Follow-Up of Pentagon Employees Two Years After the Terrorist Attack of September 11, 2001
Abstract
OBJECTIVE: This study examined probable posttraumatic stress disorder (PTSD) and probable depression, degree of psychological distress, and rates of mental health treatment in a sample of Pentagon staff two years after the terrorist attack of September 11, 2001. METHODS: Anonymous surveys were administered to staff at one Pentagon work center. Respondents were asked about exposure to the attack; injuries; exposure to dead bodies or families of the deceased; psychological distress; and use of mental health services. Probable PTSD and depression were assessed with the PCL-17 and the PHQ-9. RESULTS: A total of 267 responses were received. Fourteen percent of the sample had probable PTSD, and 7 percent had probable depression. Staff who were at the Pentagon on the day of the attack were more likely to have probable PTSD and probable depression. Exposure through watching television was not associated with a higher frequency of probable PTSD, probable depression, or distress. Injury during the attack was associated with a higher frequency of probable PTSD, probable depression, and distress. Respondents who were exposed to dead bodies or who acted as lay counselors to families of the deceased were more likely to have probable PTSD and depression and to report chronic distress. Of those with probable PTSD, 70 percent made at least one mental health visit during the next two years. Of those with probable depression, 74 percent reported at least one mental health visit. CONCLUSIONS: Direct exposure to the September 11 terrorist attack on the Pentagon, injury during the attack, and exposure to dead bodies or acting as a lay counselor to families of persons who were killed during the attack were all associated with higher frequencies of probable psychiatric illness and higher levels of psychological distress two years after the attack. Among survivors who had probable psychiatric illness, more than two-thirds received mental health treatment after the attack.
The long-term effects of terrorism on individuals and on communities have not been extensively studied. After the terrorist attacks of September 11, 2001, there were high levels of psychological distress across the nation (1,2,3). In New York City, rates of probable posttraumatic stress disorder (PTSD) ranged from 7.5 percent to 20 percent in the months after the attacks (4). Despite high levels of initial distress, a community sample in New York City demonstrated that rates of mental health service use were only moderately changed four to five months after the attacks, indicating that stress symptoms resolved or that individuals who had symptoms did not seek treatment (5).
The degree of exposure to traumatic events has been repeatedly linked to levels of illness during periods of follow-up. Of those who were directly exposed to the Oklahoma City terrorist attack, 34 percent had PTSD during the six months after the attack (6). Physical injury has also been clearly associated with elevated levels of PTSD and depression (7). The relationship between the combined exposure to a terrorist attack and injury incurred during the attack and subsequent posttraumatic illness has not been well described. National studies showed that posttraumatic symptoms were present among 5.8 percent of the population six months after the September 11 attacks, even though a majority had no direct exposure (3). The lasting effects of indirect exposure and whether such exposure results in clinically significant problems are not known.
The terrorist attack on the Pentagon left 125 Pentagon employees dead. Surveys of Pentagon employees seven and 13 months after the attack showed significant rates of probable PTSD and probable depression as well as lower perceived safety among persons who were directly exposed to the attack (8,9). One work center lost 24 of its 220 staff members (11 percent) during the attack.
The study reported here examined the current frequency of probable PTSD and probable depression among current members of the work center two years after the attack. Associations between direct exposure to the attack, physical injury, seeing or working with dead bodies or families of the deceased, indirect exposure to the attacks through the media, and rates of mental heath care treatment among persons with probable PTSD or depression were also examined.
Methods
Participants
Twenty-five months after the terrorist attack on the Pentagon and after review and approval by our institutional review board, 620 military and civilian staff who were currently assigned to the work center were given an anonymous Internet-based questionnaire that included discussions of risks and benefits of the study and provided a contact point for any questions or concerns. To preserve confidentiality, the institutional review board waived the requirement for written informed consent. Questionnaires were collected during the period November 1 to November 30, 2003.
