Case-Control Study of Frequent Visitors to an Urban Psychiatric Emergency Service
Abstract
OBJECTIVE: The purpose of this study was to identify risk factors for people who use psychiatric emergency services repeatedly and to estimate their financial charges. METHODS: The authors used interviews and chart reviews to compare 74 patients who had six or more visits to an urban psychiatric emergency service in the 12 months before an index visit with 74 patients who had five or fewer visits. Multivariate logistic regression was used to identify independent risk factors. RESULTS: Independent risk factors for frequent visitors were self-reported hospitalization in the past 12 months, need for medications as the self-reported reason for seeking care, being homeless or living in an institution, and not giving the name of a friend or family member for interview. The level of burden for support of persons who were interviewed was low and did not differ between frequent and infrequent visitors. Compared with infrequent visitors, frequent visitors had greater utilization of inpatient and outpatient behavioral health services, general emergency services, and crisis residential services in the 12 months before the index visit and greater utilization of general emergency services and psychiatric emergency services in the three months after the index visit. Frequent visitors' median financial charge for those services was $16,200 greater (5.9 times greater) than that of infrequent visitors. CONCLUSIONS: Frequent visitors represent resource-poor mentally ill persons who have high levels of utilization of health care facilities besides psychiatric emergency services. Possible clinical interventions for these patients include focused medication reviews.
The psychiatric emergency service is entrusted with the dual tasks of providing crisis and frontline care (1,2). It also serves as the entry point for hospitalization. Urban psychiatric emergency services are more likely than their suburban or rural counterparts to have specialized staff and space, but they are challenged by the number of patients and their patients' lack of resources (3).
Treatment approaches have changed because of the sharp decline in hospital beds that are available for emergency patients, and patients' adherence to treatment has been undermined by high rates of homelessness, lack of family support, poverty, substance abuse, and lack of transportation. Further undermining patients' treatment adherence is the suspicion that frequently develops between patients' family members, if they are in contact with the patient, and providers (4).
Staff members' difficulty in finding ways to provide high-quality care in such resource-poor environments is compounded by the presence of patients who return repeatedly to psychiatric emergency services. Staff members may feel antagonized by these frequent visitors (5), who take up space and time needed for attending to all patients, and this antagonism may lead to poor rapport and negative expectations as well as over- and undertreatment.
Frequent visitors are estimated to account for as many as one-third of all visits to psychiatric emergency services (6). Several studies have found that risk factors for frequent visitors include higher rates of psychiatric hospitalization and lower levels of access to resources (1,7,8,9,10,11,12,13,14,15). These same studies differ, however, in their findings on whether substance abuse and psychotic disorders are risk factors. Unfortunately, the source of information in most of these studies has been medical records. Given the often strong and negative attitudes staff members have toward frequent visitors (5), data from medical records may be biased or incomplete. A study by Gilfillan and colleagues (16) supported the potential for bias. It showed that documentation, but not presence of substance abuse, differed by primary diagnosis. To our knowledge, no studies have examined patients' perspectives on seeking care at psychiatric emergency services. Interviewing patients and persons in their support system, if they have one, may help identify additional risk factors. These risk factors may suggest specific clinical interventions or system-based interventions (17). Such risk factors could include lack of a support system, limited access to outpatient care, and poor patient functioning in the areas of symptom severity, daily living skills, and social interactions as well as financial and legal problems.
Interventions based in the community care system, such as assertive community treatment (18) and crisis residential housing, require the commitment of resources and staff at the system level. To quantify the burden represented by frequent visitors beyond the percentage of psychiatric emergency service admissions attributed to them and to consider this burden from a systemwide perspective, information about the frequency of these patients' admission to all facilities in the community health care system is needed.
To identify additional risk factors and determine health care utilization from a system perspective, we conducted a case-control study of frequent visitors to a psychiatric emergency service by conducting interviews with patients and persons in their support systems and chart reviews at the psychiatric emergency service and other community health care facilities. In addition, we estimated the amount of current health care financial charges attributed to frequent visitors to the psychiatric emergency service.
