Mental Health Service and Medication Use in New York City After the September 11, 2001, Terrorist Attack
Abstract
OBJECTIVE: A survey assessed use of mental health services and psychiatric medications in New York City four to five months after the September 11, 2001, attack on the World Trade Center. METHODS: A telephone survey using random-digit dialing was conducted among 2,001 adult householders. RESULTS: During the interviews, 7.6 percent of respondents reported use of mental health services in the past 30 days and 7.7 percent reported use of psychiatric medications. Factors associated with service use included experiencing four or more lifetime traumatic events, experiencing two or more stressful life events in the past 12 months, having posttraumatic stress disorder (PTSD), and having depression. African-American and Hispanic respondents were less likely than white respondents to use services. Greater service use after the attack was associated with a graduate education, increased alcohol use after the attack, and depression. Factors associated with medication use included being in either of two age groups (25 to 44 years and 45 to 64 years), having a primary care physician, experiencing two or more stressful life events in the past 12 months, and having depression. African-American and Hispanic respondents were less likely than white respondents to be taking medications. Greater use after the attack was associated with having depression. Mental health visits in Manhattan appeared to decrease compared with the first two months after the attack. However, among respondents with PTSD or depression, those who were nonwhite, younger, without a primary care physician, or without health insurance were less likely to use postdisaster services. CONCLUSIONS: Service use after the terrorist attack was related to mental status and to the amount of trauma and stress experienced. Overall, white respondents, those aged 25 to 64 years, and those with a primary care physician were more likely to use services.
Major disasters are rare, but studies suggest that psychiatric disorders, such as posttraumatic stress disorder (PTSD) and depression, are common among survivors (1,2,3). Furthermore, these effects may be lasting in the case of disasters that involve significant loss of life (4), although some research suggests the contrary (5). The terrorist attack in New York City on September 11, 2001, resulted in one of the largest death tolls of any disaster in the United States. An initial study in Manhattan of the psychological impact of the attack indicated that 7.5 percent of adults had symptoms consistent with PTSD that were related to the attack and 9.7 percent had symptoms consistent with depression (6).
Although use of mental health services after disasters has been documented (7,8), few investigations have focused on population-level service use. Much of the research has examined the impact on direct survivors, and different measures and time frames have been used, which makes generalizations difficult (9,10,11,12). Effective health planning requires assessment of population-level service use and needs (13). To estimate the prevalence and correlates of mental health service use in New York City after the attack, we conducted a telephone survey of adults four to five months after this event (14). The results were compared with those from a survey of Manhattan residents that we conducted one to two months after the event (15,16).
Methods
All English- or Spanish-speaking adults older than 17 years who lived in New York City and had a telephone were potential participants. Sample selection was based on random-digit dialing, with oversampling of persons living in Manhattan. After we obtained verbal consent, one adult per household was randomly selected for an interview. Trained interviewers using a computer-assisted telephone interviewing system conducted the interviews. Both English and Spanish versions of the questionnaire were used. Questionnaires were translated into Spanish and then back-translated by bilingual persons whose native language was English to ensure linguistic and cultural appropriateness. Eight percent of the interviews were conducted in Spanish. A protocol was in place to provide assistance to participants who required counseling. The mean duration of the interview was 35 minutes. The surveys were conducted in January and February 2002.
Sampling weights were developed to correct for selection bias related to the number of telephone numbers and persons in each household as well for the oversampling of Manhattan residents. Our survey cooperation rate was based on the sum of the number of completed interviews, quota-outs (those who were eligible for the interview but who were excluded because the quota for borough or gender was exceeded), and screen-outs (those who were younger than 17 years old, who did not speak English or Spanish, or did not live in the city) divided by the sum of completed interviews, quota-outs, screen-outs, refusals, and premature terminations of the interview (17). On the basis of these calculations, the cooperation rate in our survey was 64 percent. Our survey response rate, which was based on the number of completed and partial interviews divided by the count of eligible residential telephone numbers (17), was 44 percent.
The institutional review board of the New York Academy of Medicine (NYAM) approved the study protocols. Our surveys were conducted by Schulman, Ronca, and Bucuvalas, Inc. (SRBI), of New York City, a firm experienced in conducting health interviews using telephone surveys of disaster survivors, victims of sexual assault, and combat veterans. All interviewers were trained, supervised, and monitored by senior staff of both SRBI and NYAM.
Because one of our objectives was to compare service use in the January-February survey with the results from the earlier survey, we briefly describe that data collection effort. The interviews for the earlier survey were conducted in October and November 2001 among English- or Spanish-speaking adults. The sampling frame was adult residents living in Manhattan south of 110th Street. As with the January-February survey, respondents were selected by using random-digit dialing in the manner described. For the earlier survey, we completed 1,008 interviews and achieved a cooperation rate of 64 percent. Detailed reports of the previous survey have been published elsewhere (6,15,16).
