Variables Associated With Hospitalization Decisions by Emergency Psychiatrists After a Patient's Suicide Attempt
Abstract
OBJECTIVE: This study explored the factors psychiatrists considered in deciding on hospitalization for a large sample of suicide attempters in the emergency department of a general hospital in Madrid, Spain, between 1996 and 1998. METHODS: Psychiatrists assessed 509 patients who had attempted suicide; 196 of these (39 percent) were hospitalized in the psychiatric unit, and 313 (61 percent) were discharged from the emergency department. The assessment included Beck's Suicidal Intent Scale (SIS) and a checklist of 47 clinical variables. RESULTS: Of the 32 clinical variables significantly associated with hospitalization that were introduced in a logistic regression model, 11 remained significant. Six variables were associated with an increased odds of hospitalization: intention to repeat the attempt, plan to use a lethal method, low psychosocial functioning before the suicide attempt, previous psychiatric hospitalization, a suicide attempt in the past year, and planning that nobody would try to save their life after they had attempted suicide. Five variables decreased the odds: a realistic perspective on the future after the attempt, relief that the attempt was not effective, availability of a method to kill oneself (that was not used), belief that the attempt would influence others, and family support. Models based on the SIS total score and individual SIS items had lower specificity and sensitivity. CONCLUSIONS: Psychiatrists appear to rely on patients' self-report in deciding on hospitalization rather than focus on demographic, diagnostic, or psychosocial issues. If the findings of this study were replicated in other hospital settings, the implication would be that the guidelines for assessing suicide attempts need to encourage thorough and detailed assessment of the attempt and the future plans.
Suicide attempts are the best predictors of an eventual completed suicide (1). They are associated with significant morbidity and result in significant use of health care resources. A survey carried out from 1990 to 1992 indicated that 4.6 percent of persons in the U.S. population acknowledged making a suicide attempt during their lifetime (2). The Centers for Disease Control and Prevention estimated that 67.5 individuals per 100,000 were treated in emergency departments for probable or possible suicide attempts in a six-month period in 2000 (3). The annual cost of suicide attempts in the United States is estimated to be $111 billion (4). For every completed suicide there are five estimated hospitalizations and 22 emergency department visits related to a suicide attempt (5).
Thus assessment and treatment of suicidal behavior in emergency departments is a key factor in treating suicide attempts and preventing suicide. One objective of the U.S. National Strategy for Suicidal Prevention was to develop suicide risk assessment guidelines in the emergency departments (5), where records are poor in quality (6,7,8,9,10,11).
Several guidelines for suicide assessment have recently been designed (12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31), but none are universally accepted. Hospitalization is recommended when there is an imminent risk of suicide—for example, when the patient has expressed an intent to die, has a plan in mind, has lethal means available, and evidences a psychiatric disorder.
The goal of the study reported here was to determine which variables (from an extensive list of clinical variables and a suicide scale) predicted psychiatrists' decisions to hospitalize a patient in a large sample of suicide attempters who were assessed in the emergency department of a general hospital covering emergencies from a catchment area of 500,000 people.
Methods
The hospital in which the study was conducted is a general hospital within the Spanish National Health System that provides medical coverage for all emergencies in a catchment area covering a population of 500,000 people in Madrid. Suicide attempts were defined according to the definition of the National Institute of Mental Health (32). The study sample, recruited into the study between 1996 and 1998, comprised 539 persons over the age of 18 years who had attempted suicide. The mean±SD age of the participants was 35.9±14.4 years.
On the basis of six years of patient recruitment (33), including consecutive recruitment in the final two years (34), it is estimated that approximately 300 different persons who have attempted suicide are seen at the hospital every year. Approximately 84 percent of those patients consent to take part in our studies. Those who consent to participate do not appear to be demographically different from those who do not. We estimate that approximately 250 suicide attempters consent to participate each year. The sample of 539 suicide attempts for the study reported here represented more than two thirds (72 percent) of the 756 persons who had attempted suicide, which represents all persons expected to consent over a three-year period. After the study was described in detail to the participants, written informed consent was obtained.