Methods
Sample
Definitions of "frequent visitors" have varied from persons with two or more visits in two years (13) to those with six or more visits in six months (8). Our previous investigations found no natural break in the distribution of the number of psychiatric emergency service visits in a year (5). For this study, we were motivated by the clinical imperative imposed by the primary funding agency of reducing the number of persons who come back six or more times to the psychiatric emergency service. On the basis of that clinical mandate, we identified frequent visitors as patients with six or more psychiatric emergency service visits in the 12 months before the index visit (N=74). Control patients were defined as those with five or fewer visits in the 12 months before the index visit (N=74). To address the robustness of the findings, we defined post hoc a smaller group of control patients with only one psychiatric emergency service visit in the previous 12 months.
To avoid bias in the reason for a visit by day of the month—for example, more drug-related visits during the first week of the month (19)—we recruited patients evenly over the days of the month. The first patients discharged from both the morning and afternoon shifts for each day of the week for each week of the month—for example, the first Sunday of the first week—were approached for recruitment. This sampling strategy yielded four participants per day of the week for each week of the month. If the person had already been recruited or declined to participate, the next discharged patient with the same frequency of previous visits was recruited.
Recruitment from the evening shift was attempted, but the number of visits, which was less than half the usual number during other shifts, and the participation rates of less than 50 percent were below acceptable levels. Additional recruitment during the morning and evening shifts was equally spaced over the shifts, calendar days, and weeks.
Recruitment was initiated in June 2000 and ended in December 2000. The participation rate was 85 percent and did not differ between frequent and infrequent visitors. Patients who refused to participate were more likely to have been brought to the psychiatric emergency service under petition or certification (21 patients, or 78 percent, compared with 68 patients, or 46 percent of participating patients; χ2=9.26, df=1, p=.002).
Protocol and measures
The in-person interview occurred in a private area of the psychiatric emergency service after final disposition, regardless of whether the patient was to be admitted to an inpatient hospital, placed in a residential facility, or released to the community. The interview was developed with the active participation of the psychiatric emergency service clinical staff and focused on identifying risk factors that may suggest psychiatric emergency service or systemwide interventions.
The study was approved by Wayne State University institutional review board and the Detroit-Wayne County Mental Health Agency research committee. Full written consent was obtained for each patient before the start of the structured interview. The structured interview lasted approximately one hour and included questions on demographic characteristics, social support systems, levels of functioning, service history, and medication use; questions to elicit self-reported reasons for seeking care at the psychiatric emergency service, including both open-ended questions and questions about 23 predefined reasons; measures that evaluated the patient's comprehension and logical memory using subscales of the Weschler Adult Intelligence Scale- Third Edition (20); and a measure of the patient's symptom severity, the Behavior and Symptom Identification Scale (BASIS-32) (21).
Each patient was also asked to provide the name of and contact information for a family member or friend who knew him or her well. At the end of the interview, each patient was asked to sign a form for release of medical information, which would allow us to review his or her medical charts. Each patient received a $20 gift certificate from a nearby grocery chain for participating.
All facilities listed on the release form were contacted to obtain information on the type of service and dates of service provided to the study patients. The facilities included the most frequently used providers in the area and those specifically identified by the patients in response to structured questions on sources of care. For financial charges, we used estimates derived from average current charges for levels of care at the hospital in which the psychiatric emergency service was located. This facility was the most frequently used source of care for both groups. The charges were inclusive of facility, professional, laboratory, and medication fees. The emergency medicine fee, however, was exclusive of charges for trauma care.
The family member or friend identified by each patient was contacted by telephone. A brief telephone interview consisting of the Family Burden Interview Schedule-Short Form (22) supplemented by open-ended questions on involvement in care was attempted with the person identified by each patient. The purpose of the interview was to obtain information on support received by the patient and the extent of the burden on persons in the patient's support system. The interview was not intended to verify information received from the patient.
Setting
The study occurred at the primary psychiatric emergency service for Detroit. Although located in a hospital, the service is not part of the hospital's emergency medical department. The psychiatric emergency service has approximately 10,000 visits per year and is staffed 24 hours a day by psychiatrists, psychiatric residents, nurses, social workers, and mental health technicians, as are many academic psychiatric emergency services (23). It is located in a disadvantaged area of Detroit, the tenth largest city in the United States. Eighty-two percent of the population of Detroit is African American.