Dependent variables
We asked whether participants sought help for personal or emotional problems from a helping professional, such as a psychiatrist, a psychologist, a counselor, a social worker, a pastoral counselor, or some other helping professional or from a self-help group in their lifetime, in the month before the terrorist attack, and in the past month. When participants answered "yes," the interviewer asked them to report the number of times that they had seen that service provider (15). These questions were adapted from previous disaster research (18) and modified on the basis of the National Comorbidity Survey (19,20).
We also asked respondents about whether they had taken any psychiatric medications prescribed by a physician, such as antidepressants or sleeping pills for emotional problems, in the month before the attack and in the past month. We asked those who took medications to report the number of days that they had taken them. These survey questions were adapted from items in the National Comorbidity Survey (19,20).
On the basis of previous research (16), we developed two variables for further analyses: increased mental health visits and increased psychiatric medication use. Mental health visits were classified as "increased" if a person had an increase of one or more mental health visits in the past month compared with the month before the attack. Psychiatric medication use was defined as increased if a person had an increase of one or more medication days in the past month compared with the month before the attack.
Independent variables
We collected information about demographic variables that might affect use of mental health services or medications, including age, race or ethnicity, gender, household income, educational level, and marital status. In our analyses, we divided age into four groups, race or ethnicity into five groups, and education into five groups. We also asked respondents whether they had a primary care physician and health insurance coverage. Finally, we asked them about increased alcohol use after the disaster, and we used this variable in our analyses.
We asked participants to report the number of traumatic events to which they had been exposed in their lifetime (21) and grouped the responses into four categories: no events, one event, two or three events, and four or more events. We also asked about stressful life events, such as the death of a spouse, that the participant experienced in the 12 months before the attack (18). We divided these responses into three categories: no events, one event, and two or more events. We also assessed ten specific events or experiences associated with the World Trade Center attack, such as whether the respondent had witnessed the attack, had been injured, had lost friends or relatives in the attack, had been displaced, or had lost his or her job (6,15,16). We classified respondents by how far they lived from the disaster site—three miles or more, or less than three miles—and how involved they were in the postdisaster rescue efforts—no, some, or direct involvement.
Our analyses included three mental health measures: PTSD, depression, and a peri-event panic attack—that is, an attack that occurred during the disaster or within a few hours of it. The PTSD measure was used in the National Women's Study (22) and later modified on the basis of DSM-IV criteria (23,24). This scale used a non-event-specific approach for PTSD assessment (22,24). It was designed for administration by trained nonclinical interviewers during a structured telephone survey. The onset of PTSD since the disaster was based on the respondent's meeting diagnostic criteria in the previous four or five months—that is, since the attack. Specifically, a participant was deemed to have PTSD if symptoms were present for the necessary criteria B, C, and D. For our analysis, the measure of onset of PTSD since the disaster did not require the symptoms to be related to the attack. An additional variable was developed for onset of PTSD that was related specifically to the attack (6) and was used for comparison. We found these two PTSD measures to be highly correlated (kappa=.86). Cronbach's alpha for the symptoms used in this scale was reported to be .90 (15). In addition, our PTSD scale has been reported to be highly correlated with the clinician-administered Structured Clinical Interview for DSM-III-R (SCID) (kappa=.71 for current PTSD) (24,25). Since its implementation, this PTSD scale has been used in several large-scale mental health surveys involving more than 16,000 completed telephone interviews (22,26,27,28).
To further validate our PTSD measure, we compared our results with those of the PTSD Check List (PCL) (29), an established screener for PTSD, for a random subsample of 229 participants in our January- February survey. Overall, we found that the PCL had 75 percent sensitivity and 95 percent specificity in detecting PTSD as classified by our PTSD instrument (30). In a receiver operating characteristic analysis (31), we found that a PCL cutoff score of 50 or higher, which is the cutoff score recommended for the instrument, also optimally predicted PTSD when our instrument was used (area under the curve=.97).
Analyses performed for another postdisaster community survey conducted with 2,368 adults in New York City (27) provided additional validity data for our PTSD measure. In the other postdisaster study, we found that a diagnosis of PTSD in the past year was significantly associated with a lower Rosenberg self-esteem score (32) (odds ratio [OR]=7, p<.001), a clinically low mental health score on the 12-item Self-Report scale (SF-12) (33) (OR=8.3, p<.001), and lower reported work quality among employed persons (OR=3.4, p<.001). In addition, a PTSD diagnosis in the past year was associated with meeting the clinical case definitions in the past month on the 18-item Brief Symptom Inventory (BSI-18) (34) for depression (OR=6.8, p<.001), anxiety (OR=7.8, p<.001), and global severity (OR=7.1, p<.001). The correlation coefficients for PTSD symptoms in the past 30 days were .45, .46, and .48 with BSI-18 depression, anxiety, and global severity scales, respectively.
