to psychotropic medication treatment as the TANF and S-CHIP populations (twofold compared with three- to fourfold) (Table 5). The smaller disparity in the SSI and foster care groups could be accounted for by greater federal and state pressure for the treatment of impaired and court- or agency-placed youths and by the severity of their psychiatric or behavioral conditions.
Racial disparities in nonpsychotropic medical treatments among youths have been documented (5), although these disparities are smaller than those for psychotropic medications (2,34). In a recent study of youths in the S-CHIP, there was an independent effect of race or ethnicity on some health service variables in a four-state analysis, which led the authors to conclude that ensuring access to services is not sufficient to ensure utilization among nonwhite enrollees (35). Thus additional demographic factors related to race or ethnicity should be considered, such as family structure (for example, single-parent families) and whether a usual source of care was present before entry into the S-CHIP. Other factors that should be pursued in future research concern cultural perspectives, given that parental attitudes toward the use of medication for behavioral disorders and skepticism about effectiveness and safety have been documented to vary by race in parent surveys of mental health service utilization (10,36).
To further clarify these psychotropic medication disparities, future investigations will require prospective cohort studies of the therapeutic outcome (treatment duration, improvement, and satisfaction) in Medicaid and non-Medicaid community-treated populations (37). Although the number of Hispanic youths enrolled in Medicaid in the state was not sufficient to permit analysis of this subgroup, immediate attention to the Hispanic subgroup is desirable given this group's large representation in Medicaid populations across the United States.
A second objective of this study was to assess the use of psychotropic medications among S-CHIP enrollees independent of race. As expected, psychotropic utilization in the S-CHIP group was similar to that in the TANF group, with a fivefold lower use in the S-CHIP group compared with the SSI and foster care groups. This disparity is consistent with the findings of the study by Harman and colleagues (32) of psychotropic medication expenditures in 1995 and the single-county study by dosReis and colleagues (33) of the prevalence of psychotropic medication use in 1996. Both studies found a six- to tenfold higher use in the SSI and foster care categories compared with the low-income Medicaid category (then Aid to Families With Dependent Children). The finding that youths in foster care and those with federally documented disability (SSI) have a relatively high prevalence of psychotropic medication use is understandable given that those youths have high rates of psychiatric disorders (15,31,32).
To our knowledge, a comparison of the TANF and S-CHIP groups with respect to psychotropic medication use has not previously been conducted. Even though the families who qualify for the S-CHIP are more educated and financially advantaged than those who receive TANF (38), the demographic characteristics of each category's youths were similar with respect to gender and duration of enrollment. It should be noted that S-CHIP survey data are relatively recent and are not consistent across studies, which suggests that more time to accrue S-CHIP enrollees and additional demographic information are needed to precisely describe the differences between the S-CHIP and other insured youth populations (39).
This study of one U.S. state has limited generalizability because of known differences in psychotropic treatment patterns between states (40). The analysis did not cover additional variables of interest—for example, diagnosis, treatment provider, and receipt of other mental health services. Psychotropic medications may have been prescribed for nonpsychiatric indications, although diagnosis-specific utilization was beyond the scope of this study. Furthermore, our previous experience with diagnosis and use of antidepressants leads us to conclude that the group of nonpsychiatric users is relatively small compared with the psychiatric users (28). The psychotropic medications prescribed may reflect racially biased diagnosis, a situation documented for adults with severe mental disorders but, thus far, not established for youths. Concomitant medication use and duration of medication treatments were not measured. These more detailed analyses are pertinent now that we have established that eligibility categories are crucial to an understanding of the racial disparity in psychotropic prevalence patterns.