Data analysis
Bivariate analyses were conducted by using t tests and chi square tests. Factors identified in bivariate analyses as significantly different (p<.05) between groups were then entered into multivariate logistic regression models with stepwise selection. This analytical strategy identifies independent risk factors; odds ratios (ORs) were calculated to summarize the magnitude of the association. The analysis was repeated by using data for the group of patients with only one psychiatric emergency service visit in the previous 12 months.
Results
The number of visits to the psychiatric emergency service in the year before the index visit for the frequent visitors ranged from six to 99. The median number of visits was nine. The infrequent visitors, by definition, had a range of one to five visits in the year before the index visit. Forty-five percent (N=33) of the infrequent visitors had only one visit. More than 90 percent (N=132) of both groups had public insurance.
Data from medical charts indicated that the frequent visitors were more likely than the infrequent visitors to have been identified by the clinician as nonadherent with treatment (χ2=5.92, df=1, p=.02) and less likely to have been brought to the psychiatric emergency service under petition or certification (χ2=10.88, df=1, p<.001). The infrequent visitors were more likely to be admitted to an inpatient hospital (χ2=6.85, df=1, p=.009). However, no difference was found between the groups in the rate of any substance use disorder diagnosis (either primary or secondary) listed in the chart for the index visit.
Data from interviews with the patients indicated that the frequent visitors were more likely than the infrequent visitors to report that they went to the psychiatric emergency service because it is a convenient location (χ2=9.60, df=1, p=.002) where they do not need an appointment (χ2=10.19, df=1, p<.001) but can receive shelter (χ2=13.91, df=1, p<.001) and medication (χ2=5.92, df=1, p=.02) (Table 1). The frequent visitors were more likely to be homeless or to have spent time during the past year in an institution (χ2=31.10, df=2, p<.001). Although the groups did not differ in reporting any drug or alcohol consumption in the three days before admission, the frequent visitors were more likely to report drinking as opposed to taking drugs during that time (χ2=4.70, df=1, p=.03). There were no differences between the groups in the BASIS-32 scores or in the measures of logical memory or comprehension. The frequent visitors were more likely to receive Social Security Disability Income (χ2=7.11, df=1, p=.008) but less likely to have a partner provide them with money (χ2=6.98, df=1, p=.005).
The frequent visitors were more likely to report being admitted to a psychiatric hospital during the past 12 months (χ2=24.49, df=1, p<.001), visiting another psychiatric emergency service (χ2=5.34, df=1, p=.02), and being referred to a publicly funded clinic (χ2=4.89, df=1, p=.03). Although no difference between groups was found in self-reported attendance at appointments with an outpatient therapist or psychiatrist, the frequent visitors were more likely to report that they had "other things to do" (χ2=5.34, df=1, p=.02), that the psychiatrist cancelled visits (χ2=6.83, df=1, p=.009), and that they did not agree with the treatment plan (χ2=8.04, df=1, p=.005) as reasons for missing visits.
The frequent visitors were less likely to give the name of a family member or friend who knew them well (26 of the frequent visitors, or 35 percent, compared with 42 of the infrequent visitors, or 57 percent; χ2=6.96, df=1, p=.008). The groups did not differ, however, in the likelihood of contact or participation of the person once a name was provided. None of the scores on subscales of the Family Burden Interview Schedule-Short Form, including the measures of objective assistance in daily living, subjective assistance in daily living, objective supervision, subjective supervision, impact, and worry, were significantly different between the groups. Few family members or friends responded to the open-ended questions. Of those who offered responses, persons named by infrequent visitors were more likely to report speaking with psychiatric emergency service staff (eight of the persons named by frequent visitors, or 22 percent, compared with one of the persons named by infrequent visitors, or 4 percent; χ2=3.94, df=1, p<.05). Very few family members or friends of persons named by the infrequent visitors (three persons, or 8 percent) and none of the persons named by the frequent visitors mentioned providing family support to assist the patient.
Because the risk factors listed above and others identified in Table 1 may be related to each other, they were entered into a multivariate analysis to identify independent risk factors (Table 2). The independent risk factors identified in this analysis were self-reported psychiatric hospitalization in the past 12 months (OR=3.54), self-reported need for medication as the reason for seeking care (OR=2.80), homelessness (OR=7.24) or living in another nonhome environment (OR=3.84), and not giving the name of a friend or family member for interview (OR=2.40). The results of the analysis of data from the subset of patients with only one psychiatric emergency service visit in the previous year were virtually identical, except for lack of a significant between-group difference for not giving the name of a friend or family member for interview. The results of an analysis in which documented psychiatric hospitalization was substituted for self-reported psychiatric hospitalization were virtually identical to those of the original analysis, except for lack of a significant between-group difference for not giving the name of a friend or family member for interview.