To measure depression we used an adapted version of the SCID's major depressive disorder subscale from the nonpatient version (25), which has been used in other population studies (6,35). Respondents were considered to have major depressive disorder if they reported five or more symptoms listed for the DSM-IV criteria for at least two weeks. Respondents were also asked to report the last time they experienced these symptoms. The research team has had experience with this scale in previous surveys focusing on the World Trade Center disaster (6,14,15). Cronbach's alpha for the eight symptoms used in this scale was .79 (15). We also compared the results for depression in the past 30 days obtained by using our depression scale with those obtained by using the BSI-18 (34) depression scale (27). Overall, the BSI-18 depression scale had 73 percent sensitivity and 87 percent specificity in detecting depression as classified by our depression instrument (27). In a receiver operating characteristic analysis (31), the BSI depression cutoff score of 65 or higher, which is a clinical cutoff for BSI depression, also optimally predicted depression when our instrument was used (area under the curve=.89).
We also found that a diagnosis of depression in the past year as measured by our scale was associated with a lower Rosenberg self-esteem score (OR=8.1, p<.001), a clinically low mental health score on the SF-12 scale (OR=12.8, p<.001), and lower reported work quality among employed persons (OR=4, p<.001). Furthermore, a diagnosis of depression in the past year on our scale was associated with meeting the clinical case definitions on the BSI-18 in the past month for depression (OR= 11.3, p<.001), anxiety (OR=9.7, p<.001), and global severity (OR=13.4, p<.001). The correlation coefficients for depression symptoms in the past 30 days were .52, .52, and .56 with BSI-18 depression, anxiety, and global severity scales, respectively.
The panic attack measure used was a modified version of the Diagnostic Interview Schedule (DIS) subscale for panic (36), phrased to assess peri-event symptoms—those that occurred during or shortly after the terrorist attack; we have used this measure in other telephone surveys (6,15,16). We asked about panic symptoms specifically in the first few hours after the events of September 11. If a participant reported at least four of the symptoms listed for panic attack in the DSM-IV, that person was considered to have a diagnosis of a peri-event panic attack (23).
Statistical analyses
We focused on four outcome variables, all occurring in the past 30 days: visits to mental health professionals, psychiatric medication use, increased mental health visits, and increased psychiatric medication use. We used a pre-post McNemar chi square test to assess the comparison of mental health visits in the 30 days before the attack and in the past 30 days. On the basis of previous research, we identified demographic, mental health, and stress-related variables that might have been associated with postdisaster mental health service use (19,37,38). The unadjusted ORs and 95 percent confidence intervals (CIs) were calculated for these associations. We then used multivariate logistic regression to examine these associations in a predictive model. The models predicted any mental health visits, increased mental health visits, any psychiatric medication use, and increased medication use—all in the past 30 days. In our final multivariate models, only predictor variables with a p value of .05 or less in the initial bivariate analyses (based on the respective overall p values) were selected.
We also tested for interaction effects in the models between age, education, marital status, and race, because these variables have been associated with different utilization rates (13). We used the survey estimation ("svy") commands in Stata, version 7, to generate our point estimates, p values, CIs, and logistic models (39). This approach was needed to adjust the data for our sampling design, which included case weights to correct for overrepresentation of persons in households with more telephone lines and oversampling Manhattan residents. Therefore, our McNemar chi square tests were calculated as follows. First, the Stata survey estimates were conducted by using the survey estimations to generate pre-post percent point estimates. These point estimates were then converted into their respective survey frequencies. Next, these frequencies were entered into the "immediate" Stata command for pre versus post design ("mcci" in epitab command set) and used to generate the McNemar chi square tests.
Additional bivariate analyses were conducted to assess factors related to access to services among participants who met criteria for either PTSD or depression, because an earlier study suggested that younger adults, men, and persons without health insurance faced barriers to obtaining care (40). In addition, we wanted to assess changes in the use of mental health services since our earlier survey (6,15,16). To assess these changes, we used the data from Manhattan, which was the focus of our earlier survey. All p values presented were based on 2-tailed tests.