Predictor variables
Clinicians (on-call psychiatry residents) who saw patients in the emergency department carried out assessments and were responsible for deciding on hospitalization. The structured assessment included clinical variables and a suicide scale, which were analyzed separately. The clinical variables were chosen to reflect the standard procedures used by a thorough psychiatric clinician. The suicide scale reflects standardized assessment by a psychiatric researcher.
The extensive list of clinical variables was developed after review of the literature on suicide assessment. The goal of this assessment was to determine which variables obtained from the literature could help a clinical psychiatrist determine when to hospitalize a patient. The 47 variables took the form of a checklist completed by the resident during the patient interview. In addition, DSM-IV clinical diagnoses were taken from the charts. The residents made the diagnoses, supervised by the attending psychiatrists.
Beck's Suicidal Intent Scale (SIS) (35) has shown good reliability when used by suicide researchers (36). The main 15 items, scored on a scale of 0 to 2, are included in the total score. The goal of this assessment was to determine which of these 15 SIS items can help a research psychiatrist predict which patients will be hospitalized. All ratings were completed by psychiatry residents, who were trained and supervised during the first three interviews. Consensus meetings were held every month throughout the study.
Hospitalization
Determining treatment for patients who have attempted suicide in this hospital's emergency department is a complex process—as with any other clinical decisions in any emergency department—and is based on the treating physicians' clinical judgment. First, the internal medicine on-call residents decide whether hospitalization in the medical unit is required. A psychiatric assessment then takes place when the patient can collaborate with the interview. If the patient does not require a medical admission, the psychiatry resident (with the backup of an attending psychiatrist) decides on the need for psychiatric hospitalization. Thus the psychiatrists decide about discharge from the emergency department and subsequent required treatment.
The outcome was dichotomized: hospitalization or discharge from the emergency department. Of 539 persons who attempted suicide, 30 who were initially hospitalized in medical units before psychiatrists became involved were excluded from the study. The resulting sample of 509 patients included 196 (39 percent) who were hospitalized in the psychiatric unit and 313 (61 percent) who were discharged from the emergency department. The follow-up after discharge involved 200 patients (37 percent) for whom psychiatric follow-up was recommended and 113 (19 percent) who were referred to their family physicians.
Statistical analyses
The statistical analyses were conducted in two steps: univariate analyses followed by a multivariate analysis using logistic regression (37). In the univariate analyses, odds ratios (ORs) and 95 percent confidence intervals (CIs) were calculated with a dichotomous dependent variable (discharge versus hospitalization). Significance was assessed with chi square tests. The significant independent variables were then selected and introduced in logistic regression analyses with discharge versus hospitalization as the dependent variable. The Hosmer-Lemeshow goodness-of-fit test was also used.
The clinical variables were introduced as independent variables in the univariate analyses, and significant variables were then introduced into a logistic regression model. This analysis was designed to determine which variables could help clinical psychiatrists determine when patients would be hospitalized. Similarly, the SIS items were introduced as independent variables in the univariate analyses after being dichotomized in terms of presence of a high score (a score of 2 indicating present and a score of 1 or 0 indicating absent). SIS items that were significant in the univariate analyses were then introduced into a logistic regression model. This analysis was designed to determine which SIS items could help research psychiatrists determine when patients will be hospitalized.
The better cutoff point for SIS total score (sum of 15 items) to predict hospitalization was calculated by using receiver operating characteristic (ROC) analysis (38). The ROC used the total SIS score to predict hospitalization, and the logistic regression used the individual SIS items.
Results
Demographic and clinical characteristics of the study sample are listed in Table 1.
Clinical variables
Of the 47 demographic and clinical variables, 32 were significantly associated with hospitalization. When these significant variables were introduced into the logistic regression, 11 variables remained significant, as can be seen in Table 2. Six variables were associated with increased odds of hospitalization: intent to repeat the attempt, plan to use a lethal method, low psychosocial functioning before the attempt, previous psychiatric hospitalization, suicide attempt in the past year, and planning that nobody would try to save their life after they had attempted suicide. Five variables were associated with decreased odds of hospitalization (or increased odds of discharge): a realistic perspective on the future after the attempt, relief that the suicide attempt was not effective, availability of a method to kill oneself (that was not used), belief that the attempt would influence others, and family support.