Using data from the medical chart reviews, we examined health care utilization in the 12 months before the index visit and in the three months after the index visit (Table 3). In the 12 months before the index visit, frequent visitors were more likely than infrequent visitors to have any inpatient admission (χ2=12.84, df=1, p<.001), outpatient treatment (χ2=6.63, df=1, p=.01), crisis residential stay (χ2=9.98, df=1, p=.002), and emergency department visit (χ2=8.60, df=1, p=.003). In addition, in the three months after the index visit, frequent visitors were more likely to have an emergency department visit (χ2=6.46, df=1, p=.01) and a psychiatric emergency service visit (χ2=20.58, df=1, p<.001).
The frequent visitors had a median health care charge for inpatient and outpatient behavioral health services and emergency medical and emergency psychiatric services over the previous 12 months of $19,500. In contrast, the infrequent visitors had a median charge of $3,300. The excess health care charge for the frequent visitors was $16,200. Given this estimate, the health care system could receive health care charges from 5.9 infrequent visitors for each frequent visitor.
Discussion
This study found that frequent visitors to an urban psychiatric emergency service had fewer resources, such as a home and support system, than infrequent visitors. From the patients' perspective, the frequent visitors' reliance on the psychiatric emergency service was entirely rational—they valued it for its location, lack of a requirement for appointments, and provision of food, shelter, and medications. From the patient-identified support persons' perspective, frequent visitors did not pose a burden. From the health care system's perspective, frequent visitors were expensive, because one frequent visitor could incur financial charges equivalent to those for about six infrequent visitors.
The goal of the study was to suggest clinic-based or system-based interventions to address high levels of utilization of the psychiatric emergency service. Working with an existing support person would be challenging in this urban area—only 35 percent of the frequent visitors were able to give the name of a possible support person. Likewise, enhancing access to outpatient clinics does not appear promising, because the frequent visitors were more than twice as likely to have visited an outpatient clinic in the past year. The identification of the need for medication as a self-reported reason for seeking care suggests that a brief, focused intervention directed at medications for frequent visitors in the psychiatric emergency service may be useful. Rather than providing comprehensive services to all patients, it may be useful to provide some of the frequent visitors with a brief intervention focused primarily on mediation needs. This intervention would minimize the burden to the psychiatric emergency service and should result in lower financial charges to the system. Such an intervention needs to be evaluated, however, to avoid potential adverse effects on quality of care and cost offsets.
It appears that system-based interventions may be most promising in addressing patients' lack of resources and poor functioning in the area of financial matters. One such intervention, assertive community treatment (18), may be most appropriate, although recent trials with homeless individuals were not as promising as earlier implementations of assertive community treatment (24). It is noteworthy that very few patients in this study were identified by the interview or chart review as having had assertive community treatment.
The study was limited to patients who visited the psychiatric emergency service and was limited by the durations of the assessment period. The results suggest nothing about patients who do not visit the psychiatric emergency service. This group may be composed of patients who do not receive the care they need or of patients who are successful in preventing crises and/or deterioration in functioning. Inclusion of such patients in future studies would provide useful information for designing system-based interventions. Our decision to have a relatively short interview precluded an independent assessment of psychiatric diagnoses. We also did not use a drug and alcohol screen, because of concerns about reducing the level of participation (25). We focused on achieving high participation rates and were pleasantly surprised by the high level of participation. However, the patients did not seem to be motivated to answer the questions assessing cognitive functioning or to expand on their answers to open-ended questions, such as providing reasons for their lack of adherence to previous treatment plans.
Despite these limitations, the findings were much appreciated by the psychiatric emergency service clinical staff and its funding agency. The risk factors of homelessness, self-reported or documented recent hospitalization, and self-reported seeking of medications as a reason for visiting the psychiatric emergency service paint a picture of resource-poor mentally ill persons who rely on the psychiatric emergency service for support. The findings of higher use of other health care facilities reinforce the necessity for the system as a whole to address the needs of frequent visitors.