Results
Among the 2,011 participants in our study, ten persons were eliminated because of missing demographic data. In the remaining sample, 53.5 percent were women, and the mean±SD age was 41±16 years. Of the participants, 39.9 percent were white, 5.3 percent were Asian, 25.3 percent were African American, 24.6 percent were Hispanic, and 4.9 percent were classified as "other." Geographically, at the time of the survey, 18 percent of respondents lived in Manhattan, 16 percent in the Bronx, 29.8 percent in Brooklyn, 30.3 percent in Queens, and 6 percent in Staten Island. The age, gender, race, and regional distributions in our sample were not significantly different from estimates in the 2000 U.S. Census (41). Thus our sampling method or cooperation rate did not appear to lead to demographic biases.
As Table 1 shows, 9 percent of the participants were classified as probably having PTSD in the postdisaster period, 7.8 percent as probably having major depression in the postdisaster period, and 16.7 percent as having had a peri-event panic attack associated with the disaster. In addition, 7.6 percent visited a professional for mental health problems in the past 30 days, and 7.7 percent used psychiatric medications in the past 30 days. More than 95 percent of the sample reported no change in postdisaster mental health visits or medication use. However, 2.7 percent reported more visits in the past 30 days than in the month before the disaster, and 2.8 percent reported more medication use. In addition, 1.3 percent reported visits in the past month but none in the month before the disaster, and 2.8 percent reported medication use in the past month and none in the month before the disaster. Overall, 3.9 percent reported fewer visits in the past month than in the month before the disaster (CI=3 to 4.8) and 1.8 percent reported less use of medications (CI=1.1 to 2.4) (analyses not shown).
Overall, participants' use of mental health services was significantly lower in the fourth and fifth months after the disaster than in the month before the disaster (7.6 percent compared with 8.6 percent; McNemar χ2=5.1, df=1, p=.024). In contrast, overall use of psychiatric medications in the fourth and fifth months after the disaster was significantly higher than in the month before the disaster (7.7 percent compared with 6.8 percent; McNemar χ2=4.4, df=1, p=.035).
Table 2 shows the associations between any postdisaster mental health service use in the fourth and fifth month after the disaster and demographic and exposure-related variables selected for the multivariate model. The adjusted likelihood of mental health service use was significantly lower among African-American and Hispanic respondents than among white respondents. Among the predisaster variables, experiencing four or more lifetime traumatic events and experiencing two or more stressful life events in the 12 months before the attack were positively associated with mental health service use. Two postdisaster variables were positively associated with service use—having PTSD and having an episode of depression.
Predictors of increased use of mental health services after the attack (analyses not shown) were graduate school education (less than high school was the comparison group; OR=8.3, p=.024), increased postdisaster alcohol use (OR=4.5, p<.001), some involvement (but not direct) in rescue or recovery efforts (compared with none; OR=1.9, p=.041), and depression (OR=2.4, p=.02).
As can be seen in Table 3, multivariate analyses showed that African-American and Hispanic respondents were less likely than white respondents to use medication after the attack. Several variables were positively associated with medication use: being in either of two age groups—25 to 44 years and 45 to 64 years (compared with 18 to 24 years)—having a primary care physician, experiencing either one stressful life event or two or more events before the attack, and being depressed.
Only one variable—being depressed (OR=2.6, p=.032)—was significantly associated with increased postdisaster use of medications (analyses not shown).
No interaction effects were found among the key age, gender, marital status, and education groups for any of the four models.
On the basis of our earlier survey, we conducted additional analyses related to use of services among respondents with postdisaster PTSD or depression (N=277). As shown in Table 4, white respondents with PTSD or depression were more likely to have received postdisaster mental health services, as were respondents aged 25 years or older, especially those between the ages of 45 and 64 years. Furthermore, respondents with health insurance or primary care physicians were more likely to have received services.
Table 5 compares mental health service use by Manhattan residents in the survey reported here with that reported in our earlier survey (6,14). The results show a clear decrease in use over time. For example, 19.4 percent of Manhattan residents used services in the first and second month after the attack, compared with 12 percent in the fourth and fifth month. Although an increase in psychiatric medication use was noted during this time, these differences were not significant.
Discussion
The results of our study suggest that mental health service use in the community four to five months after the attack on the World Trade Center was modest. Only 7.6 percent of residents used mental health services, a slight decrease from reported use the month before the disaster (8.6 percent). Psychiatric medication use was also modest four to five months later; 7.7 percent of survey respondents reported use, a slight increase from medication use the month before the disaster (6.8 percent).
In multivariate analyses, we found that African-American and Hispanic respondents were less likely than white respondents to use mental health services or psychiatric medications after the disaster. Furthermore, respondents who reported postdisaster medication use were more likely to have primary care physicians and to be between 25 and 64 years of age. Life stress in the 12 months before the attack was also associated with postdisaster service and medication use. Some respondents reported more mental health visits after the disaster than before—those with a graduate school education, those whose use of alcohol was greater after the attack, those who were depressed, and those with some involvement with the rescue efforts.