A high score on 15 of the 20 SIS items was associated with hospitalization as opposed to discharge. When introduced into the logistic regression, eight items remained significant: attitude toward living and dying, number of previous attempts, conception of medical rescuability, reaction to the attempt, degree of premeditation, conception of the method's lethality, final acts in anticipation of death, and not acting to get help (Table 3).
A total score of 11 or higher best balanced sensitivity (69 percent) and specificity (70 percent) to predict hospitalization. When this cutoff score was used, 72 percent of the participants were properly classified.
Discussion
Clinical variables
As in all hospitals, the way in which hospitalization is decided upon after a suicide attempt is probably a somewhat arbitrary and complex process that considers the patient's global presentation. When this process was assessed specifically and indirectly by logistically regressing a long list of clinical variables, the intent to repeat the suicide attempt was clearly the best unique predictor. In the univariate analysis, the intent to repeat the attempt stood out as an excellent predictor, with 92 percent specificity. This sample of 509 patients who were assessed by a psychiatrist included 141 who had attempted suicide and who verbalized planning a subsequent attempt; most of these individuals (117, or 83 percent) were hospitalized. However, the intent to repeat the attempt had a relatively low sensitivity (63 percent). In the logistic model (Table 2), other characteristics of making or planning an attempt were associated with increased odds of hospitalization: plan to use a lethal method, low psychosocial functioning before the attempt, previous psychiatric hospitalization, a suicide attempt in the past year, and planning that nobody would try to save their life after they had attempted suicide. Other variables were associated with decreased odds: a realistic perspective on the future after the attempt, relief that the suicide attempt was not effective, availability of a method to kill oneself, belief that the attempt would influence others, and family support. Surprisingly, only three demographic or clinical variables that were associated with the attempt also predicted hospitalization; these were low psychosocial functioning before the attempt, previous psychiatric hospitalization, and suicide attempt in the past year.
Although depression alone was not associated with hospitalization, psychiatrists appeared to consider depression in assessing patients who had attempted suicide. The variables associated with hospitalization were not the same for depressed patients as for those who were not depressed, which was obvious when four independent logistic regressions—of male gender, female gender, depression, and absence of depression—were conducted. Intent to repeat the attempt was a good predictor of hospitalization in the four groups. The use of a lethal method was a significant predictor in the regression of male gender. In the other subgroups (women, patients with depression, and patients without depression), which had low percentages of patients who had used lethal methods, plan to use a lethal method was a significant predictor. Previous psychiatric hospitalization was a predictor among female patients and patients without depression. After other variables in the logistic regression were controlled for, poor past psychosocial functioning predicted hospitalization only among patients with depression.
Thus clinicians' decisions appeared to be better explained in this hospital setting by the self-report of the patient who had attempted suicide than by the typical variables included in the suicide assessment guidelines, such as history, current diagnosis, and psychosocial support. If the predictors of hospitalization were replicated in other hospital settings, one could infer that guidelines for assessing suicide attempts may need to emphasize the need for thorough and detailed assessment of the attempt and future plans, because clinicians may be using the patient's report in deciding on hospitalization rather than focusing only on demographic, diagnostic, or psychosocial factors.
Comparing clinical variables and SIS items as predictors
It was perplexing that the SIS score was not a better predictor than an extensive clinical checklist. Moreover, compared with the model that used the clinical checklist, the model that used the SIS items appeared to have lower sensitivity (85 percent compared with 89 percent) and lower specificity (59 percent compared with 75 percent) and to result in a lower percentage of patients who were correctly classified (74 percent compared with 83 percent). Use of the total SIS score did not predict hospitalization better than use of the SIS items. Nor did SIS score predict completed suicide in past studies (39,40,41). In summary, it appears that clinical assessment is a better means of determining whether a patient will be hospitalized than is a thorough assessment using a research tool.