Conclusions
Given that the psychiatric emergency service is the primary entry point for inpatient and crisis residential admissions, the higher use of these services by frequent visitors makes sense. However, it is less intuitive that the frequent visitors also are highly likely to use outpatient services. Together these findings suggest that, despite receiving more services, frequent visitors to the psychiatric emergency service do not appear to have their needs met. These patients are using a disproportionate share not only of psychiatric emergency service resources but of other resources as well. It is imperative for the health care system to carefully evaluate the quality, appropriateness, and effectiveness of available services to better target the needs of frequent visitors. Frequent visitors may be better served by nontraditional services that comprehensively address needs for food and shelter as well as medication.
Acknowledgments
This work was supported by a grant from the Ethel and James Flinn Family Foundation and a grant from the state of Michigan (Joe Young, Sr.).
Dr. Arfken, Dr. Zeman, Ms. Yeager, Ms. White, and Dr. Amirsadri are affiliated with the department of psychiatry and behavioral neurosciences at Wayne State University, 2761 East Jefferson, Detroit, Michigan 48207 (e-mail, [email protected]). Dr. Arfken is also with the Center for Healthcare Effectiveness Research at Wayne State University. Mr. Mischel is with the department of emergency psychiatry at Detroit Medical Center in Detroit.
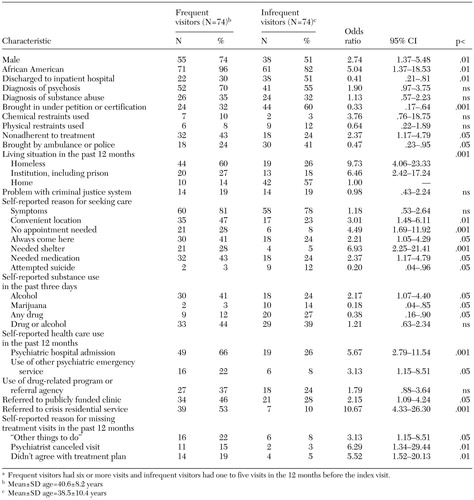 |
Table 1. Demographic and clinical characteristics of frequent and infrequent visitors to a psychiatric emergency servicea
a Frequent visitors had six or more visits and infrequent visitors had one to five visits in the 12 months before the index visit.
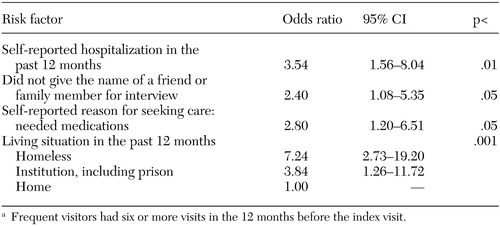 |
Table 2. Results of multivariate logistic regression analysis of independent risk factors associated with being a frequent visitor to a psychiatric emergency servicea
a Frequent visitors had six or more visits in the 12 months before the index visit.
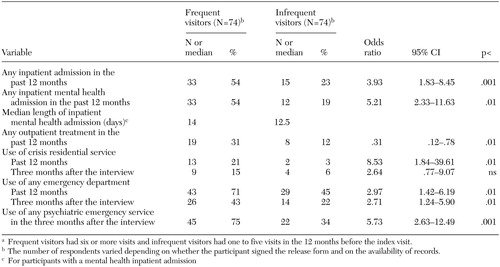 |
Table 3. Health service utilization of frequent and infrequent visitors to a psychiatric emergency servicea
a Frequent visitors had six or more visits and infrequent visitors had one to five visits in the 12 months before the index visit.