Conclusions
By disaggregating the full set of Medicaid prescription data into the four major eligibility categories, future analyses of intergroup differences could better inform research on quality-of-care issues. Future studies should help to detail specific aspects of racial or ethnic mental health treatment disparities. These studies could use Medicaid data to generate new disparity data—for example, for specific conditions and for specific age groups. In addition, eligibility category-specific prevalence findings reported on a regular basis could be useful to identify questions for future studies of clinical outcome, as well as to monitor off-label use, access to care, and culturally based disparities. Linking disparate usage to outcomes and learning from prospective studies why the disparities occur is necessary before embarking on meaningful quality assurance efforts to reduce the disparities. This approach will take time, additional methodologic development, and the will to more fully understand the complexities of community-based care. National population-based data for Medicaid enrollees would be a useful first step.
Dr. Zito, Dr. Zuckerman, and Mr. Gardner are affiliated with the department of pharmaceutical health services research at the University of Maryland, Baltimore, 515 West Lombard Street, Baltimore, Maryland 21201 (e-mail, [email protected]). Dr. Safer is with the Johns Hopkins University School of Medicine in Baltimore. Dr. Soeken is with the School of Nursing at the University of Maryland, Baltimore.
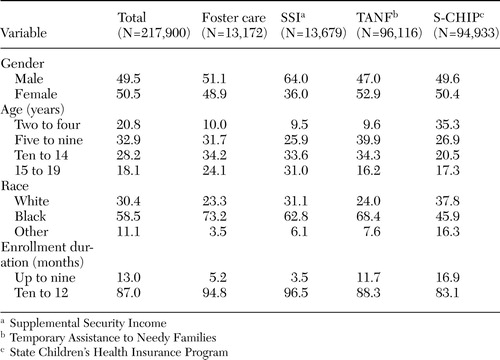 |
Table 1. Characteristics of a Medicaid study population aged two to 19 years, by eligibility category (%)
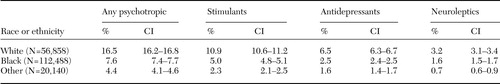 |
Table 2. Unadjusted prevalence of psychotropic medication (%) and 95 percent confidence intervals (CIs) for any psychotropic, stimulant, antidepressant, and neuroleptic medications in a continuously enrolled youth Medicaid population, by race or ethnicity (N=189,486)
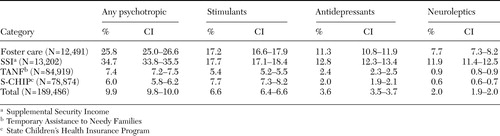 |
Table 3. Unadjusted mean annual prevalence for any psychotropic and three psychotropic classes (%) and 95 percent confidence intervals (CIs) in a continuously enrolled youth Medicaid population and for four Medicaid eligibility categories
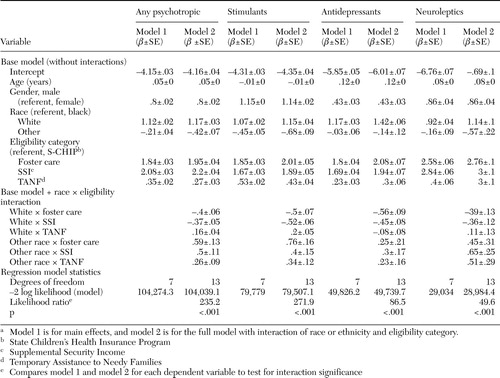 |
Table 4. Logistic regression models of prevalence of psychotropic drug use by age, sex, race or ethnicity, and Medicaid eligibility category(N=189,486)a
a Model 1 is for main effects, and model 2 is for the full model with interaction of race or ethnicity and eligibility category.