Exposure to the attack
Study participants were asked to identify their location on the day of the attack: at the Pentagon, elsewhere in the D.C. metropolitan area, or not in the D.C. metropolitan area. Respondents who reported their location as the Pentagon were compared with those who were not at the Pentagon. Among respondents who were at the Pentagon during the attack, those who reported injury were compared with those who did not report injury. Participants were asked whether they saw anyone seriously injured or killed, whether they handled dead bodies, and whether they worked as a casualty assistance officer (lay counselor to the families of persons killed in the attack). Respondents who reported any of these exposures were compared with those who did not. Participants were asked to identify how many hours of television coverage of the attacks they watched during the days after the terrorist attacks. Among respondents who were not at the Pentagon on the day of the attack, those who watched three or more hours of television coverage per day were compared with those who watched less than three hours.
PTSD, depression, and psychological distress
Probable PTSD was assessed with the 17-item PTSD Checklist (PCL-17) (10). The PCL-17 lists all symptoms of PTSD outlined in DSM-IV. Respondents rate how much they had been bothered by that problem in the past month. Each question was worded so as to be related to the respondent's experience with the attack at the Pentagon. Possible responses were 1, not at all, 2, a little bit, 3, moderately, 4, quite a bit, and 5, extremely.
When this scale is used as a screening tool, responses are summed to produce a range from 17 to 85. Studies in primary care settings have validated the use of PCL-17 scores of 30 or greater as indicative of probably PTSD (sensitivity .86, specificity .76) (11,12). In this study we applied a more clinically based indicator of presence of probable PTSD by using DSM-IV criteria: one intrusion symptom, three avoidance symptoms, and two hyperarousal symptoms, each present at the level of moderate or higher during the previous month. Respondents who met criteria for PTSD by this method in this sample had a mean±SD PCL-17 score of 55.5±10.33 (range, 34 to 85), which indicates endorsement of a majority of the symptoms at the level of bothered "quite a bit" or bothered "extremely" by most respondents who met the criteria.
Probable depression was assessed with use of the Patient Health Questionnaire Depression Scale (PHQ-9) (13). Probable depression is present when at least five of the nine symptoms have been present "more than half the days" or "nearly every day" in the past two weeks and one of the symptoms is depressed mood or anhedonia. When compared against structured clinical evaluations in primary care settings, the PHQ-9 demonstrated 74 percent sensitivity and 94 percent specificity for this application (14).
Psychological distress was assessed with a question asking respondents how much they were bothered by symptoms of depression or PTSD during three periods: before September 2001, September 2001 to March 2002, and March 2002 to the present. Possible responses for each item were not at all, a little bit, moderately, quite a bit, or extremely. Psychological distress was considered to be present when participants reported being bothered moderately to extremely. Participants were rated as having acute psychological distress when they reported psychological distress only in the six months after the attack. They were rated as having chronic psychological distress when they reported psychological distress during the first six months and subsequent 19 months but not before the attack.
Use of mental health services
Respondents were asked to identify how many times they had seen a psychiatrist, a psychologist, or a social worker during the three periods September 11, 2000, to September 11, 2001; September 11, 2001, to September 11, 2002; and September 11, 2002, to the present. Those who reported at least six mental health visits during each of these periods were considered to be receiving ongoing mental health treatment.
Statistical analyses
Risk factors for probable PTSD, depression, and psychological distress were evaluated by binary logistic regression. The demographic variables gender, age, race (Caucasian versus other), and educational level (college degree or advanced degree versus other) were entered as covariates with the variable under examination. The estimate of the odds ratio and its 95 percent confidence interval (CI) are reported. Statistical analyses were performed with use of SPSS for Windows (version 11).
Results
We received 267 responses, for a 43 percent response rate. The mean±SD age of the respondents was 46.4±7.5 years; 53 percent were female (N=142), 77 percent were married (N=206), and 77 percent had a college or postgraduate degree (N=206). The racial breakdown of the sample was 72 percent Caucasian (N=192), 21 percent African American (N=54), 4 percent Hispanic (N=10), 2 percent Asian (N=6), and 1 percent Native American (N=3); 1 percent (N=2) reported mixed racial backgrounds. Compared with the work center as a whole, the study sample contained more women (53 percent [N=142] compared with 45 percent at the work center), senior officers (major through colonel, 36 percent [N=96] compared with 28 percent in work center), and middle and senior civilian managers (GS-9 and above, 47 percent [N=125] compared with 34 percent).