1. Bassuk E, Gerson S: Chronic crisis patients: a discrete clinical group. American Journal of Psychiatry 137:1513–1517, 1980Link, Google Scholar
2. Breslow RE, Erickson BJ, Cavanaugh KC: The psychiatric emergency service: where we've been and where we're going. Psychiatric Quarterly 71:101–121, 2000Crossref, Medline, Google Scholar
3. Huffine CL, Craig TJ: Social factors in the utilization of an urban psychiatric emergency service. Archives of General Psychiatry 30:249–255, 1974Crossref, Medline, Google Scholar
4. Morgan SL: Families' experiences in psychiatric emergencies. Hospital and Community Psychiatry 40:1265–1269, 1989Abstract, Google Scholar
5. Arfken CL, Lackman-Zeman L, Yeager L, et al: Frequent visitors to psychiatric emergency services: staff attitudes and temporal patterns. Journal of Behavioral Health Services and Research 29:490–496, 2002Crossref, Medline, Google Scholar
6. Ellison JM, Blum N, Barsky AJ: Repeat visitors in the psychiatric emergency service: a critical review of the data. Hospital and Community Psychiatry 37:37–41, 1986Abstract, Google Scholar
7. Slaby AE, Perry PL: Use and abuse of psychiatric emergency services. International Journal of Psychiatry in Medicine 10:1–8, 1980Crossref, Medline, Google Scholar
8. Purdie FR, Honigman B, Rosen P: The chronic emergency department patient. Annals of Emergency Medicine 10:298–301, 1981Crossref, Medline, Google Scholar
9. Munves PI, Trimboli F, North AJ: A study of repeat visits to a psychiatric emergency room. Hospital and Community Psychiatry 34:634–638, 1983Abstract, Google Scholar
10. Ellison JM, Blum NR, Barsky AJ: Frequent repeaters in a psychiatric emergency service. Hospital and Community Psychiatry 40:958–960, 1989Abstract, Google Scholar
11. Hansen TE, Elliott KD: Frequent psychiatric visitors to a Veterans Affairs medical center emergency care unit. Hospital and Community Psychiatry 44:372–375, 1993Abstract, Google Scholar
12. Klinkenberg WD, Calsyn RJ: The moderating effects of race on return visits to the psychiatric emergency room. Psychiatric Services 48:942–945, 1997Link, Google Scholar
13. Spooren DJ, de Bacquer D, van Heeringen K, et al: Repeated psychiatric referrals to Belgian emergency departments: a survival analysis of the time interval between first and second episodes. European Journal of Emergency Medicine 4:61–67, 1997Crossref, Medline, Google Scholar
14. Dhossche DM, Ghani SO: A study on recidivism in the psychiatric emergency room. Annals of Clinical Psychiatry 10:59–67, 1998Crossref, Medline, Google Scholar
15. Saarento O, Hakko H, Joukamaa M: Repeated use of psychiatric emergency outpatient services among new patients: a 3-year follow-up study. Acta Psychiatrica Scandinavica 98:276–282, 1998Crossref, Medline, Google Scholar
16. Gilfillan S, Claassen CA, Orsulak P, et al: A comparison of psychotic and nonpsychotic substance users in the psychiatric emergency room. Psychiatric Services 49:825–828, 1998Link, Google Scholar
17. Goldfinger SM, Hopkin JT, Surer RW: Treatment resisters or system resisters? Toward a better service system for acute care recidivists. New Directions for Mental Health Services, no 21:17–27, 1984Google Scholar
18. tein LI, Test MA: Alternative to mental hospital treatment, I: conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry 37:392–397, 1980Crossref, Medline, Google Scholar
19. Shaner A, Eckman TA, Roberts LJ, et al: Disability income, cocaine use, and repeated hospitalization among schizophrenic cocaine abusers—a government-sponsored revolving door? New England Journal of Medicine 333:777–783, 1995Google Scholar
20. Wechsler D: Wechsler Adult Intelligence Test-Third Edition. San Antonio, Tex, Psychological Corporation, 1997Google Scholar
21. Eisen SV, Dill DL, Grob MC: Reliability and validity of a brief patient-report instrument for psychiatric outcome evaluation. Hospital and Community Psychiatry 45:242–247, 1994Abstract, Google Scholar
22. Tessler R, Gamache G: Continuity of care, residence, and family burden in Ohio. Milbank Quarterly 72:149–169, 1994Crossref, Medline, Google Scholar
23. Currier GW, Allen M: Organization and function of academic psychiatric emergency services. General Hospital Psychiatry 25:124–129, 2003Crossref, Medline, Google Scholar
24. Hornstra RK, Bruce-Wolfe V, Sagduyu K, et al: The effect of intensive case management on hospitalization of patients with schizophrenia. Hospital and Community Psychiatry 44:844–847, 1993Abstract, Google Scholar
25. Schiller MJ, Shumway M, Batki SL: Patterns of substance use among patients in an urban psychiatric emergency service. Psychiatric Services 51:113–115, 2000Link, Google Scholar