Limitations
This study had all the limitations of any naturalistic study that lacks an experimental design. The study included a large sample—larger than those in most previous clinical suicide studies in emergency departments—but did not include all possible patients who had attempted suicide. Logically, completed suicides cannot be included in this type of study, but relatively few patients were missed. During the period 1996 to 1999, the catchment area death registry identified 32 deaths by suicide and another 23 deaths with unknown intentionality. The annual rate for suicides and accidental deaths (except traffic accidents) was 16.6 per 100,000, which is similar to the national rate in Spain (42). Thus our study included a highly representative sample of persons who had attempted suicide and who were seeking medical help in this catchment area.
Although it was assumed in this study that the clinical discharge decision was appropriate, there is certainly no absolute standard. The study hospital provides free coverage to all Spanish citizens living in the catchment area. All hospitalizations are free, being paid for by the government through taxes. Admission decisions are made solely by clinicians who have no concerns about litigation and who do not need approval from any organization or managed care company. Given that U.S. managed care systems may not provide the best treatment for suicide attempts (43), suicide guidelines developed in other clinical environments may help improve outcomes in managed care settings.
It must be remembered that individual clinicians' decisions for each patient in our sample were not studied. Statistical analyses were used to indirectly explore which variables may have been more closely related to the clinical decision. Certainly, there is no definitive proof that these variables really supported the individual clinical decisions.
New additions to the literature
No other published studies have used extensive assessments of characteristics of a suicide attempt to determine variables associated with hospitalization. An almost 30-year-old U.S. study (44) used expert criteria to compare hospitalization decisions for 248 persons who had attempted suicide. Although, according to the criteria, all 248 persons should have been hospitalized, the clinicians discharged 127 (51 percent). Stern and colleagues (45) studied 177 consecutive patients in a U.S. hospital who had overdosed; 47 percent of the patients were hospitalized. Owens and colleagues (46) studied 1,096 patients in the emergency department of a British hospital who had attempted self-poisoning. The proportion of patients hospitalized was 69 percent. The clinical variables associated with hospitalization were older age, worse physical health, expressing a threat or leaving a note, and previous psychiatric hospitalization. Detailed clinical or research assessment of characteristics of the suicide attempt was not performed.
The results of our study provide several new additions to the literature—specifically, the fact that characteristics of the clinical assessment were better predictors of hospitalization than were the SIS items or the total SIS score. Clinicians—at least at this hospital—may be paying more attention to some specific characteristics of the suicide attempt than to demographic factors when deciding on hospitalization. Thus the guidelines for assessing suicide attempts may need to emphasize the need for thorough and detailed assessment of the attempt and future plans, because clinicians may be using patients' self-reports in deciding on hospitalization rather than focusing only on demographic, diagnostic, or psychosocial factors.
Conclusions
Further studies are needed to determine whether the variables we describe or other variables are good predictors of hospitalization in other hospital settings. More important, prospective studies in emergency departments are needed to determine which characteristics of the emergency department best predict whether a person treated for attempted suicide will commit suicide several years later. In this type of prospective study, which recruits suicide attempters at the emergency department, it may be important to distinguish long-term predictors of completed suicide among patients in the emergency department who are discharged from such predictors among hospitalized patients. It is hoped that hospitalization may alter the prognosis of the patients who participated in this study and may benefit some of them, even though a priori, persons who are hospitalized are likely to have a worse prognosis than those who are discharged from the emergency department (46).
Acknowledgments
This study was conducted at the Hospital Ramon y Cajal in Madrid, Spain. The study was supported by two awards from the National Alliance for Research on Schizophrenia and Depression to Dr. Baca-Garcia and by a grant from the Spanish Government (Fondo de Investigacion Sanitaria, FIS 01/0077-01).