Among residents who met criteria for either PTSD or depression after the attack (N=277), African Americans and Hispanics were less likely to report mental health visits, as were respondents aged 18 to 24 years, those without health insurance, and those without a primary care physician. When mental health service use by Manhattan residents in the fourth and fifth month after the disaster was compared with use in the first two months after the disaster, a significant decrease over time was found.
As many as 41 percent of the direct survivors of the Oklahoma City bombing reported seeking professional mental health treatment in the six months after the incident (42). Only 8.5 percent of the general population of the Oklahoma City metropolitan area sought help in the three months after the bombing (8). This lower rate of help seeking is comparable to the rate we found in the fourth and fifth months after the attack in New York City. However, because no data on use of mental health services in Oklahoma City before the bombing are available, comparisons are difficult. Six months after the Newcastle earthquake in Australia, a community survey indicated that as many as 21.3 percent of adults used disaster-related support services; however, mental health services were apparently just one of the types of services included in that category (7). As these few studies suggest, because of different exposure factors, time frames, and demographic factors, as well as regional differences, it is difficult to predict population-level mental health services use, except to state that use will usually be higher than it was before the disaster but will decline over time (9,10). Many postdisaster studies have focused on use of emergency services, which further complicates the comparison with postdisaster mental health service use (9,43).
We found that race or ethnicity, exposure to lifetime traumatic events, exposure to recent stressful life events, and current depression were consistent predictors of postdisaster use of mental health services. Previous research has shown that PTSD is associated with a history of exposure to traumatic stress as well as exposure to stressful life events (18). In addition, PTSD is commonly associated with depression (44). Given the results of previous studies, our findings for race and ethnicity are not surprising (13). Studies have found racial and ethnic disparities in mental health care, including differences in access, diagnostic practices, and availability of optimal treatments (45). Although cultural factors likely played a role (46), the racial and ethnic disparities in postdisaster mental health service use that we found were surprising, because free counseling services were available in New York City after the attack (47). Not surprising, however, was the finding that persons with postdisaster PTSD or depression were less likely to receive mental health treatment if they did not have a primary care physician or health insurance coverage (13). Finally, our finding that greater use of services after the attack was associated with a reported increase in alcohol consumption warrants further investigation. Exposure to psychological trauma may put victims at risk of substance abuse, because some traumatized individuals may use alcohol or drugs to reduce psychological distress (48,49).
Our findings should be interpreted with caution. At the time of the survey, New York City was on a heightened state of alert, and residents were concerned about possible terrorist attacks. These factors may have affected service use. In addition, it is possible that residents may have temporarily left the city after September 11, although we found little evidence of this in subsequent surveys (27). We used self-reported data collected by telephone, which raises the possibility of poor respondent recall and sample selection biases, although the demographic characteristics of our sample were comparable to U.S. census estimates for New York City (41). Finally, we assessed service use during a 30-day period. The short time frame and seasonal variation may also have biased our results, although we found little evidence for this in subsequent surveys (27).
Conclusions
Despite the limitations of the study, it is one of only a few that have examined longitudinal, population-level mental health service use in the community after a catastrophic event. Although use was not as high as expected (50) and appeared to decrease over time, the access issues suggested by our findings are worthy of investigation. In particular, we found that African Americans, Hispanics, respondents aged 18 to 24 years, and respondents without health insurance or a primary care physician were less like to have received postdisaster mental health care for some reason, despite the availability of free counseling services. In addition, how New Yorkers fare over time is also an important area of investigation. We plan to study these and other issues in future research.
Acknowledgments
The research was supported by grants from the United Way of New York City, the September 11th Fund of the New York Community Trust, and grant R01-DA14219-01S1 from the National Institute on Drug Abuse.
Dr. Boscarino and Dr. Adams are affiliated with the division of health and science policy of the New York Academy of Medicine, 1216 Fifth Avenue, DHSP Room 552, New York, New York 10029 (e-mail, [email protected]). Dr. Boscarino is also with the research service of the Department of Veterans Affairs in East Orange, New Jersey. Dr. Galea, Ms. Ahern, and Dr. Vlahov are with the Center for Urban Epidemiologic Studies at the New York Academy of Medicine. Dr. Galea is also with the department of epidemiology at Columbia University in New York. Dr. Vlahov is also with the School of Public Health at Johns Hopkins University in Baltimore. Dr. Resnick is with the National Crime Victims' Center at the Medical University of South Carolina in Charleston.