A total of 129 respondents (48 percent) were at the Pentagon on the day of the attack. Twenty-eight respondents (22 percent of those present at the Pentagon during the attack) were injured. Sixty-four respondents (24 percent) reported seeing someone killed, working with dead bodies, or working as a counselor to families of the deceased. Among the 138 respondents who were not at the Pentagon during the attack, 64 (46 percent) reported watching at least three hours of television coverage of the attacks per day.
Forty-two respondents (16 percent) had probable PTSD or depression. Thirty-seven respondents (14 percent) met criteria for probable PTSD, and 19 respondents (7 percent) met criteria for probable depression. Fourteen respondents (5 percent) met criteria for both probable PTSD and probable depression. Nine respondents (4 percent) reported psychological distress before the attack, 90 respondents (34 percent) reported acute psychological distress after the attack, and 48 respondents (18 percent) reported chronic psychological distress. When persons who met criteria for current probable PTSD or depression were excluded, 55 respondents (24 percent) reported acute distress, and 19 (8.4 percent) reported chronic distress.
When all demographic variables were examined simultaneously, no associations were found between gender, age, race, or educational level and the risk of probable PTSD. Non-Caucasians were 3.66 times as likely to meet depression criteria as Caucasians (CI=1.24 to 10.80, Wald χ2=5.50, df=1, p=.019). Women were 2.30 times as likely as men to experience acute psychological distress (CI=1.25 to 4.25, Wald χ2=7.10, df=1, p=.008) but not chronic distress. No other associations were noted between demographic variables and risk of probable depression or psychological distress.
Table 1 lists the frequencies of probable PTSD, probable depression, and psychological distress on the basis of exposure during and after the attack. After demographic factors were controlled for, persons who were at the Pentagon during the attack were 5.23 times as likely to have probable PTSD (CI=2.04 to 1,341, Wald χ2=11.84, df=1, p=.001) and were 3.09 times as likely to have probable depression (CI=1.05 to 14.56, Wald χ2=4.13, df=1, p=.042) compared with respondents who were not at the attack site. Those at the Pentagon were 3.96 times as likely to report acute psychological distress (CI=2.16 to 7.27, Wald χ2=19.79, df=1, p<.001) and were 6.70 times as likely to report chronic psychological distress (CI=2.80 to 16.02, Wald χ2=18.31, df=1, p<.001). Among those who were not at the Pentagon, no association was found between the number of hours of television watched and subsequent meeting of PTSD or depression criteria or reporting of acute or chronic psychological distress.
After demographic factors were controlled for, participants who were at the Pentagon and were injured were 7.94 times as likely to have probable PTSD (CI=2.76 to 22.84, Wald χ2=14.75, df=1, p<.001) and were 4.94 times as likely to have probable depression (CI=1.32 to 18.41, Wald χ2=5.65, df=1, p=.017) as participants who were at the Pentagon and not injured. Those who were injured were 7.20 times as likely to report acute psychological distress (CI=2.43 to 21.39, Wald χ2=12.65, df=1, p<.001) and were 7.42 times as likely to report chronic psychological distress (CI=2.74 to 20.09, Wald χ2=15.59 df=1, p<.001).
After demographic variables and location on the day of the attack were controlled for, respondents who were exposed to dead bodies or who worked with families of the deceased were 5.78 times as likely to have probable PTSD (CI=2.08 to 16.04, Wald χ2=11.36, df=1, p=.001) and 5.21 times as likely to have probable depression (CI=1.32 to 20.49, Wald χ2=5.57, df=1, p=.018) compared with those who were not exposed. Those who were exposed to dead bodies or who acted as family counselors were 2.71 times as likely to have chronic psychological distress (CI=1.16 to 6.34, Wald χ2=5.28, df=1, p=.022). No association was found between exposure to dead bodies or serving as a family counselor and acute psychological distress.