Dr. Baca-García is affiliated with the department of psychiatry of Fundacion Jimenz Diaz in Madrid, Spain. Dr. Diaz-Sastre, Dr. García Resa, Dr. Blasco, Dr. Braqehais Conesa, and Dr. Saiz-Ruiz are with the department of psychiatry of Hospital Ramon y Cajal, Universidad de Alcalá in Madrid. Dr. de Leon is affiliated with the Mental Health Research Center at Eastern State Hospital in Lexington, Kentucky. Send correspondence to him at 627 West Fourth Street, Lexington, Kentucky 40508 (e-mail, [email protected]). An earlier version of this paper was presented as a poster at the annual meeting of the American Psychiatric Association held May 18 to 23, 2002, in Philadelphia.
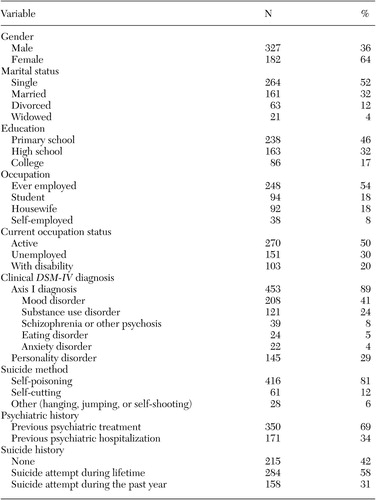 |
Table 1. Demographic and clinical characteristics of a sample of 509 patients assessed by a psychiatrist after a suicide attempt
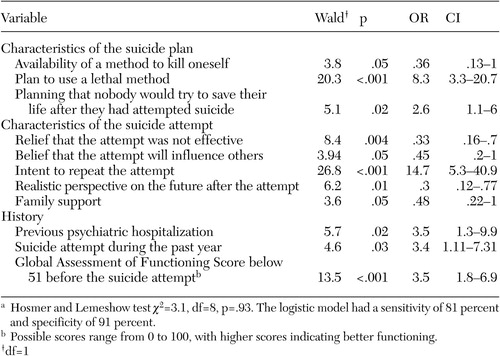 |
Table 2. Significant clinical variables in a logistic regression to predict psychiatric hospitalizationin a sample of 509 patients who had attempted suicidea
a Hosmer and Lemeshow test χ2=3.1, df=8, p=.93. The logistic model had a sensitivity of 81 percent and specificity of 91 percent.
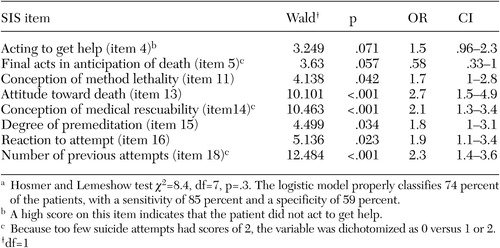 |
Table 3. Significant high scores on items of Beck's Suicidal Intent Scale (SIS) in a logisticregression to predict psychiatric hospitalization in a sample of 509 patients whohad attempted suicidea
a Hosmer and Lemeshow test χ2=8.4, df=7, p=.3. The logistic model properly classifies 74 percent of the patients, with a sensitivity of 85 percent and a specificity of 59 percent.