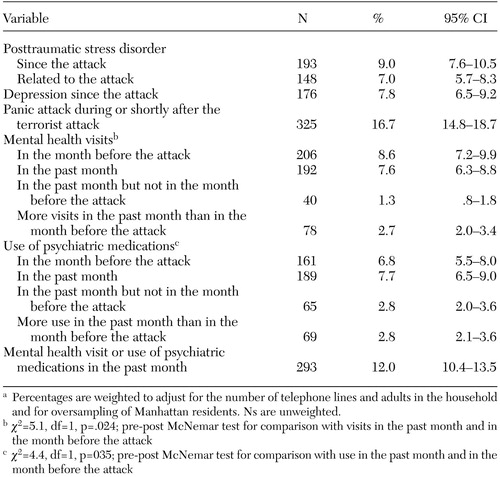 |
Table 1. Psychiatric disorders and use of mental health services and psychiatric medications reported by respondents to a survey conducted in New York City four to five months after the attack on the World Trade Centera
a Percentages are weighted to adjust for the number of telephone lines and adults in the household and for oversampling of Manhattan residents. Ns are unweighted.
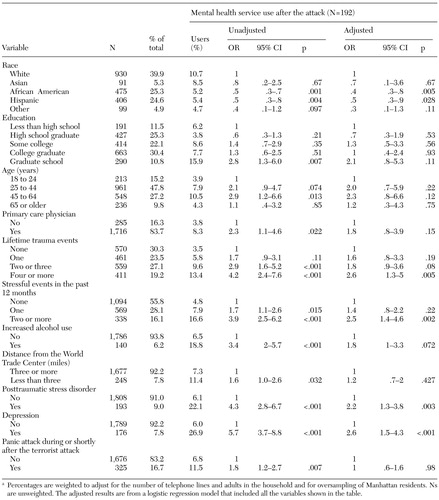 |
Table 2. Results of multivariate analyses of predictors of use of mental health services by respondents to a survey conducted in NewYork City four to five months after the attack on the World Trade Centera
a Percentages are weighted to adjust for the number of telephone lines and adults in the household and for oversampling of Manhattan residents. Ns are unweighted. The adjusted results are from a logistic regression model that included all the variables shown in the table.
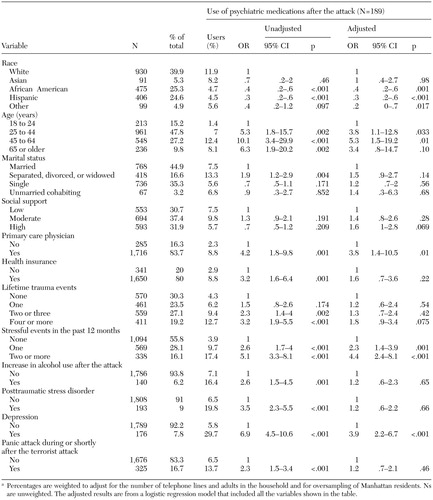 |
Table 3. Results of multivariate analyses of predictors of use of psychiatric medications by respondents to a survey conducted in New York City four to five months after the attack on the World Trade Centera
a Percentages are weighted to adjust for the number of telephone lines and adults in the household and for oversampling of Manhattan residents. Ns are unweighted. The adjusted results are from a logistic regression model that included all the variables shown in the table.
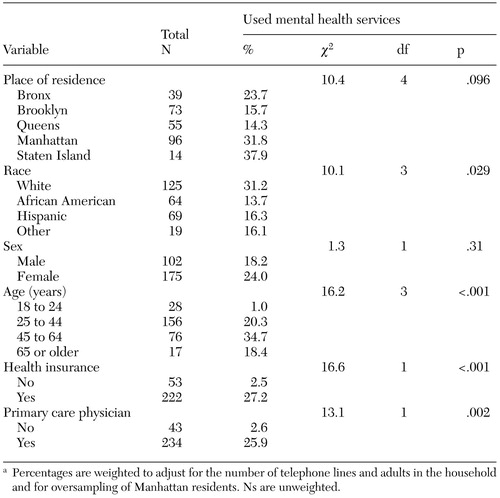 |
Table 4. Mental health service use among respondents in New York City who had posttraumatic stress disorder (PTSD) or depression when they were surveyed four to five months after the attack on the World Trade Center (N=277)a
a Percentages are weighted to adjust for the number of telephone lines and adults in the household and for oversampling of Manhattan residents. Ns are unweighted.
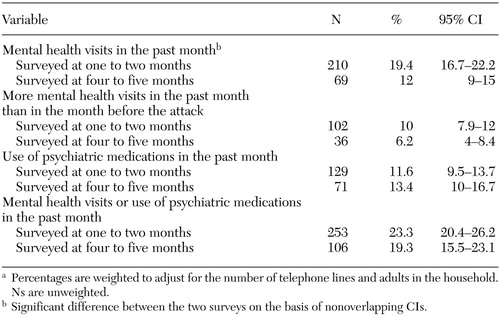 |
Table 5. Use of mental health services after the attack on the World Trade Center by respondents in two Manhattan surveys, one conducted one to two months after the attack (N=988) and another conducted four to five months after (N=506)a
a Percentages are weighted to adjust for the number of telephone lines and adults in the household. Ns are unweighted.