Seventy respondents (26 percent) reported at least one mental health visit in the two years after the attack, and 27 (10 percent) reported at least six visits during the period. None of the 37 respondents with probable PTSD had been receiving mental health treatment before the attack. Twenty-six respondents with probable PTSD (70 percent) reported at least one mental health visit during the two-year period after the attack. Sixteen (43 percent) reported at least six visits during the first year after the attack, and 12 (32 percent) remained in treatment during the second year after the attack. Of the 19 respondents with probable depression, one (5 percent) was receiving treatment before the attack. Fourteen (74 percent) reported at least one mental health visit in the two years after the attack, and nine (47 percent) reported at least six mental health visits during that period. Eight respondents (42 percent) were in ongoing treatment during the first year, and seven (37 percent) were in ongoing treatment during the second year.
Discussion
This population provided a unique opportunity to examine the long-term effects of the terrorist attacks of September 2001 on a unique group that was representative of corporate staff and leadership at the Pentagon. Eighty-three percent of respondents were officers or middle- and senior-level civilian managers whose daily work has a direct effect on the activities of tens of thousands of personnel and millions of dollars of facilities and material around the world. Approximately half the sample had direct exposure to the attack, and half had indirect exposure, which provided us with naturalistic exposure comparison groups. All respondents had a similar work environment, and all had access to health care through their health insurance plans or through free mental health services provided after the attack.
Direct exposure to the attack was associated with a higher prevalence of probable PTSD and probable depression and significant levels of distress that persisted for more than two years. In contrast to previous reports of distress possibly associated with television exposure (3), in this sample media exposure in the absence of direct exposure to the attacks was not associated with risk of current probable PTSD or depression or with the degree of psychological distress reported since the attack. This finding is consistent with other reports of associations between higher rates of probable PTSD and combined television watching and direct exposures but not with television watching alone (15). The group with high television exposure did have higher frequencies of illness and distress, but the difference was not statistically significant. The relationship with media exposure may also be less evident in this sample because other exposures followed the attack, such as knowing someone who was killed during the attack or currently working at the site of the attack—which was also a possible site for future attacks.
Injury during the attack was associated with a substantially increased risk of probable PTSD, probable depression, and psychological distress among staff who were at the Pentagon during the attack. Exposure to dead bodies or working with families of the deceased also increased the risk of probable PTSD, independent of the staff member's location during the attack. These are important factors to consider in determining the populations at highest risk of psychiatric illness and distress after a terrorist attack.
In this sample, 70 percent of persons with probable PTSD and 74 percent of those with probable depression reported at least one mental health visit during the two years after the attack on the Pentagon. Forty-three percent of those with probable PTSD and nearly half of those with probable depression had been receiving ongoing mental health treatment at some point during the two-year period. Sampling of residents in New York City four to five months after the attack on the World Trade Center indicated that 22 percent of those who met screening criteria for probable PTSD and 27 percent of those who met criteria for probable depression had obtained mental health services in the preceding month (5). This study used different screening instruments and different sampling techniques that may account in part for differences in health care use between the samples. Higher rates of use in the Pentagon sample also may have been a consequence of full employment, health care benefits, and access to free mental health care for matters related to the attack. Because our study had a longer follow-up period, the persistence of symptoms may have also resulted in higher rates of care seeking during the study period. In addition, extensive workplace outreach programs, strong endorsement of these programs by leadership, and availability of services at or near the workplace may have contributed to long-term care-seeking behavior.
Because of the study recruitment process and selection biases, the rates of probable illness or distress cannot be generalized to other populations. Also, although we used well-validated survey measures, our assessments could identify only probable PTSD or depression, not a clinical diagnosis (16,17). In addition, participants were asked to recollect levels of exposure, distress, and use of mental health services across time, which could have produced recall bias influenced by current symptoms and function. Also, no data are available on the reliability of the distress and mental health service use questions.
Conclusions
Surveyed staff who were exposed to the attack on the Pentagon had a higher prevalence of probable psychiatric illness two years after the attack. Direct exposure to the attack was also associated with higher levels of reported acute and chronic distress. Although greater exposure to media coverage of the September 11 attacks was associated with high levels of initial distress in previous studies, that association was not evident among persons who were not directly exposed in this sample two years later.