1. Harris C, Barraclough B: Suicide as an outcome for mental disorders. British Journal of Psychiatry 170:205–228, 1997Crossref, Medline, Google Scholar
2. Kessler RC, Borges G, Walters EE: Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry 56:617–626, 1999Crossref, Medline, Google Scholar
3. Center for Diseases Control and Prevention: Nonfatal self-inflicted injuries treated in hospital emergency departments: United States, 2000. Morbidity and Mortality Weekly Report 51:436–438, 2002Medline, Google Scholar
4. Kashner TM, Shoaf T, Rush AJ: The economic burden of suicide in the United States in the year 2000. The Economics of Neuroscience 2:44–48, 2000Google Scholar
5. US Public Health Service: National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC, US Department of Health and Human Services, 2001Google Scholar
6. Suokas J, Lonnqvist J: Suicide attempts in which alcohol is involved: a special group in general hospital emergency rooms. Acta Psychiatrica Scandinavica 91:36–40, 1995Crossref, Medline, Google Scholar
7. Black D, Creed F: Assessment of self-poisoning patients by psychiatrists and junior medical staff. Journal of the Royal Society of Medicine 81:97–99, 1988Crossref, Medline, Google Scholar
8. O'Dwyer FG, D'Alton A, Pearce JB: Adolescent self-harm patients: audit of assessment in an accident and emergency department. British Medical Journal 303:629–630, 1991Crossref, Medline, Google Scholar
9. Shepherd RM, Dent TH, Alexander GJ, et al: Prevalence of alcohol histories in medical and nursing notes of patients admitted with self poisoning. British Medical Journal 311:847, 1995Crossref, Medline, Google Scholar
10. Ebbage J, Farr C, Skinner DV, et al: The psychosocial assessment of patients discharged from accident and emergency departments after deliberate self-poisoning. Journal of the Royal Society of Medicine 87:515–516, 1994Medline, Google Scholar
11. Malone KM, Szanto K, Corbitt E, et al: Clinical assessment versus research methods in the assessment of suicidal behavior. American Journal of Psychiatry 152:1601–1607, 1995Link, Google Scholar
12. The General Hospital Management of Adult Deliberate Self-Harm: A Consensus Statement on Standards for Service Provision. London, England, Royal College of Psychiatrists, 1992Google Scholar
13. Gunnell D, Frankel S: Prevention of suicide: aspirations and evidence. British Medical Journal 308:1227–1233, 1994Crossref, Medline, Google Scholar
14. Kachur P, DiGuiseppi C: Screening for Suicide Risk: Guide to Clinical Preventive Services, 2nd ed. Washington, DC, US Department of Health and Human Services, Office of Disease Prevention and Health Promotion, 1996. Available at http://cpmcnet.columbia.edu/texts/gcps/gcps0060.htmlGoogle Scholar
15. McNamee JE, Offord DR: Prevention of suicide, in Canadian Task Force on the Periodic Health Examination: Canadian Guide to Clinical Preventive Health Care. Ottawa, Health Canada, 1994. Available at www.ctfphc.org/tables/ch40tab.htmGoogle Scholar
16. Suicide Risk Advisory Committee of the Risk Management Foundation of the Harvard Medical Institutions: Guidelines for Identification, Assessment, and Treatment Planning for Suicidality. Available at www.rmf.harvard.edu/index.htmlGoogle Scholar
17. NHS Center for Reviews and Dissemination, University of York: Deliberate self-harm decision makers. Effective Health Care 4:1–12, 1998Google Scholar
18. Hider P: Youth suicide prevention by primary healthcare professionals: a critical appraisal of the literature. New Zealand Health Technology Assessment Report 4. 1998. Available at http://nzhta.chmeds.ac.nzGoogle Scholar
19. Royal New Zealand College of General Practitioners: Guidelines for Primary Care Providers Detection and Management of Young People at Risk of Suicide. 1998. Available at www.rnzcgp.org.nz/guidelines/ysGoogle Scholar
20. Gliatto MF, Rai AK: Evaluation and treatment of patients with suicidal ideation. American Family Physician 59:1500–1506, 1999Medline, Google Scholar
21. Hirschfeld RMA: Algorithm for the evaluation and treatment of suicidal patients. Primary Psychiatry 3:26–29, 1996Google Scholar