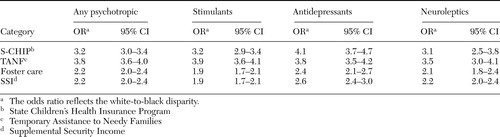 |
Table 5. Likelihood of psychotropic medication dispensing for white youths compared with black youths for four Medicaid eligibility categories, adjusted for age and gender
1. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Washington, DC, US Public Health Service, 2001Google Scholar
2. Zito JM, dosReis S, Safer DJ, et al: Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. Journal of the American Academy of Child and Adolescent Psychiatry 37:179–184, 1998Crossref, Medline, Google Scholar
3. Martin A, VanHoof T, Stubbe D, et al: Multiple psychotropic pharmacotherapy among child and adolescent enrollees in Connecticut Medicaid managed care. Psychiatric Services 54:72–77, 2003Link, Google Scholar
4. Khandker RK, Simoni-Wastila LJ: Differences in prescription drug utilization and expenditures between blacks and whites in the Georgia Medicaid population. Inquiry 35:78–87, 1998Medline, Google Scholar
5. Hahn BA: Children's health: racial and ethnic differences in the use of prescription medications. Pediatrics 95:727–732, 1995Medline, Google Scholar
6. Newacheck PW, Hughes DC, Stoddard JJ: Children's access to primary care: differences by race, income, and insurance status. Pediatrics 97:26–32, 1996Medline, Google Scholar
7. Whaley AL: Cultural mistrust of white mental health clinicians among African Americans with severe mental illness. American Journal of Orthopsychiatry 71:252–256, 2001Crossref, Medline, Google Scholar
8. Mukherjee S, Shukla S, Woodle J, et al: Misdiagnosis of schizophrenia in bipolar patients: a multiethnic comparison. American Journal of Psychiatry 140:1571–1574, 1983Link, Google Scholar
9. DosReis S, Zito JM, Buchanan RW, et al: Antipsychotic dosing and concurrent psychotropic treatments for Medicaid-insured individuals with schizophrenia. Schizophrenia Bulletin 28:607–617, 2002Crossref, Medline, Google Scholar
10. DosReis S, Zito JM, Safer DJ, et al: Parental perceptions and satisfaction with stimulant medication for attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics 324:1–8, 2003Google Scholar
11. Bussing R, Schoenberg NE, Perwien AR: Knowledge and information about ADHD: evidence of cultural differences among African-American and white parents. Social Science and Medicine 46:919–928, 1998Crossref, Medline, Google Scholar
12. Padgett DK, Patrick C, Burns BJ, et al: Ethnicity and the use of outpatient mental health services in a national insured population. American Journal of Public Health 84:222–226, 1994Crossref, Medline, Google Scholar
13. American Academy of Pediatrics: Medicaid policy statement. Pediatrics 104:344–347, 1999Crossref, Medline, Google Scholar
14. Shatin D, Levin R, Ireys HT, et al: Health care utilization by children with chronic illnesses: a comparison of Medicaid and employer-insured managed care. Pediatrics 102:e44, 1998Google Scholar
15. Kuhlthau K, Perrin JM, Ettner SL, et al: High-expenditure children with supplemental security income. Pediatrics 102:610–615, 1998Crossref, Medline, Google Scholar
16. Kelleher KJ, Childs GE, Wasserman RC, et al: Insurance status and recognition of psychosocial problems. Archives of Pediatrics and Adolescent Medicine 151:1109–1114, 1997Crossref, Medline, Google Scholar
17. Kelleher KJ, McInerny TK, Gardner WP, et al: Increasing identification of psychosocial problems:1979–1996. Pediatrics 105: 1313–1321, 2000Google Scholar
18. Starfield B, Gross E, Wood M, et al: Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics 66:159–167, 1980Medline, Google Scholar
19. Kelleher KJ, Hohmann AA, Larson DB: Prescription of psychotropics to children in office-based practice. American Journal of Diseases of Children 143:855–859, 1989Medline, Google Scholar
20. Zito JM, Safer DJ, dosReis S, et al: Psychotherapeutic medication patterns for youths with attention deficit hyperactivity disorder. Archives of Pediatrics and Adolescent Medicine 153:1257–1263, 1999Crossref, Medline, Google Scholar