1. Green BL: Evaluating the effects of disasters. Psychological Assessment 3:538–546, 1991Crossref, Google Scholar
2. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology 60:409–418, 1992Crossref, Medline, Google Scholar
3. Smith EM, North CS, McCool RE, et al: Acute post-disaster psychiatric disorders: identification of persons at risk. American Journal of Psychiatry 147:202–206, 1990Link, Google Scholar
4. Rubonis AV, Bickman L: Psychological impairment in the wake of disaster: the disaster-psychopathology relationship. Psychology Bulletin 109:384–399, 1991Crossref, Medline, Google Scholar
5. McFarlane AC: The aetiology of post-traumatic morbidity: predisposing, precipitating, and perpetuating factors. British Journal of Psychiatry 154:221–228, 1989Crossref, Medline, Google Scholar
6. Galea S, Ahern J, Resnick H, et al: Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine 346:982–987, 2002Crossref, Medline, Google Scholar
7. Carr VJ, Lewin TJ, Carter GL, et al: Patterns of service utilization following the 1989 Newcastle earthquake: findings from phase 1 of the quake impact. Australian Journal of Public Health 16:360–369, 1992Crossref, Medline, Google Scholar
8. Smith DW, Christiansen EH, Vincent R, et al: Population effects of the bombing of Oklahoma City. Journal of the Oklahoma State Medical Association 92:193–198, 1999Medline, Google Scholar
9. Burkle FM: Acute-phase mental health consequences of disasters: implications for triage and emergency medical services. Annals of Emergency Medicine 28:119–128, 1996Crossref, Medline, Google Scholar
10. Gleser GC, Green BL, Winget C: Prolonged psychosocial effects of disaster: a study of Buffalo Creek. New York, Academic Press, 1981Google Scholar
11. Joseph S, Yule W, Williams R, et al: Increased substance use in survivors of the Herald of Free Enterprise disaster. British Journal of Medical Psychology 66:185–191, 1993Crossref, Medline, Google Scholar
12. Madakasira S, O'Brien KF: Acute posttraumatic stress disorder in victims of a natural disaster. Journal of Nervous and Mental Disease 175:286–290, 1987Crossref, Medline, Google Scholar
13. Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, 1999Google Scholar
14. Galea S, Boscarino J, Resnick H, et al: Mental health in New York City after the September 11 terrorist attacks: results from two population surveys, in Mental Health, United States, 2001. Edited by Manderscheid RW, Henderson MJ. Rockville, Md, Center for Mental Health Services, 2003Google Scholar
15. Boscarino JA, Galea S, Ahern J, et al: Utilization of mental health services following the September 11th terrorist attacks in Manhattan, New York City. International Journal of Emergency Mental Health 4:143–155, 2002Medline, Google Scholar
16. Boscarino JA, Galea S, Ahern J, et al: Psychiatric medication use among Manhattan residents following the World Trade Center disaster. Journal of Traumatic Stress 16:301–306, 2003Crossref, Medline, Google Scholar
17. Standard Definitions: Final Dispositions of Case Codes and Outcomes Rates for Surveys. Ann Arbor, Mich, American Association for Public Opinion Research, 2000Google Scholar
18. Freedy JR, Kilpatrick DG, Resnick HS: Natural disasters and mental health: theory, assessment, and intervention. Journal of Social Behavior and Personality (special issue) 8:49–103, 1993Google Scholar
19. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8–19, 1994Crossref, Medline, Google Scholar
20. Kessler RC, Zhao S, Katz SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156:115–123, 1999Link, Google Scholar
21. Stamm BH: Contextualizing death and trauma: a preliminary endeavor, in Death and Trauma. Edited by Figley CR. New York, Brunner/Mazel, 1996Google Scholar
22. Resnick HS, Kilpatrick DG, Dansky BS, et al: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology 61:984–991, 1993Crossref, Medline, Google Scholar
23. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
24. Kilpatrick DG, Resnick HS, Freedy JR, et al: The posttraumatic stress disorder field trial: evaluation of the PTSD construct: criteria A through E, in DSM-IV Sourcebook, vol 4. Edited by Widiger T, Frances A, Pincus A, et al. Washington, DC, American Psychiatric Press, 1998Google Scholar
25. Spitzer RL, Williams JB, Gibbon M: Structured Clinical Interview for DSM-III-R, Non-patient Version. New York, New York State Psychiatric Institute, Biometrics Research Department, 1987Google Scholar