22. Hirschfeld RMA, Russell JM: Assessment and treatment of suicidal patients. New England Journal of Medicine 337:910–915, 1997Crossref, Medline, Google Scholar
23. Hirschfeld RMA: The suicidal patient. Hospital Practice 33:119–123,127,128,131–133, 1998Crossref, Google Scholar
24. Evidence Based Medicine Guidelines: Suicide: 2000. Available at http://195.236.0.10Google Scholar
25. Hamilton NG: Suicide prevention in primary care: careful questioning, prompt treatment can save lives. Postgraduate Medicine 108:81–87, 2000Crossref, Medline, Google Scholar
26. Preventing Suicide: A Resource for General Physicians. Geneva, World Health Organization, 2000Google Scholar
27. Magellan Behavioral Health Clinical Practice Guideline: Clinical Practice Guideline for Assessing and Managing the Suicidal Patient. Available at www.magellanprovider.com/handbook/clinprac.asp, 2000Google Scholar
28. Isacsson G,Rich CL: Management of patients who deliberately harm themselves. British Medical Journal 322:213–215, 2001Crossref, Medline, Google Scholar
29. Nicholas LM, Golden RN: Managing the Suicidal Patient. Clinical Cornerstone 3:47–57, 2001. Available at www.medscape.com/excerptamed/clincornerstne/2001/v03.n03/clc0303.07.nich/clc0303.07.nich-01.htmlGoogle Scholar
30. Shaffer D, Pfeffer CR: Practice parameters for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child and Adolescent Psychiatry 40:S24-S51, 2001Google Scholar
31. Rihmer Z, Belsö N, Kiss K: Strategies for suicide prevention. Current Opinion in Psychiatry 15:83–87, 2002Crossref, Google Scholar
32. O'Carroll PW, Berman AL, Maris RW, et al: Beyond the Tower of Babel: a nomenclature for suicidology. Suicide and Life Threatening Behaviors 26:227–235, 1996Google Scholar
33. Baca-García E, Diaz-Sastre E, Basurte E, et al: A prospective study of the paradoxical relationship between impulsivity and lethality of suicide attempts. Journal of Clinical Psychiatry 62:560–564, 2001Crossref, Medline, Google Scholar
34. Baca-García E, Vaquera C, Diaz-Sastre C, et al: A gender-specific association between the serotonin transporter gene and suicide attempts. Neuropsychopharmacology 26:692–695, 2002Crossref, Medline, Google Scholar
35. Beck AT, Schuyler D, Herman I: Development of suicidal intent scales, in Prediction of Suicide. Edited by Beck AT. Philadelphia, Charles, 1974Google Scholar
36. Mieczkowski TA, Sweeney JA, Haas GL, et al: Factor composition of the Suicide Intent Scale. Suicide and Life Threatening Behaviors 23:37–45, 1993Medline, Google Scholar
37. SPSS Advanced Statistics 7.5. Chicago, SPSS Inc, 1997Google Scholar
38. Greiner M, Pfeiffer D, Smith RD: Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Preventive Veterinary Medicine 45:23–41, 2000Crossref, Medline, Google Scholar
39. Beck AT, Steer RA: Clinical predictors of eventual suicide: a five to ten year prospective study of suicide attempters. Journal of Affective Disorders 17:203–209, 1989Crossref, Medline, Google Scholar
40. Tejedor MC, Diaz A, Castillon JJ, et al: Attempted suicide: repetition and survival: findings of a follow-up study. Acta Psychiatrica Scandinavica 100:205–211, 1999Crossref, Medline, Google Scholar
41. Beck RW, Morris JA, Beck TA: Cross-validation of the Suicide Intent Scale. Psychological Report 34:445–446, 1974Crossref, Medline, Google Scholar
42. Martinez de Aragon MV, Llacer A: Mortalidad en España. Boletin Epidemiologico Semanal 8:253–264, 2000Google Scholar
43. Ellison JM, ed: Treatment of Suicidal Patients in Managed Care. Washington, DC, American Psychiatric Press, 2000Google Scholar
44. Kirstein L, Prusoff B, Weissman M, et al: Utilization review of treatment of suicide attempters. American Journal of Psychiatry 132:22–27, 1975Link, Google Scholar
45. Stern TA, Gross PL, Pollack MH, et al: Drug overdose seen in the emergency department: assessment, disposition, and follow-up. Annals of Clinical Psychiatry 3:223–231, 1991Crossref, Google Scholar
46. Owens D, Dennis M, Jones S, et al: Self-poisoning patients discharged from accident and emergency: risk factors and outcome. Journal of the Royal College of Physicians London 25:218–222, 1991Medline, Google Scholar