Government and business leaders as well as disaster medical planners should maintain awareness that some individuals who are exposed to acts of terrorism will need long-term access to mental health services. Those directly exposed to attacks, those who are injured, and those who are exposed to dead bodies or who work as family counselors are at higher risk of experiencing persisting posttraumatic symptoms and distress.
The authors are affiliated with the Department of Psychiatry, B-3068, Uniformed Services University, 4301 Jones Bridge Road, Bethesda, Maryland 20814 (e-mail, [email protected]).
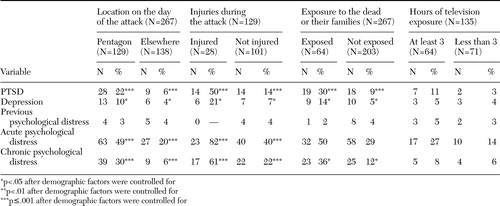 |
Table 1. Frequency of probable posttraumatic stress disorder (PTSD), probable depression, and psychological distress on the basis of exposure during and after the terrorist attack on the Pentagon on September 11, 2001
1. Schlenger WE, Caddell JM, Ebert L, et al: Psychological reaction to terrorist attacks: findings from the national study of Americans' reactions to September 11. JAMA 288:581–588,2002Crossref, Medline, Google Scholar
2. Schuster MA, Stein BD, Jaycox LH, et al: A national survey of stress reactions after the September 11, 2001 terrorist attacks. New England Journal of Medicine 345:1507–1512,2001Crossref, Medline, Google Scholar
3. Silver RC, Holman EA, McIntosh DN, et al: Nationwide longitudinal study of psychological responses to September 11. JAMA 288:1235–1244,2002Crossref, Medline, Google Scholar
4. Galea S, Ahern J, Resnick H, et al: Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine 346:982–987,2002Crossref, Medline, Google Scholar
5. Boscarino JA, Galea S, Adams RE, et al: Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatric Services 55:274–283,2004Link, Google Scholar
6. North CS, Nixon SJ, Shariat S, et al: Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA 282:755–762,1999Crossref, Medline, Google Scholar
7. O'Donnell ML, Creamer M, Pattison P, et al: Psychiatric morbidity following injury. American Journal of Psychiatry 161:507–514,2004Link, Google Scholar
8. Grieger TA, Fullerton CS, Ursano RJ. Posttraumatic stress disorder, alcohol use, and perceived safety after the terrorist attack on the Pentagon. Psychiatric Services 54:1380–1382,2003Link, Google Scholar
9. Grieger TA, Fullerton CS, Ursano RJ: Posttraumatic stress disorder, depression, and perceived safety 13 months following the terrorist attack on the Pentagon. Psychiatric Services 55:1061–1063,2004Link, Google Scholar
10. Weathers F, Ford J: Psychometric properties of the PTSD Checklist, in Measurement of Stress, Trauma, and Adaptation. Edited by Stamm BH. Lutherville, Md, Sidran, 1996Google Scholar
11. Walker EA, Newman E, Dobie DD, et al: Validation of the PTSD Checklist in an HMO sample of women. General Hospital Psychiatry 24:375–380,2002Crossref, Medline, Google Scholar
12. Lang AJ, Laffaye C, Satz LE, et al: Sensitivity and specificity of the PTSD Checklist in detecting PTSD in female veterans in primary care. Journal of Traumatic Stress 16:257–264,2003Crossref, Medline, Google Scholar
13. Kroenke K, Spitzer RL: The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals 32:509–515,2002Crossref, Google Scholar
14. Kroenke K, Spitzer RL, Williams JB: The PHQ-9. Journal of General Internal Medicine 16:606–613,2001Crossref, Medline, Google Scholar
15. Ahern J, Galea S, Resnick H, et al: Television images and psychological symptoms after the September 11 terrorist attacks. Psychiatry 65:289–300,2002Crossref, Medline, Google Scholar
16. Marshall RD, Galea S: Science for the community: assessing mental health after 9/11. Journal of Clinical Psychiatry 65(suppl 1):37–43,2004Medline, Google Scholar
17. North CS, Pfefferbaum B: Research on the mental health effects of terrorism. JAMA 288:633–636,2002Crossref, Medline, Google Scholar