26. Acierno R, Kilpatrick DG, Resnick H, et al: Assault, PTSD, family substance use, and depression as risk factors for cigarette use in youth: findings from the National Survey of Adolescents. Journal of Traumatic Stress 13:381–396, 2000Crossref, Medline, Google Scholar
27. Boscarino JA, Adams RE: Mental health treatment in New York City 1 year after the terrorist attacks. Presented at the annual meeting of AcademyHealth, Nashville, June 26–29, 2003Google Scholar
28. Galea S, Vlahov D, Resnick H, et al: Trends in probable posttraumatic stress in New York City after the September 11 terrorist attacks. American Journal of Epidemiology 158:514–524, 2003Crossref, Medline, Google Scholar
29. Blanchard EB, Jones-Alexander J, Buckley TC, et al: Psychometric properties of the PTSD checklist. Behavioral Research and Therapy 34:669–673, 1996Crossref, Medline, Google Scholar
30. Galea S, Vlahov D. Mental health in the New York City metropolitan area after the September 11 attacks: research of the New York Academy of Medicine, in The Social, Psychological, and Political Impact of the September 11th Terrorist Attacks on the American Public. Edited by Smith T. New York, Russell Sage, 2004Google Scholar
31. Pepe MS: The Statistical Evaluation of Medical Tests for Classifacation and Prediction. Oxford, England, Oxford University Press, 2003Google Scholar
32. Blascovich J, Tomaka J: Measure of self-esteem, in Measures of Personality and Social Psychological Attitudes. Edited by Robinson JP, Shaver PR, Wrightsman LS. New York, Academic Press, 1991Google Scholar
33. Ware JE, Kosinski M, Tuner-Bowker DM, et al: Version 2 of the SF-12 Health Survey. Boston, Quality Metric Inc, 2002Google Scholar
34. Derogatis LR: Brief Symptom Inventory 18 (BSI-18) Manual. Minnetonka, Minn, NCS Assessments, 2001Google Scholar
35. Kilpatrick DG, Ruggiero, KJ Acierno, R, et al: Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the national survey of adolescents. Journal of Consulting and Clinical Psychology 71:692–700, 2003Crossref, Medline, Google Scholar
36. Robins LN, Cottler LB, Bucholz KK, et al: Diagnostic Interview Schedule for DSM-IV (revised Jan 9, 2002). St Louis, Washington University School of Medicine, Department of Psychiatry, 1999Google Scholar
37. Bromet E, Sonnega A, Kessler RC: Risk factors for DSM-III-R posttraumatic stress disorder: findings from the National Comorbidity Survey. American Journal of Epidemiology 147:353–361, 1998Crossref, Medline, Google Scholar
38. Kulka RA, Schlenger WE, Fairbank JA, et al: Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
39. STATA, version 7.0. College Station, Tex, Stata Corp, 2001Google Scholar
40. Boscarino JA, Galea S, Ahern J, et al: Access to psychiatric services in New York City following the September 11th terrorist attacks. Annals of Epidemiology 12:514, 2002Crossref, Google Scholar
41. Census summary tape, file 3A (STF3A). Washington, DC, Bureau of the Census, 2000Google Scholar
42. North CS, Nixon SJ, Shariat S, et al: Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA 282:755–762, 1999Crossref, Medline, Google Scholar
43. Gerrity ET, Flynn BW: Mental health consequences of disasters, in The Public Health Consequences of Disasters, Edited by Noji EK. New York, Oxford University Press, 1997Google Scholar
44. Kessler RC, Sonnega A, Bromet E, et al: Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 52:1048–1060, 1995Crossref, Medline, Google Scholar
45. Snowden LR: Bias in Mental health assessment and intervention: theory and evidence. American Journal of Public Health 93:239–243, 2003Crossref, Medline, Google Scholar
46. Cauce AM, Domenech-Rodriguez M, Paradise M, et al: Cultural and contextual influences in mental health help seeking: a focus on ethnic minority youth. Journal of Consulting and Clinical Psychology 70:44–55, 2002Crossref, Medline, Google Scholar
47. Quervalu I: Project Liberty New York City. New York, New York City Department of Mental Health, Mental Retardation, and Alcoholism, 2002Google Scholar
48. Ouimette P, Brown PJ (eds): Trauma and Substance Abuse: Causes, Consequences of Comorbid Disorders. Washington, DC, American Psychological Publishing, 2003Google Scholar
49. Boscarino J: Current excessive drinking among Vietnam veterans: a comparison with other veterans and non-veterans. International Journal of Social Psychiatry 27:204–222, 1981Crossref, Medline, Google Scholar
50. Mental illness crisis fails to materialize. Psychiatric News 37(17):23, 2002Google Scholar