21. Boles M, Lynch FL, DeBar LL: Variations in pharmacotherapy for attention deficit hyperactivity disorder in managed care. Journal of Child and Adolescent Psychopharmacology 11:43–52, 2001Crossref, Medline, Google Scholar
22. DeBar LL, Lynch F, Powell J, et al: Use of psychotropic agents in preschool children: associated symptoms, diagnoses, and health care services in a health maintenance organization. Archives of Pediatrics and Adolescent Medicine 157:121–123, 2003Crossref, Medline, Google Scholar
23. Goodwin R, Gould MS, Blanco C, et al: Prescription of psychotropic medications to youths in office-based practice. Psychiatric Services 52:1081–1087, 2001Link, Google Scholar
24. Halfon N, Berkowitz G, Klee L: Mental health service utilization by children in foster care in California. Pediatrics 89:1238–1244, 1992Medline, Google Scholar
25. Snowden LR, Cuellar AE, Libby AM: Minority youth in foster care. Medical Care 41:264–274, 2003Medline, Google Scholar
26. Shireman TI, Olson BM, Dewan NA: Patterns of antidepressant use among children and adolescents. Psychiatric Services 53:1444–1450, 2002Link, Google Scholar
27. Zito JM, Safer DJ, dosReis S, et al: Psychotropic practice patterns for youth: a ten-year perspective. Archives of Pediatrics and Adolescent Medicine 157:17–25, 2003Crossref, Medline, Google Scholar
28. Zito JM, Safer DJ, dosReis S, et al: Rising prevalence of antidepressant treatments for US children and adolescents. Pediatrics 109:721–727, 2002Crossref, Medline, Google Scholar
29. Zito JM, Safer DJ, dosReis S, et al: Trends in the prescribing of psychotropic medications to preschoolers. JAMA 283:1025–1030, 2000Crossref, Medline, Google Scholar
30. Rappley MD, Eneli IU, Mullan PB, et al: Patterns of psychotropic medication use in very young children with attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics 23:23–30, 2002Crossref, Medline, Google Scholar
31. Takayama JI, Bergman AB, Connell FA: Children in foster care in the state of Washington. JAMA 271:1850–1855, 1994Crossref, Medline, Google Scholar
32. Harman JS, Childs GE, Kelleher KJ: Mental health care utilization and expenditures by children in foster care. Archives of Pediatric and Adolescent Medicine 154:1114–1117, 2000Crossref, Medline, Google Scholar
33. DosReis S, Zito JM, Safer DJ, et al: Mental health services for youths in foster care and disabled youths. American Journal of Public Health 91:1094–1099, 2001Crossref, Medline, Google Scholar
34. Edwards JN, Bronstein J, Rein DB: Do enrollees in "look-alike" Medicaid and SCHIP programs really look alike? Health Affairs 21(3):240–248, 2002Google Scholar
35. Shone LP, Dick AW, Brach C, et al: The role of race and ethnicity in the State Children's Health Insurance Program (SCHIP) in four states: are there baseline disparities, and what do they mean for SCHIP? Pediatrics 112:e521-e532, 2003Google Scholar
36. Bussing R, Gary FA, Mills TL, et al: Parental explanatory models of ADHD: gender and cultural variations. Social Psychiatry and Psychiatric Epidemiology 38:563–575, 2003Crossref, Medline, Google Scholar
37. President Bush's New Freedom Commission Report. Washington, DC, 2003Google Scholar
38. Byck GR: A comparison of the socioeconomic and health status characteristics of uninsured, State Children's Health Insurance Program-eligible children in the United States with those of other groups of insured children: implications for policy. Pediatrics 106:14–21, 2000Crossref, Medline, Google Scholar
39. Brach C, Lewit EM, VanLandeghem K, et al: Who's enrolled in the State Children's Health Insurance Program (SCHIP)? An overview of findings from the Child Health Insurance Research Initiative (CHIRI). Pediatrics 112:e499-e507, 2003Google Scholar
40. Cox ER, Motheral BR, Henderson RR, et al: Geographic variation in the prevalence of stimulant medication use among children 5 to 14 years old: results from a commercially insured US sample. Pediatrics 111:237–243, 2003Crossref, Medline, Google Scholar



